Oral Complications
advertisement

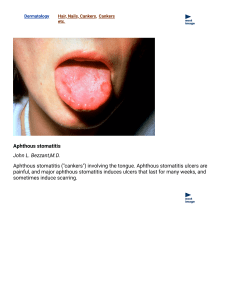
chemotherapy (CT) radiation therapy (RT), hematopoietic stem cell transplantation (HSCT) 1. 2. 3. 4. 5. CT- and RT-related stomatitis oropharyngeal pain xerostomia oral infection oral chronic graft-versus-host disease (cGVHD). Stomatitis is an inflammation of the mucous membranes of the oral cavity and oropharynx characterized by tissue erythema, edema, and atrophy, often progressing to ulceration. The clinical significance of CT- and RTrelated stomatitis as a dose- and treatmentlimiting side effect is well appreciated. PATIENT-RELATED Age older than 65 y or younger than 20 y Gender Inadequate oral health and hygiene practices Periodontal diseases Microbial flora Chronic low-grade mouth infections Salivary gland secretory dysfunction Herpes simplex virus infection Inborn inability to metabolize chemotherapeutic agents effectively Inadequate nutritional status Exposure to oral stressors including alcohol and smoking Ill-fitting dental prostheses TREATMENT-RELATED Radiation therapy: dose, schedule Chemotherapy: agent; dose, schedule Myelosuppression Neutropenia Immunosuppression Reduced secretory immunoglobulin A Inadequate oral care during treatment Infections of bacterial, viral, fungal origin Use of antidepressants, opiates, antihypertensives, antihistamines, diuretics, and sedatives Impairment of renal and/or hepatic function Protein or calorie malnutrition, and dehydration Xerostomia Risk factors for CT-related stomatitis are complex, and study results are conflicting. continuous CT infusion therapy for breast and colon cancer [5-FU and leucovorin ] selected anthracyclines alkylating agents taxanes vinca alkaloids Antimetabolites antitumor antibiotics myeloablative conditioning regimens for HSCT; RT to the head and neck. Children are 3 times more likely than adults to develop stomatitis because of a higher proliferating fraction of basal cells. Individual drug metabolism affects stomatitis incidence and severity, as seen with patients who are unable to adequately metabolize certain CT 40% of CT patients develop stomatitis, Half requiring parenteral analgesia that may lead to treatment modification. 60% are seen in the HSCT setting, Oral infection, herpes simplex virus (HSV) in particular, may increase stomatitis severity a 4 times greater relative risk of septicemia asymptomatic erythema and progresses from solitary, white, elevated desquamative patches that are slightly painful to large, contiguous, pseudomembranous, painful lesions. Area Type of ionizing radiation volume of irradiated tissue daily and cumulative dose duration of RT Stomatitis is a dose- and rate-limiting toxicity of RT for head and neck cancer, and of hyperfractionated RT and CT that is designed to improve survival time. COX-2 plays an amplifying role in RT-related stomatitis. Atrophic changes in the oral epithelium usually occur at total doses of 1,600 to 2,200 cGy, administered at a rate of 200 cGy per day. Doses higher than 6,000 cGy place the patient at risk for permanent changes in the salivary glands. depend primarily on salivary changes rather than on direct irradiation of the teeth. Direct irradiation of teeth may alter the organic or inorganic components making them more susceptible to decalcification or hypocalcification. daily fluoride application is necessary Long-term effects of head and neck RT 1. Soft tissue fibrosis 2. Obliterative endoarteritis 3. Trismus 4. Nonhealing or slow-healing mucosal ulcerations 5. slow healing of dental extraction sites. RT-induced fibrotic changes up to 1 year post-therapy, becoming more serious over time. Higher incidences are seen after total doses to the bone exceed 65 Gy. The risk of ORN actually increases over time following RT. pathologic fracture, infection of surrounding soft tissues, and severe pain. time to allow adequate extraction site healing is 10 to 14 days before start of RT. Long use :bisphosphonate therapy majority required surgical procedures to remove the involved bone. Oral candidiasis angular cheilitis, may appear as white and removable chronic hyperplastic (nonremovable) chronic erythematous (diffuse patchy erythema). Acute GVHD occurs within the first 100 days after allogeneic HSCT. Chronic GVHD begins as early as 70 days or as late as 15 months after allogeneic transplant. 80% of patients with extensive cGVHD have some type of oral involvement Oral infection in cGVHD patients is a risk factor for systemic infections that are the primary cause of death in this population stomatitis-related pain Immunocompromised cancer patients with HSV infections have larger, more painful lesions as compared with noncancer patients cGVHD The effect on the patient's psychological well-being: medication usage, decreased oral intake use of analgesics and opioids. individual's thought process, self-perception, reported pain relief, the personal meaning of the pain. The sociocultural dimension includes demographic characteristics, cultural background, and family and work roles. age and pain perception, intraethnic differences in pain perception Gender Pain control is critical to accomplish to avoid suffering and psychological distress. Effective oral pain management is promoted through open, consistent communication between and among patient, physician, nurse, and caregiver. A comprehensive pain assessment tool? Xerostomia Severity dependent on the radiation dosage and location, and volume of exposed salivary glands. Significant xerostomia has not been reported in patients treated with CT alone. Xerostomia can affect oral comfort, fit of prostheses, speech, and swallowing. Xerostomia-associated enzymes contribute to the growth of caries (decay)-producing organisms, and the decrease in quantity and quality of saliva can be very harmful to dentition Pretherapy Dental Evaluation and Intervention Assessment of the Oral Mucosa an experienced dental team Many health care institution-specific policies and preventive approaches exist for oral care for CT and RT patients. dental screening at least 2 weeks