Generics and public health - WHO archives
advertisement

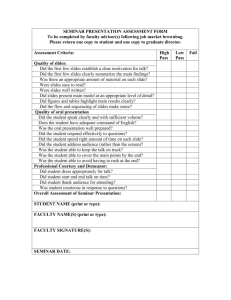
Generics and public health Andrew Creese - Valerio Reggi Department of Essential Drugs and Medicines Policy - EDM Health Technology and Pharmaceuticals Cluster World Health Organization May 2002 Definitions Generics are pharmaceutical products that contain well-established drugs. They are: intended to be interchangeable with the original product, usually manufactured without a licence from the original manufacturer, marketed after the expiry of patent or other exclusivity rights, marketed either under a non-proprietary name (INN or other approved name) or under brand names ("branded generics"). 2 PAR Seminar October 2002 WHO - EDM The worldwide role of generic pharmaceuticals Public health need National strategies Social responsibility 3 PAR Seminar October 2002 WHO - EDM The worldwide role of generic pharmaceuticals Public health need National strategies Social responsibility 4 PAR Seminar October 2002 WHO - EDM Public health need In poor countries drugs are largest household and second largest public expenditure for health Pharmaceutical spending, as % of total health spending Greece Germany Italy France Spain Denmark UK United States Netherlands Norway Developed countries (7 - 20%) Bulgaria Czech Rep. Hungary Croatia Poland Estonia Slovenia Lithuania Transitional countries (15 - 30%) Mali Egypt China Indonesia Thailand Tunisia Jordan Argentina South Africa Developing countries (24 - 66 %) 0 5 PAR Seminar October 2002 10 20 30 40 50 60 WHO - EDM 70 Public health need The cost of medicine is substantial - number of working hours to pay full treatment course 600 500 400 Hours 500 460 And the burden falls heaviest on those least able to pay: Developed countries: 50-90 % publicly funded Developing countries: 50-90 % paid out-of-pocket Tuberculosis 300 200 Shigellosis 120 100 Gonorrhoea 100 100 20 0 Tanzania Zimbabwe 20 20 6 Thailand Based on average worldwide price and national per capita income. Source: WHO/DAP 6 PAR Seminar October 2002 1.4 1.4 0.4 Switzerland WHO - EDM Public health need Despite the potential health impact and expenditure, too many people still lack access to essential drugs >1/3 of world’s population lacks regular access 320 million in Africa have <50% Problem worsens with economic pressures Percentage of populations and number of countries with regular access to essential drugs: 1 = <50% 2 = 50-80% 3 = 80-95% 4 = >95% 5 = No data available 7 PAR Seminar October 2002 (43) (64) (30) (41) (1) WHO - EDM Public health need Millions of children and adults still die from diseases readily treated with generic essential drugs Developing Country Deaths (millions) 1990 INFECTIOUS & PARASITIC DISEASES Respiratory infections Age 5 & over Under 5 Diarrhoeal disease Tuberculosis Measles Malaria Tetanus Pertussis HIV Meningitis NON-COMMUNICABLE DISEASES - A GROWING CHALLENGE Heart attacks, strokes Cancer 0 8 PAR Seminar October 2002 1 2 3 4 5 WHO - EDM 6 The worldwide role of generic pharmaceuticals Public health need National strategies Social responsibility 9 PAR Seminar October 2002 WHO - EDM National strategies As of the mid-1990’s, few countries had achieved large generic coverage D E V E LO P E D C O UN T R IE S D e nm a rk Unit e d S t a t e s Unit e d Kingdo m G e rm a ny N e t he rla nds Ire la nd P o rt uga l N e w Z e a la nd J a pa n F ra nc e S pa in D E V E LO P IN G C O UN T R IE S Indo ne s ia M o ro c c o P hilippine s 0 10 20 30 40 50 60 % prescriptions generic Source: DAP Global comparative pharmaceutical expenditures and IGPA 10 PAR Seminar October 2002 WHO - EDM 70 National strategies Price differentials between generic and brand products vary greatly among countries Belgium Italy Spain Germany France Canada UK US 20% 20% + 25% 25% - 30% 25% - 35% 40% - 50% 80% + 50% - 90% Source: IMS, Pharma Strategy Group 11 PAR Seminar October 2002 WHO - EDM National strategies Drug sales 1990 and 2000: originator and licensed products grew from 50% to 64% of world market value 300 250 market value in US $ billion 102,3 200 Other 150 100 64,2 50 63,5 180,2 Originator 0 1990 2000 Source: IMS Health, customised study. Data from 52 countries/areas 12 PAR Seminar October 2002 WHO - EDM National strategies Drug sales 1990 and 2000: market share of originator and licensed products in high, middle and low income country markets 70 60 50 % of market by value High (25) Middle (23) Low (4) 40 30 20 10 0 1990 2000 Source: IMS Health, customised study. Data