Powerpoint
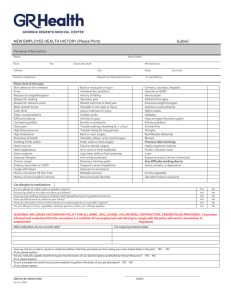
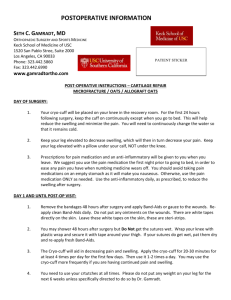
advertisement

Reasons for deciding to have Joint Replacement Improve quality of living Tired of living in pain Not being able to do things you like to do NORMAL AND ABNORMAL XRAYS Preoperative testing Need clearance from Primary Care Physician They will send you for blood work, EKG, CXR, urinalysis, and sometimes other tests Must be within 30 day window of surgery date Some of you will be asked to donate your own blood- GBMC’s Blood Donor Room phone # 443-849-2817. Call for an appointment. 10 days before surgery-page 24 Stop taking Aleve, Ibuprofen, Motrin, Advil, Aspirin products. Tylenol is okay to continue using Stop taking Vitamin E Stop taking herbal products If taking Coumadin, Plavix, or other blood thinners, talk to your prescribing physician about what to do with these medications 24 hours before surgery If you are taking Avandamet, Actoplus, Glucophage, Metforman, or Glucovance – STOP TAKING 24 HOURS BEFORE SURGERY! These medications can cause your surgery to be cancelled if taken within this time period. If you are on insulin, talk to your prescribing physician about how many units they want you to take the evening before surgery Night before surgery NPO after midnight – no eating or drinking except in the morning you may take your blood pressure, or cardiac medications with a sip of water (if instructed to do so by your physician) If you keep a drink on your bedside table, remove it before you go to sleep. Old habits are hard to break! No chewing gum or mints Morning of Surgery Blood pressure/Cardiac medication- Talk to your primary care or cardiologist to discuss which medications you should take in the morning of your surgery. Typically, they will get you to take them with a sip of water depending on the medication. Heartburn or ulcer medicine- acid blockers (Zantac, Pepcid, Axid, Prilosec, Propulsid, Reglan) should be taken on the morning of the surgery to reduce the risk of aspiration pneumonia. Antacids like Maalox, Tums, or Carafate should NOT be taken because they contain particulate material that may damage the lungs if aspirated. Day of Surgery Bring with you to the hospital – anything your surgeon has asked for you to bring, medication list, green blood donation cards (if donated blood) Be at the hospital 2 hours before your surgery time Follow directions on the purple hand-out in your packet to admitting area Pre-op area Turn in the paperwork that you brought with you You will be given a hospital gown to change into Meet your surgical team – surgeon, nurse, anestheologist, tech Many questions will be asked – “Do you know why you are here?” Don’t panic, they do know. They want to make sure you are in agreement to what procedure is being done Vital signs and IV will be started Preventing Infections and other complications Control your blood sugar before, during and after your surgery Exercise and healthy weight loss Try to stop smoking Good nutrition with adequate calories and protein Make sure skin is dry in between skin folds Dental Health-make sure you have had a dental examine in the past 6 months Please be sure to keep pets away from the incision site Do not let pets sleep with you after surgery Apply fresh linens to bed before surgery Pre-op skin preparationChlorhexidine gluconate(CHG) Preparing or prepping the skin before your surgery can reduce the risk of infection at the surgical site. GBMC will be providing 3 packs of CHG wipes which you are receiving today in this class. You will start using these wipes the 3 days prior to your surgery. One more CHG bath will be done in the pre-op area the day of surgery. Do not shave legs the 3 days prior to surgery Things not to do Don’t write on extremities – For example – “Wrong leg!” Your surgeon will initial the limb being operated on Types of Anesthesia General Anesthesia Most commonly used Spinal Operating Room Surgery will take approximately 2 to 2-1/2 Bilateral knees will take longer. Recovery Room Wake patient Monitor Vital Signs Control Pain Pain Management One concern patients have is how much discomfort will they have. We