Drug Therapy for Older Adults
advertisement

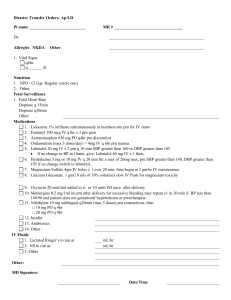
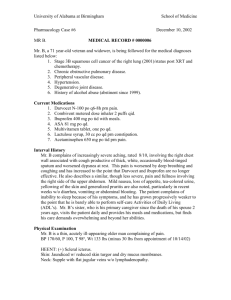
Drug Therapy for Older Adults: Acute Care Considerations Shelly Gray, PharmD, MS Acknowledgment: Peggy Odegard, PharmD Goals Describe how age-related physiological changes may affect disposition and response to drug therapy Identify drugs that may be associated with hospitalization Identify drugs that are associated with acute care problems such as falls, confusion, memory impairment, delirium Discuss strategies for optimizing therapy Did you know… 28% of hospitalizations for older adults are due to adverse drug reactions. Medications are a major cause of hip fractures Older adults take the bulk of medicines 32,000 seniors affected each year by a fracture following a medication-related fall. 12.7% of the U.S. population are over 65 years, but consume approximately 34% of total prescriptions. individuals 65 to 69 yo take an average 14 Rxs annually individuals 80 to 84 yo take an average 18 Rxs annually. Adverse drug events (ADEs) are among the top five greatest threats to the health of seniors. source: ascp.com Key Considerations Older persons are a heterogeneous group of individuals and comprise up to 50% of the inpatient population Delirium after surgery has been reported in 9-26% of elderly patients and up to 65% of patients post hip fx repair Pain is a complicating factor in post-op delirium Age is an independent risk for late, postoperative cognitive dysfunction with 9.9% of patients affected at 3 months in one study Case Study Mrs H, an 80 yo woman admitted after a cardiac arrest. Today she complained to her daughter of nausea and was somewhat confused prior to her collapse. PMH: atrial fibrillation, hypertension, osteoarthritis, insomnia and renal insufficiency. Medications: warfarin 2.5 mg mon, wed, fri; 5 mg other days digoxin 0.125 mg daily (reduced from 0.25 mg recently) isosorbide 20 mg TID aspirin 81 mg daily lotensin 20 mg daily oxybutynin 2.5 mg TID temazepam 15 mg at bedtime Glucosamine/chondroitin 500/400 TID PE/Labs: HR 37 on admit, Dig level today 3.4 ng/ml What do you think might have caused this admission? Case Study:History The medics found duplicate medication vials for each medication (including digoxin 0.25). Numerous pills were found on the floor. When asked about difficulty in taking medications as prescribed, she indicated she doesn’t miss many doses, but can’t quantify number of missed doses/week; “don’t like taking so many pills”; “don’t like the oxybutynin because it causes dry mouth”. She has difficulty with ambulation and reports occasional falls (several/week). What problems can be prevented during her admission? Cardiac Care Standing Orders I & O Saline lock Flush Q8H I&O each shift Aspirin 325mg chewable STAT if not given by medics or ED If aspirin not ordered, list contraindication: M E D I C A T I O N S L A B S R T D / C NTG 0.4mg SL Q5MIN X 3 PRN chest pain. Call MD if patient uses 3 doses within 2 hours NTG Infusion IV. Start at 5mcg/min and titrate to relief of chest pain. Keep SBP between 90 and 130mmHg. Clopidogrel (Plavix) 300mg PO X 1 dose Clopidogrel (Plavix) 75mg PO daily Metoprolol 25mg PO Q12H (hold if HR less than 50 bpm or SBP less than 95mmHg –OR- 2 or 3 heart block) If beta-blocker not ordered, list contraindication: Dalteparin (Fragmin) 120 units per kg subcutaneous Q12H Diazepam (Valium) 2.5mg IV -OR- 5mg PO Q3H PRN sedation (MR X 1 dose in 30 minutes if first dose ineffective) Promethazine (Phenergan) 12.5mg PO or IV Q6H PRN nausea (MR X 1 in 30 minutes) Zolpidem (Ambien) 5mg at bedtime PRN sleep. (May repeat x1 if ineffective) Docusate 240mg PO daily (hold for loose stools) MOM 30ml PO daily PRN constipation Maalox 30ml PO QID PRN indigestion Acetaminophen (Tylenol) 650mg PO Q4H PRN fever over 38.5 C or headache