from 52 countries/areas 13 PAR Seminar October 2002 WHO - EDM National strategies Drug sales 1990 and 2000: originator and licensed products in high, middle and low income country markets market value in US $ billion 180 160 140 120 100 80 60 40 20 0 168 High (25) Middle (23) Low (4) 59 40,5 1990 12 0,6 2000 Source: IMS Health, customised study. Data from 52 countries/areas 14 PAR Seminar October 2002 WHO - EDM National strategies Rapidly changing drugs markets Czech Republic*, 1990 and 2000 100% 19,7 90% 80% 15,5 70% 8,5 44,6 60% 50% 48,6 40% 39,8 30% 20% 16,2 10% 0% 1990 Unbranded 7,1 2000 Other brands Origin/licensed status n/a *2000 Population: 10.3 million Source: IMS Health, customised study. Data from 52 countries/areas 15 PAR Seminar October 2002 WHO - EDM What are the potential benefits of generics? Better access to needed medicines. Well chosen generics make government or household spend less without loss of quality or safety 1998 study by US Congressional Budget Office: average generic medicine prescription price was less than one third of average price of single-source innovator brand drug 16 PAR Seminar October 2002 WHO - EDM What are the potential benefits of generics? Impact on the price of non-generics through competition: generics may be the only way to bring price competition to a market that is based on product differentiation, patent protection and heavy brand promotion to both prescribers and patients access to needed medicines. 17 PAR Seminar October 2002 WHO - EDM Why are generics less expensive? Not because they are inherently different in composition from patented drugs, but mainly because of the structure of the generics market: competitive, free from IPRs, often without the R&D and particularly the marketing cost that goes into branded proprietary drugs 18 PAR Seminar October 2002 WHO - EDM National strategies Building a large generic market takes time - and requires a combination of strategies National strategies for generics: 50 45 40 35 30 25 20 15 10 5 0 5 8 19 19 PAR Seminar October 2002 1. 2. 3. 4. Supportive legislation & regulation Reliable quality assurance Professional, public acceptance Economic incentives Percent of new prescriptions, U.S. 6 8 19 7 8 19 8 8 19 9 8 19 0 9 19 1 9 19 2 9 19 * 3 4 9 9 9 19 1 WHO - EDM National strategies 1. Supportive legislation and regulation product development authorized during patent life abbreviated marketing authorization differential registration fees generic labeling generic prescribing and substitution 20 PAR Seminar October 2002 WHO - EDM National strategies Product development during patent period varies among countries Examples of “early workings” for generics access to innovator product safety and efficacy data production tests on a patent-protected product laboratory tests for marketing approval – e.g. bioequivalence production and stockpiling prior to patent expiry Countries with some early workings provisions Argentina Australia Canada 21 PAR Seminar October 2002 Hungary Tunisia USA WHO - EDM National strategies 2. Reliable quality substitution / non-substitution lists national regulatory capacity enforcement of good manufacturing practices (GMP) distribution system inspection and enforcement GMP 22 PAR Seminar October 2002 WHO - EDM Drug registration Requirements for abridged marketing authorization application (i.e. without pre-clinical and clinical data) product information previously approved, active ingredient previously approved, route of administration, strength and dosage form equal to those of previously approved product, adequate information on analytical methods, manufacturing process, manufacturers of finished product and starting materials, stability studies, proof of therapeutic equivalence with previously approved product. 23 PAR Seminar October 2002 WHO - EDM Drug registration Definitions (1) Pharmaceutical equivalents: Products that contain the same amount of the same active substance(s) in the same dosage form; meet the same or comparable standards; are intended to be administered by the same route. Pharmaceutical equivalence does not necessarily imply therapeutic equivalence as differences in excipients and/or manufacturing process can lead to differences in product performance. 24 PAR Seminar October 2002 WHO - EDM Drug registration Definitions (2) Generic (multi-source): pharmaceutical equivalent of a non-patentprotected product (comparator product) whose safety and efficacy are well established; can be marketed under its INN or a brand name; may or may not be interchangeable with its comparator product. 