use different techniques or modalities to help: PCA pumps Lumbar Plexus nerve blocks for hips Femoral nerve blocks for knees “Cocktail” mixture of pain medication, local anesthetic, and anti-inflammatory injected into the knee Epidural Blocks PCA Pain pump connected to your IV Only patient should push button to receive medication Programmed to only allow a certain amount of medication in a period of time Pain scale 0-10 0 means no pain and 10 the worst pain that you have ever had Stryker Drain A drain that is inserted near your surgical site during surgery to collect bloody drainage. Blood can be re-infused back into your IV within a certain time frame. Decreases swelling at surgical site Equipment used Sequential Compression Device (SCD’s) Ted Stockings Stryker Drain Patient Controlled Analgesia (PCA) Oxygen Foley catheter Abduction Pillow (Hips only) Incentive spirometry AV Boots and TED Stockings Used on your lower extremities to help circulation Help prevent blood clots Abduction Pillow(for hips only) Placed between legs while in bed Hip precautions Don’t cross legs Don’t turn toes inward Don’t bend beyond 90 degrees Don’t twist Incentive Spirometry Exercise your lungs Use 10 x per hour Place mouth on mouthpiece Take a slow, deep breath in and hold for 3 seconds Exhale The Joint and Spine Center Unit 58 Transfer to Unit 58 Private Rooms Dedicated staff Day of Surgery You will probably feel sleepy for most of the day Vital signs checked frequently, every 4 hours Continuous pulse ox placed on finger to monitor your oxygen level Knee Patients Do NOT place a pillow under your knee because it makes it harder to get your knee straight. It may be more comfortable, but you should NOT do this. Day after Surgery POD # 1 Busy Morning Nurse Practitioner will remove Stryker Drain (if used) and change dressing Foley Catheter removed Evaluated by Physical Therapist (P/T) and Occupational Therapist (O/T) PCA will be discontinued and you will be started on oral pain medication PATIENT SAFETY Fall Prevention “Do not get up without the help of staff!” HAVING KNEE OR HIP REPLACEMENT MAKES YOU A FALL RISK SO FOR PATIENT SAFETY…. “Do not get up without the help of staff!” AND Orange or Red non-skid socks will be placed on you when you are admitted to GBMC to signal you are a fall risk. Case Manager The case manager on Unit 58 will come in to visit you to start working on your discharge planning needs. Home Physical Therapy, Out-Patient Physical Therapy or Sub-acute Rehab Order equipment needed for home First Ice Compression Wrap Placed on your operative leg on Unit 58 Decreases pain levels and swelling The ice wrap is purchased for you by The Joint Center Knee Wrap Hip Wrap Afternoon POD # 1 Group Therapy at approximately 2 p.m. in our Clubroom (Coaches should attend if possible) Therapy session lasts about 1 hour Coaches If possible ask a family member or friend to attend the group therapy sessions to help learn and assist you with your exercises. Same day of surgery or POD#1 CPM will be placed on Total Knee Replacements (if ordered) Usually, it will be placed after dinner The goal is to keep it on for at least 2 to 3 hours Ask for pain medication before being placed in CPM Bedside Reporting The nurses do their reporting to the next shift at your bedside. POD # 2 Early rising! To ensure that each patient is ready for physical and occupational therapy, you will be awakened very early (between 5:00 and 5:30 a.m.) by Unit 58 staff Staff will assist you with bathing and getting dressed POD # 2 PT will walk you in the morning individually OT will assist you with ADL’s Group Therapy at approximately 10 am and 2:00 pm POD #2 or POD# 3 Group Therapy in Clubroom at approximately 10 a.m. Plan for discharge by 12-1 p.m. You will receive: Discharge Instructions Paperwork with name of agency providing Home Physical Therapy (if appropriate) Dressing materials and TED stockings Preventing Blood Clots Everyone will be on either Lovenox, Arixtra, Xarelto, Aspirin or Coumadin(Warfarin) to help prevent blood clots. If you are on one of the injectables(lovenox or arixtra), you or a family member will be instructed how to administer