before therapy Oral hygiene related to several important factors, including radiation exposure , type, portal field, fractionization, total dosage tumor prognosis, expediency of control of the cancer. Careful examination of extraction sites must be performed before RT commences. Dental extractions following RT require collaborations between dental and radiation oncology team members to minimize the risk of ORN. A low incidence of ORN is seen when pre-RT dental consultation and appropriate treatment (e.g., extractions) are rendered. Follow-up Assessment of the Oral Mucosa The optimal treatment ? mainly empirical The only standard forms of care are pretreatment oral/dental stabilization, saline mouthwashes, and oropharyngeal pain management. oral hygiene unreliable evidence for the effectiveness of 1. allopurinol mouthwash, 2. vitamin E, 3. immunoglobulin, 4. human placental extract no single agent completely prevented stomatitis, suggesting that combined strategies may be necessary A standardized approach for the prevention and treatment of CT- and RT-induced stomatitis is essential. Chlorhexidine gluconate (Peridex), Saline rinses, Sodium bicarbonate rinses, Acyclovir Amphotericin B Ice a local anesthetic such as lidocaine or dyclonine hydrochloride, magnesium-based antacids (Maalox, Mylanta), diphenhydramine hydrochloride (Benadryl), nystatin, or sucralfate These agents are used either alone or in various combinations as a mouthwash formulation. opioids used less commonly include kaolin-pectin (Kaopectate), allopurinol, vitamin E, betacarotene, chamomile (Kamillosan) liquid, aspirin, antiprostaglandins, prostaglandins, MGI 209 (marketed as Oratect Gel), silver nitrate, and antibiotics has shown efficacy in the treatment of gastrointestinal (GI) ulceration has been tested as a mouthwash for the prevention and treatment of stomatitis? CT? Sucralfate has also been tested in the head and neck RT population? Gelclair is a concentrated, bioadherent gel that has received for the management of stomatitis-related oral pain. Benzydamine is a nonsteroidal antiinflammatory drug with reported analgesic, anesthetic, anti-inflammatory, and antimicrobial properties. بتامتازون +اب هیدروکورتیزون +نیستاتین +تتراسایکلین +دیفن هیدرامین Vitamin E + vitamins C and E and glutathione ? Azelastine may be useful to prevent CTinduced stomatitis Silver Nitrate + Laser? Miscellaneous Agents? diphenhydramine hydrochlor-ide (Benadryl), saline, sodium bicarbonate, and gentian violet Cryotherapy used to induce vasoconstriction should be considered for patients receiving 5-FU or melphalan when these agents are administered during short infusion times. Hematopoietic Growth Factors? Keratinocyte Growth Factors Antimicrobials Pharmacologic Modulation Recently, palifermin, which is a recombinant human keratinocyte growth factor, has shown efficacy in the reduction of oral mucosal injury related to cytotoxic therapy Treatment approaches for oral candidiasis include Mycostatin (troches), nystatin (liquid or ointment), or clotrimazole. Pseudomembranous candidiasis is successfully treated topically. Chronic candidiases usually requires much longer treatment, and it may be necessary to use oral ketoconazole, fluconazole, or intravenous amphotericin B. chlorhexidine mouthwash ? Allopurinol mouthwash for the prevention and treatment of 5-FU-related stomatitis positive results have led to allopurinol becoming routine practice. no protective effect of allopurinol against 5FU-induced stomatitis was seen in a randomized, double-blind clinical trial conducted by the NCCTG and the Mayo Clinic. RT-induced fibrosis of the masticatory muscles and/or the temporal mandibular joint may be prevented or attenuated through early exercises with trismus appliances posttherapy. Fibrosis of the masticatory muscles may occur up to 1 year postradiation; therefore, jaw-opening exercises should start after oral mucosal healing and continue for more than 1 year following RT. Effective exercises in reducing trismus include the use of tongue depressors taped together 10 to 15 times a day for 10-minute sets. 1. 2. Antibiotics and surgical debridement and curettage. Hyperbaric oxygen ? conservative debridement and antibiotic therapy. surgical procedures to remove the involved bone. Early diagnosis pretherapy dental care Stomatitis is the principal etiology of most pain experienced during the 3-week post-BMT time period. Stomatitis-related oropharyngeal pain is multidimensional. Immunocompromised patients with cancer who are also HIV develop larger, more painful lesions Oral pain associated with cGVHD has been described as severe, with symptoms of burning, irritation, dryness, and loss of taste has been reported. viscous lidocaine (Xylocaine) or dyclonine hydrochloride temporary pain relief kaolin-pectin, diphenhydramine, Orabase, and Oratect Gel. One large clinical research center uses a topical formulation that contains lidocaine viscous 2% (40 mL), diphenhydramine 12.5 mg/5mL (40 mL), and Maalox 10 mg (40 mL) and prescribes its use every 3 to 4 hours as needed. Severe stomatitis-related oropharyngeal pain may interfere with hydration and nutritional intake and affect quality of life. Management of this oropharyngeal pain may require use of opioids, oral transmucosal fentanyl was more effective than morphine sulfate immediate release in treating breakthrough pain At present, no standard treatment has been defined for the prevention or treatment of stomatitis-related oral pain; therefore, it is essential to continue studies of the treatments already available and to develop promising new approaches. Oral hygiene regimens that include the use of water/saline and daily fluoride application along with brushing teeth at least 3 times daily may reduce colonization and proliferation of oral pathogens. pilocarpine, 5- and 10-mg doses amifostine (Ethyol), administered at 200 mg/m2 as a 3-minute intravenous infusion 15 to 30 minutes before each fraction of radiation. Artificial saliva, which usually uses carboxymethylcellulose as a base? sugarless gum and hard candy Conclusion