25 PAR Seminar October 2002 WHO - EDM Drug registration Definitions (3) Comparator product: • • • 26 PAR Seminar October 2002 product with which a generic is expected to be interchangeable; product whose safety and efficacy studies are well established and will be the basis for approval of all its pharmaceutical equivalents; product that often has the largest market share. WHO - EDM Drug registration Definitions (4) Therapeutic equivalents: pharmaceutical equivalents whose bioavailability or dissolution profiles, after the same molar dosis, are similar to such an extent that their safety and efficacy can be assumed to be substantially equal. Therapeutic equivalents are interchangeable. 27 PAR Seminar October 2002 WHO - EDM Drug registration Therapeutic equivalence Depending on active ingredient and formulation: 28 PAR Seminar October 2002 dissolution (in vitro) bioequivalence studies (in vivo) pharmacodynamic studies (in vivo) clinical trials (in vivo) WHO - EDM Drug registration Active ingredient and formulation characteristics affecting dissolution/absorption Particle size: digoxine, griseofulvine, nitrofurantoin Crystal form (different forms with equal internal structure, different internal structures, solvates) : riboflavine, cimetidine, erithromycine, clortalidon, chloramfenicol, cefalexine Wettability: phenytoin Dependence on pH: aspirin, ketoconazol, sulfonamides Excipients: nystatin, sulfadimidine with PVP or gelatin, phenytoin with con lactose 29 PAR Seminar October 2002 WHO - EDM Drug registration Examples of drug with high first-pass metabolism Alprenolol Amitriptyline Chlormethiazole Desipramine Dextropropoxyphene Dihydroergotamine Diltiazem 5-Fluorouracil Hydralazine Isoproterenol Labetolol Testosterone Lidocaine Methylphenidate Morphine Neostigmine Nifedipine Nitroglycerin Papaverine Pentazocine Phenacetin Propranolol Salicylamide Verapamil FA= 0.5 or less. From: Pond, S.M. and Tozer, T.N. : First-pass elimination. Basic concepts and clinical consequences. Clin Pharmacokinetics 1984; 9:1-25 30 PAR Seminar October 2002 WHO - EDM Drug registration Examples of drugs with “possible” BA/BE problems (104 substances) Acebutolol Amiodarone Bromocryptine Cefalexin Chlorpropamide Cyclophosphamide Digitoxin Droperidol Ethinylestradiol Fluocortolone Flutamide Haloperidol Labetalol Medroxyprogesterone Methylprednisolone Nifedipine Oxprenolol Procainamide Temazepam Thyroglobulin Trifluoperazine Acetohexamide Amitryptyline Busulfan Cefazolin Clomifene Cyproterone Digoxin Dydrogesterone Ethosuximide Fluoxymesterone Glibenclamide Hydrocortisone Levothyroxine Mesterolone Metoprolol Nitrendipine Perphenazine Propranolol Terazosin Tocainide Valproate Ajmaline Atenolol Butriptyline Chlorambucil Clonazepam Deslanoside Diltiazem Enalapril Ethylestrenol Flupentixol Gliclazide Imipramine Liothyronine Metformin Midazolam Nitroglycerin Phenytoin Pyrazinamide Testosterone Tolbutamide Verapamil Alprenolol Betamethasone Captopril Chloramphenicol Clonidene Dexamethasone Disopyramide Epinephrine Felodipine Fluphenazine Glipizide Isosorb.-5-mononitrate Lithium Carb. Methotrexate Nadolol Norethisterone Pindolol Quinidine Theophylline Triamcinolone Warfarin Aminophylline Bevantolol Carbamazepine Chlorpromazine Conjugated Estrogens Diethylstilbestrol Dosulepin Erythromycin Flecainide Flurazepam Guanfacine Isosorbide dinitrate Magnesium sulfate Methylergometrine Nicardipine Oxandrolone Prazosin Rifampicin Thioridazine Triazolam Sources: too many to list 31 PAR Seminar October 2002 WHO - EDM Drug registration ¿In vitro or in vivo? (1) Different criteria exist: US-FDA: WHO : MULTI-SOURCE PHARMACEUTICAL PRODUCTS, WHO GUIDELINE ON REGISTRATION REQUIREMENTS TO ESTABLISH INTERCHANGEABILITY, 1996 Http://www.fda.gov EU: Http://www.eudra.org 32 PAR Seminar October 2002 WHO - EDM Drug registration ¿In vitro or in vivo? (2) US-FDA’s Biopharmaceutic Classification System In vivo BE waiver based on solubility and permeability Peff = Qin (Cin – Cout) / Cout * 2rl Unfortunately, permeability is not easy to measure and published data are scarce Waiver probably never used in practice 33 PAR Seminar October 2002 WHO - EDM Drug registration Bioequivalence (1) Compare two formulations to determine whether they provide substantially the same amount of active substance at a comparable rate. It is applied for authorizing : - ‘scaling up’ - post-approval changes - generics Almost no product is marketed in the same formulation used in phase I, II, and III clinical trials. 