Admit labs (if not done in ED or office): CK, CK-MB, Troponin, BMP, Lipid Panel, CBC, Protime, PTT CK/CKMB, & Troponin-I draw 6 hours after arrival in ED EKG routine 12-Lead with Interpretation, 6 hours after admission and PRN chest pain XR chest 1 view portable on admission (if not done in ED), obtain report for chart Oxygen 1 to 6 liters per minute by nasal cannula PRN to keep oxygen SaO2 greater than 95% Initiate Cardiac Discharge education Consult to Cardiac rehabilitation Home Meds to be continued warfarin 2.5 mg mon, wed, fri; 5 mg other days digoxin 0.125 mg daily -on hold isosorbide 20 mg TID aspirin 81 mg daily lotensin 20 mg daily oxybutynin 2.5 mg TID temazepam 15 mg at bedtime Glucosamine/chondroitin (?- P&T not quite sure) Inpatient vs. home meds 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. Aspirin 325 mg QD NTG 0.4 SL prn Nitro drip Clopidogrel 75 mg QD Metoprolol 25 mg BID dalteparin 120 units/kg q12 Diazepam 5 mg po q3hr prn sedation Promethazine 12.5 mg po/IV q hrs prn nausea Zolpidem 5 mg HS prn DOSS 250 mg HS prn Maalox prn heartburn MOM 30 cc prn constipation APAP 650 mg 1-2 q4 prn pain/fever 1. 2. 3. 4. 5. 6. 7. 8. warfarin 2.5 mg mon, wed, fri; 5 mg other days digoxin 0.125 mg daily (on hold) isosorbide 20 mg TID aspirin 81 mg daily lotensin 20 mg daily oxybutynin 2.5 mg TID temazepam 15 mg at bedtime Glucosamine/chondroitin Case Study Intervention Concerns: cognition and medication adherence resulting in cardiac arrest; standing orders Inpatient Actions: change diazepam to lorazepam for anxiety minimize promethazine use; falls precautions Hold home aspirin tx ? need for isosorbide during ntg drip Either zolpidem or temazepam prn sleep, address sleep hygiene in planning for d/c Case Study Intervention Discharge Planning: remove all old med bottles to minimize risk of dosing error ? Need or change isosorbide TID to once daily product oxybutynin was not very effective so discontinue not able to simplify the warfarin regimen ? Need for aspirin taper temazepam How it looks on discharge! Medical Problems: htn, atrial fibrillation, s/p recent AMI, insomnia, osteoarthritis, renal insufficiency Meds: lotensin 20 mg daily warfarin 2.5 mg mon, wed, fri; 5 mg other days Aspirin 81 mg daily Metoprolol 50 mg BID (hold if pulse <60 bpm, call if pulse >100 bpm) Acetaminophen 500 mg TID prn knee pain Glucosamine/chondroitin 500/400 TID for osteoarthritis Chamomille tea for sleep (her preference) Most Common Prescription Drugs Therapeutic Class Cardiovascular CNS Endocrine/Metabolic Analgesic Respiratory Duke EPESE 1986-1987 % 47 13 11 10 7 Most Common OTC Drugs EPESE(%) MoVIES (%) Analgesic 42 66 Nutritional 23 38 Gastrointestinal 21 38 Respiratory 3 5 Frequency of Drug Use MoVIES Ann Pharmacother 1996:30:589 30 % (n=1360) 25 20 15 10 5 0 0 1 2 3 4 Number of Medications 5-7 8+ Incidence of ADEs in Older Persons in Ambulatory Setting Cohort of 27,617 Medicare enrollees 1523 ADEs 28% preventable Error occurred at prescribing and monitoring phases 38% were serious, life-threatening or fatal 42% of these were preventable JAMA 2003;289:1107 Which Drugs Cause Serious ADEs? Ambulatory Diuretics Nonopioid analgesics Anticoagulants Antiepileptics Nursing Home Opioids Antipsychotics Antiinfectives Antiepileptics Antidepressants JAMA 2003;289:1107 Arch Intern Med 2001;161:1629 How does aging influence drug therapy? Goal #1 Describe how age-related physiological changes may affect disposition and response to drug therapy Consideration #1 Pharmacokinetic changes do occur with age Absorption Distribution Hepatic Metabolism Renal Elimination These changes may result in the need for adjustment of drug dosing and require careful monitoring for effects. Absorption: The chemistry of the GI track changes with aging. These changes do not have any major impact on medication dosing or use! Drug