it. It is only given in the abdomen. Group Lunch Group lunch is held on Thursdays at approximately 12 noon in the Clubroom. Coaches are welcome. Great way to get camaraderie! Parking Passes See form on Parking in Packet Weekly parking passes available for purchase once you are here for surgery $15.00 weekly pass must be purchased when you are admitted The passes are available from the gift shop What is MOLST Maryland MOLST is a portable medical order form covering options for cardiopulmonary resuscitation and other life-sustaining treatments The medical orders are based on a patient’s wishes about medical treatments The original, copy, or faxed MOLST form are all valid orders MOLST orders are still valid even if written by a practitioner who is NOT on their medical staff MOLST orders do not expire •Who Needs a MOLST FORM MOLST will be necessary for all admitted/observation patients All patients that are transferred to another facility will also require a MOLST form prior to EMS transport Physical Therapy Explanation of PT services 2 sessions a day Ask for pain medication at least 30 minutes prior to PT/OT sessions Information to know/things to bring Social information-live alone or have help Environment-do you live on one level or more, do you have stairs to enter? Prior level of function-how were you doing before you came into the hospital? Bring rolling walker from home to ensure proper fit and condition. Don’t buy RW’s. Bring loose fitting shorts or pants; elastic waist is easiest Walking shoes with good ankle support(no open heel shoes) Pre-operative Exercises Turn to guidebook page 28 for both Hip and Knee Begin pre-op exercises at home, 2-3 times a day to strengthen your body before surgery Stop, or do less repetitions if pain increases (1) Ankle Pumps Move ankle up and down. Repeat 20 times. (2) Quad Sets Lie on back, press knee into mat, tightening muscles on front of thigh. Hold for count of 5. Do NOT hold breath. Repeat 20 times. (3) Gluteal Sets (Bottom squeezes) Squeeze bottom together. Hold for count of 5. Do NOT hold breath. Repeat 20 times. (4) Hip Abduction and Adduction(slide heels out and in) Lie on back, slide legs out to side. Keep toes pointed up and knees straight. Bring legs back to starting point. Repeat 20 times. (5) Heel Slides (slide heel up and down) Lie on couch or bed. Slide heel toward your bottom. Repeat 20 times. (6) Short Arc Quads Lie on back, place towel roll under thigh. Lift foot, straightening knee. Hold for count of 5. Do not raise thigh off roll. Repeat 20 times. (7) Long Arc Quads Sit with back against chair. Straighten knee. Hold for count of 5. Repeat 20 times. (8) Armchair Push-Ups This exercise will help strengthen your arms for walking with crutches or a walker. Sit in an armchair. Place hands on armrests. Straighten arms, raising bottom up off chair seat if possible. Feet should be flat on floor. Repeat 20 times. (9) Seated Hamstring Stretch For Knees Sit on couch or bed with leg extended. Lean forward and pull ankle up. Stretch until pull is felt. (9) Mini Squats Holding on to a stable object, slightly bend knees and slowly straighten. Repeat 20 times. (10) Straight Leg Raises For Knees Lie on back, unaffected knee bent and foot flat. Lift opposite leg up 12 inches. Keep knee straight and toes pointed up. Relax. Repeat 20 times. (10) Seated Hamstring Stretch For Hips Sit on couch or bed with leg extended. Lean forward and ankle up. Stretch until pull is felt. Hold for 20-30 seconds. Keep back straight. Relax. Repeat 5 times. (11) Knee Extension Stretch For Knees Prop foot of affected leg up on chair. Place towel roll under ankle and ice pack over knee. Put 5-10 lbs. of weight on top of knee( a 5-10 lb. bag of potatoes or rice works well). Do for 20 minutes. Occupational Therapy(OT) Introduction of OT services 1 session a day ADL Equipment See handout for where to purchase recommended equiptment such as: reacher sock aid long handled shoehorn long handled sponge elastic shoelaces dressing stick bedside commode tub seat Equipment usually not covered by insurance Shower doors on bathtubs may need to be removed See you soon at the Joint Center