34 PAR Seminar October 2002 WHO - EDM Drug registration Bioequivalence (2) Design: 12-36 healthy volunteers (males, age 18-36) possible effects of disease/age/sex assumed identical for the 2 formulations each volunteer receives at least one dose of each formulation after suitable washout period Specific designs (~100 FDA, USP) 35 PAR Seminar October 2002 WHO - EDM Drug registration Bioequivalence (3) 3 bioavailability parameters (including active metabolites if applicable): 36 PAR Seminar October 2002 WHO - EDM Drug registration Bioequivalence (4) Evaluation: •AUC: •90% CI of ratio of average AUC of the 2 products (both directions), • 90% confidence interval should generally be within 80 to 125% (EEUU, UE, Canadá, Australia) •Cmax: wider acceptance criteria •Tmax: considered only when clinically relevant 37 PAR Seminar October 2002 WHO - EDM Drug registration Bioequivalence (5) 1962: FDA establishes BE requirement, implementation ‘from now on’, AUC and Cmax of TD/RD must be between +/-20% in majority of subjects 1977: 75/75-125: 75% of subjects must fall within 75-125% 1979: First Orange Book 1991: 90%CI must fall within 0.80-1.25 1999: Biopharmaceutics Classification System - BE waiver in selected cases. 38 PAR Seminar October 2002 WHO - EDM Drug registration Bioequivalence (6) Practical implementation of BE study requirement: manufacturer selects one batch for BE study and study for submission, after approval, only dissolution is used for following batch releases and lower limits are based on BE batch data (i.e. data of one single batch). 39 PAR Seminar October 2002 WHO - EDM Drug registration Bioequivalence (7) Implementation seems good enough because: reports of clinical failures due to BA/BE problems are anecdotal US-FDA claims “there are no documented examples of generic products manufactured to meet approved specifications that could not be used interchangeably with the corresponding brand-name drug” http://www.fda.gov/cder/news/nightgenlett.htm Innovative industry and patients’ associations in US claim that no documented cases of “patient-formulation” interaction exist FDA hearing 23 September 1999 40 PAR Seminar October 2002 WHO - EDM Drug registration Bioequivalence (8) Other elements to consider: - apparently-identical drugs of the same brand but manufactured and marketed in different countries are not necessarily bioequivalent - transitive property of bioequivalence (different formulations of same product or different products) - change in labelling resulted in reports of 20% ‘therapeutic failures’ (Glaxo, 1990) - superbioavailability reformulation (first always best?) - WHO guidelines on interchangeability and comparator product 41 PAR Seminar October 2002 WHO - EDM Drug registration WHO Guidelines What are the practical implications of requiring new BE studies in each country even for drugs from reliable source meant for use in non-chronic courses? MULTI-SOURCE PHARMACEUTICAL PRODUCTS, WHO GUIDELINE ON REGISTRATION REQUIREMENTS TO ESTABLISH INTERCHANGEABILITY, 1996 42 PAR Seminar October 2002 Selection of Comparator Pharmaceutical Product for Equivalence Assessment of Interchangeable Multi-source (Generic) Products,WHO, 1999 WHO - EDM How to Identify Comparator Pharmaceutical Product: Decision Tree Comparator Pharmaceutical Product (CPP) Quality/Safety/Efficacy known Innovator known Yes No Available on local market Yes Present on List B No Consider Innovator as CPP Consider obtaining Innovator: List A Innovator available Yes Consider Innovator as CPP No Consider Market Leader Yes No Follow compendial standards approach Consider Market Leader Quality of Market Leader known and well-documented Yes Consider Market Leader as CPP No Conduct comparative compendial tests between Multi-source and Market Leader Acceptable test results Yes No Consider Market Leader as CPP 43 PAR Seminar October 2002 Consider 2nd Market Leader WHO - EDM Drug registration Some ‘free’ considerations on BE BE is a scientifically sound concept that has been applied with varying criteria in different regulatory systems over the last 38 years at the same time, industry has mainly used dissolution as an indicator of uniformity of biopharmaceutical characteristics of products at lot release during all this time, reports of ‘therapeutic failures’ have been scarce it is likely that implementation of strict BE requirements is not high priority for countries that do not fully assess the quality part of MA applications, have no full market control, cannot