absorption in the gastrointestinal (GI) system is not impaired despite many age-related changes in the GI tract with age decreased GI blood flow increased gastric pH diminished GI motility The most significant effect on absorption is other illnesses…Effects on cardiac output (e.g. CHF) or gut rest are considerations in the acute care setting Drug Distribution: The makeup of the body changes with aging. Age-related increased body fat and decreased lean body mass may predispose to retention of more fatsoluble drugs Example, Valium™ and some anesthetic agents over-dose of drugs distributed to lean tissue or body water Example, ethanol or aminoglycosides Metabolism: Liver performance is somewhat reduced with aging. The liver’s system for activating medications or performing metabolism is not as efficient with aging. With aging, the liver’s size and blood flow are reduced which results in some reduction in the ability for the liver to metabolize (inactivate) drugs Recommendation: If used, use medicines that have shorter half-lives or don’t require extensive metabolism. Renal Elimination Age-related decline in kidney function by about 1% per year after the age of 50 years Can lead to excess or over-dose of drugs cleared by the kidney if dose not adjusted (e.g. many antibiotics, ranitidine or Zantac™, lithium) Creatinine Clearance creatinine = clearance (140-age) weight in kg 72 (serum creatinine) *multiply by 0.85 if female ** use IBW unless >20% over ***estimate based on stable renal function so may not apply in acutely ill patients Is it an issue? “Young” “Old” Cr Cl = (140 - 40) 72 72 (1.0) Cr Cl = 100 ml/min Cr Cl = (140-80) 72 72 (1.0) Cr Cl = 60 ml/min Yes: <60 ml/min is a cutoff for adjustment of many drug doses Case 80 yr old female with hypertension & DJD Started on ranitidine 150 mg BID for GERD Estimated renal function (140-80) 65 kg (0.85) 1.5 * 72 CrCl= 31 ml/min Meds: Tylenol 1 gm QID, Enalapril 10 mg BID 65 kg, Scr=1.5 mg/dl Effect of reduced renal function? Can lower ranitidine dose to QD. General Principles of Drug Clearance Steady state concentration Css= F * Dose Cl Half life (t1/2)=0.693*Vd/Cl Factors that reduce clearance will result in an increased plasma concentration and may increase toxicity Factors that increase Vd may result in increase T ½ if clearance doesn’t change Consideration #2 Pharmacokinetic and pharmacodynamic parameters may be altered more by concomitant diseases, medications and nutritional status than by aging alone. New drugs should be avoided/ used cautiously until their full effects in older persons are known. PK Action Item! Toxicity due to an age-related pharmacokinetic change can often be anticipated and prevented with appropriate dose adjustments and close monitoring for adverse events Screen for appropriate dosing on admission and adjust whenever needed (keep in mind, some doses may have been so for years- it’s never to late to change them!) Pharmacodynamics Sensitivity to certain drugs increases with age especially drugs that work at receptors or in the central nervous system Propranolol (Inderal™) Diazepam (Valium™) and valium-like drugs Narcotics (e.g. Vicodin™ or morphine) Why does this happen? Altered homeostatic mechanisms physiological reserve capacity to respond to stress beyond energy needed for daily activities gradual reduction occurs with aging more susceptible to decompensation under stress (infections, trauma, drug effects). more difficult to maintain homeostasis (regulate blood pressure, pH, etc). Specifically Changes in water/sodium regulation Decrease in balance control Prolongation in CNS reaction time Reduced responsiveness to hypoglycemia 1. 2. 3. 4. • Altered beta receptor sensitivity to glucagon Inability to recover quickly from orthostasis 5. • altered baroreceptor response How do these Pharmacodynamic Changes Affect Medication Use? Altered receptor sensitivity may affect efficacy or toxicity of certain drugs: Beta agonists (e.g. albuterol) Beta antagonists (e.g. metoprolol) How do these Pharmacodynamic Changes Affect Medication Use? Risk of orthostatic hypotension greater Vasodilators (e.g. hydralazine) ACE inhibitors beta antagonists nitrates calcium channel antagonists How do these Pharmacodynamic Changes Affect Medication Use? Altered sensitivity to drugs affecting neurotransmitters Dopaminergic system decrease in dopamine2 receptors in striatum Cholinergic system loss of cholinergic cells decrease in choline acetyltransferase How do these Pharmacodynamic Changes Affect Medication Use? Increased sensitivity to drugs with effects on neuroendocrine system Anaesthetics Opioids Anticonvulsants Psychotropic agents PD Action Item! Toxicity due to an age-related pharmacodynamic change may be hard to predict, however careful monitoring for desired effects and taking actions to avoid unwanted effects is key to preventing problems. Goal #2 Identify drugs that may be associated with hospitalization Case Anne is an 88 year old women who was just admitted for a GI bleed. She has a h/o stomach upset x3 weeks (burning pain) for which she was taking ranitidine OTC. What are your initial thoughts? Could a medication have caused this problem? The answer: YES Four weeks prior to hospitalization, she… began using ibuprofen 400 mg every 4 hours while awake for dental pain. scheduled a DDS visit, however, needed to reschedule so delayed the visit by 20 days. did not report the regular ibuprofen use to her PCP because she didn’t think it was important since she would see her DDS about the dental pain. Ouch! Regular use of NSAIDs is a leading cause of GI bleeding and gastritis in older adults! 1/3 of regular NSAID users have GI ulceration (gastric or duodenal) on endoscopy OR 5.36 for serious gastric complications Gut protection is essential for regular NSAID users to prevent problems Becker JA. Br J Clin Pharmacol. 2004; 58(6): 587–600 Costs of this ADE Hospitalization (via ED) Two office visits to PCP GI consultation Endoscopy Rxs Cancellation of social activities Frustration and fear 3 plane flights for family How does this happen? The Prescribing Cascade BMJ 1997;315:1096-1099 Drug-related Causes of Admission Key Players Drug 1. 2. 3. 4. NSAIDs Narcotics Digoxin CNS active drugs like benzodiazepines, sleepers, some BP meds Non-adherence Problem 1. 2. 3. 4. GI bleed GI obstruction Arrhythmia Falls Poor illness control Always consider medication use in the differential diagnosis A direct drug effect? Age-related pharmacokinetic change? Change the dose Age-related pharmacodynamic change? Stop the drug Stop the drug? Change the dose? Drug-related needs Case SR, a 75 year old healthy female, visits her MD with a 1 month history of sleep complaints. She “just can’t fall asleep at night” and would like something to help. Her MD prescribes zolpidem (Ambien ™ ) 10 mg at bedtime as needed (#30). ADEs Can Lead to Hospitalization 1 week later, SR is rushed to the ER after suffering a fall down a flight of stairs. A fracture of the right femur is seen on x-ray. While she tolerates the surgery well, she has poor endurance with therapeutic exercises and therefore is sent to a local skilled nursing facility. 