ensure GMP compliance, and cannot monitor raw materials 44 PAR Seminar October 2002 WHO - EDM National strategies 3. Professional and public acceptance 45 PAR Seminar October 2002 involvement of professional groups phased implementation all training by generic name use of generic names in clinical manuals brand-generic / generic-brand indexes public promotional information and activities WHO - EDM National strategies Stages in Generic Substitution - legislative support for generic substitution may evolve over time 1. No substitution 2. Substitution permitted brand dispensing assumed generic may be requested 3. Substitution encouraged generic dispensing assumed brand may be requested 4. Substitution required Increasing generic support 46 PAR Seminar October 2002 WHO - EDM National strategies Generic substitution laws can give each party a voice Regulatory authority Prescriber write ‘no substitution’ by hand on the prescription Pharmacist - must substitute a generic unless: declare products as ‘substitutable’ or ‘non-substitutable’ prescriber or patient forbid substitution retail price of generic is higher than the brand product has been declared not substitutable Patient may forbid generic substitution 47 PAR Seminar October 2002 WHO - EDM National strategies Pocket manuals put generic names and brand-generic lists at health professionals’ figure-tips 100+ countries have treatment guidelines, formularies 48 PAR Seminar October 2002 WHO - EDM National strategies Public education campaigns help professional and public acceptance to reinforce each other Posters and brochures Radio and TV messages Other media 49 PAR Seminar October 2002 WHO - EDM National strategies 4. Economic incentives price information for professionals and the public retail margins favorable to generics use of generics for insurers / reimbursement development of generic industry 50 PAR Seminar October 2002 WHO - EDM National strategies Price information - enlightens health professionals and empowers consumers relative / absolute price information in clinical manuals drug pricing guide publication of pricing surveys Using ATC/DDD-based system to compare prices (e.g. Italy, Netherlands, Tunisia) 51 PAR Seminar October 2002 WHO - EDM National strategies Different types of dispensing margins create different incentives for rational dispensing Cost + fixed percentage Cost + declining percentage e.g.: cost + 20% for cheaper drugs, declining to 5% for expensive drugs Cost + fixed professional fee e.g.: cost to pharmacist + 20 % e.g.: cost + $3 professional dispensing fee Cost + differential professional fee 52 PAR Seminar October 2002 e.g.: cost + $4 for generics, $2 for brand name drugs WHO - EDM National strategies Insurance coverage is everywhere rising - generic essential drugs are needed for cost control Established Market6 Economies Middle Eastern Crescent 5 4 Transitional Economies Latin Americas & Caribbean 3 Asia & Islands 2 1 Sub-Saharan Africa 0 0 10 20 30 40 50 60 70 80 Percentage coverage of population Each diamond represents % of population covered in one country Source: WHO/DAP Global pharmaceutical expenditures 53 PAR Seminar October 2002 WHO - EDM 90 100 National strategies WHO supports generic drug use through a variety of efforts - some examples Normative support Generically-oriented drug information model list of essential drugs model prescribing information model formulary of essential drugs Regulatory support 54 PAR Seminar October 2002 International Non-propriety Names (INN) International Pharmacopoeia manual on marketing authorization support to national regulatory authorities WHO - EDM The worldwide role of generic pharmaceuticals Public health need National Strategies Social responsibility 55 PAR Seminar October 2002 WHO - EDM Social responsibility Generic pharmaceutical manufacturers and distributors also have a social responsibility priority on essential generic drugs adherence to WHO ethical criteria for drug promotion help to assure supply of “abandoned” essential drugs ether for anesthesia oxaminiquine, metrifonate for schistosomiasis suramin sodium, pentamidine isethionate for African trypanosomiasis 56 PAR Seminar October 2002 WHO - EDM Conclusions Generics can play an important role in public health This role can be optimized through: - supportive legislation and regulations capable and credible regulatory authorities favorable economic environment information and advocacy initiatives Professional and public acceptance 57 PAR Seminar October 2002 WHO - EDM