1yr later, she still requires use of a walker. Pertinent History about SR Drinks ½ pot of coffee daily Takes a mid-morning and early evening nap daily – just does not have any energy Does not exercise Lost her husband 1 year ago. Is still very quick to tears and is having difficulty enjoying pleasurable activities Goal #3 Identify drugs that are associated with acute care problems. The primary concern… Some medicines cause changes in the body that might seem like a normal part of aging so are unrecognized as problematic therapies. confusion falling constipation feeling sad or depressed poor memory Heartburn Medications that may increase risk of falls Blood pressure medicines Antidepressants Antihistamines Parkinsons medicines Anti-psychotics Benzodiazepines Decongestants Opioids Muscle relaxers Sleep medicines Urinary anticholinergics Drugs and Falls/Hip Fractures Leipzig R JAGS 1999:47:40, JAGS 1999:47:30 Consistent evidence Benzodiazepines Antidepressants Antipsychotics Weak/inconsistent evidence Analgesics (NSAIDS, narcotics) Cardiovascular agents thiazides, antiarrhythmics, digoxin BZD and Hip Fractures: Does Duration of Action Matter? Several studies have found that both short-and long-acting benzodiazepines increase risk ~2 fold for falls/hip fractures Short acting: oxazepam, alprazolam Long acting: diazepam, flurazepam Dose probably more important than half-life Herings R Arch Intern Med 1995, Neutel Age Aging 1996 Medications cause constipation Narcotics Require stimulant laxative, at the minimum, to promote GI motility with ongoing use (e.g. Senna). A stool softener can be added but is inadequate as sole therapy. Other products associated with constipation include anticholinergics, CCBs, calcium, iron Medications cause cognitive dysfunction, memory impairment, and delirium Some Culprit Drugs Narcotics Hypnotics Benzos Anesthetics Phenothiazines Corticosteroids anticholinergics Possible Problems All may cause falls, confusion, delirium, or other cognitive dysfunction BZDs may cause memory impairment Phenothiazines may cause dystonic rxns Drug Effects on Cognition 307 outpatients with dementia 12% (n=36) had an ADE impairing cognition Discontinuation/modification improved cognition 16 were using benzodiazepines Larson Ann Intern Med 1987 Delirium Delirium is not an uncommon problem in the operative period for older adults Delirium associated with surgery may occur early (post op day 2-7 interval) or late (3 mos) Pain increases risk for delirium and may compromise a weakened CV system Pre-operatively Peri-operatively Post-operatively Age increases risk for delirium How should delirium be managed? 1. 2. 3. 4. Remove or correct the cause! Low dose haloperidol (0.5 mg IV/PO) may be used for its sedative qualities (IV faster acting) Low dose, oral atypical antipsychotics (e.g. risperidone 0.25 mg) are used, however, action is not immediate due to oral absorption. Some concern with association with stroke. Management is acute! Remember, these meds may be confused for chronic meds if sent home at discharge! Medications to avoid using in older adults unless absolutely needed Meperidine (Demerol) Propoxyphene (Darvon™) Pentazocine (Talwin) Trimethobenzamide (Tigan) Muscle relaxants like Robaxin, Soma, Flexeril Disopyramide (Norpace) Methyldopa (Aldomet) Long acting benzos (Dalmane, Valium, Librium) Amitriptyline Geriatrics Consultation In a small RCT (n=126), a structured geriatrics consultation resulted in reduced risk of delirium (RR 0.64) for older adults (mean age 79) admitted for surgical repair of hip fx. Volume 49 Issue 5 Page 516-522, MAY 2001 Content of Structured Geri Consultation CNS oxygen delivery Fluid/electrolytes Severe pain mgmt Eliminate unnecessary meds Regulate bowel and bladder fn Adequate nutrition Early mobilization & rehab Px, early detection, and tx of major post-op complications Appropriate environmental stimuli Tx agitated delirium Volume 49 Issue 5 Page 516-522, MAY 2001 Optimizing Drug Use in the Elderly 1. 2. 3. 4. Consider whether drug therapy is necessary Use least number of drugs to treat common problems Adjust dosing to match pk/pd needs Establish reasonable therapeutic endpoints and monitor for desired outcome 5. Watch for ADRs and for effects on functional status Monitor and encourage persistence with therapy Consider possibility of drug-induced illness for any symptom or problem