Function of the adrenal glands

ةصاخلا ةيروسلا ةعماجلا
يرشبلا بطلا ةيلك
ةحارجلا مسق
Adrenal Glands Disorders
Dr . M.A.Kubtan MD - FRCS
M.A.Kubtan
1
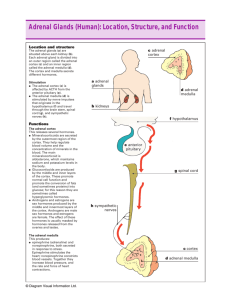
Anatomy
ADRENAL GLANDS
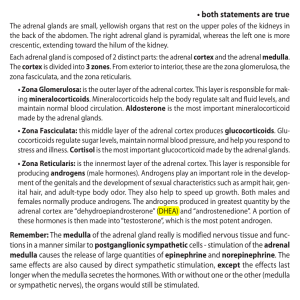
components of the gland: the inner adrenal medulla and the outer adrenal cortex .
The weight of a normal adrenal gland is approximately 4 g.
They are situated at the upper poles of the kidneys in the retroperitoneum within
Gerota’s capsule.
They are well supplied by blood vessels.
A large adrenal vein drains on the right side into the vena cava and on the left side into the renal vein.
Position of the adrenal glands
(hatched) in the retroperitoneum.
M.A.Kubtan
2
Embryology
The cortex and the medulla
Arise from different blastodermic layers .
Mesodermal cells form the adrenal cortex .
Neuroectodermal cells migrate to the cortex and form the adrenal medulla.
M.A.Kubtan
3
Function of the adrenal glands
Catecholamines adrenalinen(epinephrine) but also noradrenaline
(norepinephrine) and dopamine. are secreted by the adrenal medulla .
corticosteroids, aldosterone and cortisol are synthesised in the adrenal cortex.
M.A.Kubtan
4
Catecholamines Functions
Act as hormones .
They are secreted directly into the circulation.
Their effects are mediated through α and β receptors on target organs .
Activation of the cardiovascular system .
Increase in blood pressure and heart rate.
Vasoconstriction of vessels in the splanchnic system .
Vasodilatation of vessels in the muscles an bronchodilatation.
Increased glycogenolysis in liver and muscles .
M.A.Kubtan
5
Adrenal cortex function
Cells of the zona glomerulosa produce aldosterone .
The target organs of aldosterone are the kidneys, the sweat and salivary glands and the intestinal mucosa.
Aldosterone promotes sodium retention and potassium excretion.
Renin–angiotensin system are the most important regulators of aldosterone secretion .
M.A.Kubtan
6
Renin–Angiotensin System
Renin produced by the juxtaglomerular cells in the kidneys .
Its substrate angiotensinogen to generate angiotensin 1 .
Angiotensin I is converted by the angiotensin-converting enzyme (ACE) to the octapeptide angiotensin II .
Angiotensin II, is modified to angiotensin III.
Both II & III stimulate the secretion of aldosterone from the adrenal cortex
.
M.A.Kubtan
7
Function of the zona fasciculata and zona reticularis
Cortisol
Cortisol secretion is regulated by adrenocorticotrophic hormone (ACTH)
The hypothalamus controls ACTH secretion by secreting corticotropinreleasing hormone (CRH).
Adrenal androgens
Dehydroepiandrosterone (DHEA)
Dehydroepiandrosterone sulphate
( DHEAS )
M.A.Kubtan
8
DISORDERS OF THE ADRENAL CORTEX
Incidentaloma
Definition
A clinically unapparent mass detected incidentally by imaging studies conducted for other reasons.
Incidence
The prevalence of adrenal masses in autopsy studies ranges from
1.4% to 8.7% and increases with age.
Incidentalomas may be detected on imaging studies in 4% of patients.
More than 75% are non-functioning adenomas .
Cushing’s adenomas, phaeochromocytomas and even adrenocortical carcinomas may be present .
M.A.Kubtan
9
Prevalence of non-functioning and functioning tumours in patients with incidentalomas
Tumour Prevalence (%)
Non-functioning adenoma 78
Cushing’s adenoma 7
Adrenocortical carcinoma 4
Phaeochromocytoma 4
Myelolipoma 2
Cyst 2
Metastases 2
Conn’s adenoma 1
M.A.Kubtan
10
Diagnosis
Hormonal evaluation includes:
Morning and midnight plasma cortisol measurements;
A 1-mg overnight dexamethasone suppression test;
24-hour urinary cortisol excretion (optional);
24-hour urinary excretion of catecholamines, metanephrines
Plasma-free metanephrines;
Serum potassium, plasma aldosterone and plasma renin activity;
Serum Dehydroepiandrosterone sulphate DHEAS, testosterone or 17βhydroxyestradiol (virilising or feminising tumour).
M.A.Kubtan
11
Radiological & Histological Diagnosis
For evaluation of malignancy computerised tomography (CT) or magnetic resonance imaging (MRI) should be performed in all patients with adrenal masses .
Fine-needle aspiration cytology after a phaeochromocytoma has been excluded.(A pheochromocytoma will often release a burst of catecholamines, with the associated signs and symptoms quickly following ).
The likelihood of an adrenal mass being an adrenocortical carcinoma increases with the size of the mass (25% > 4 cm).
M.A.Kubtan
12
Types of Adrenal Cortex Disease
Primary hyperaldosteronism (Conn’s adenoma ) .
Cushing’s syndrome .
Adrenogenital syndrome (Congenital adrenal hyperplasia ) .
Adrenal insufficiency (loss of function of the adrenal cortex ).
M.A.Kubtan
13
Primary hyperaldosteronism
(Conn’s adenoma )
Incidence : Commonly unilateral adenoma , 12% of hypertensive patients have PHA with normal potassium levels.
Pathology : In 20–40% of cases, bilateral micronodular hyperplasia is causative. 70% have hyperplasia and 30% unilateral adenoma.
Clinical features : Most patients are between 30 and 50 years of age , female predominance , non-specific symptoms: headache, muscle weakness, cramps, intermittent paralysis, polyuria, polydypsia ( excessive thirst ) and nocturia , hypertension and hypokalaemia .
Diagnosis : Biochemical diagnosis is the assessment of potassium level and the aldosterone to plasma renin activity ratio , MRI or CT with a sensitivity of 80–90% , selective adrenal vein catheterisation , determination of aldosterone to cortisol ratio (ACR).
Treatment : Laparoscopic or open surgical resection when indicated .
M.A.Kubtan
14
Cushing’s syndrome
Definition : Hypersecretion of cortisol , (85%) ACTH-dependent ,
ACTH-independent (pituitary Adenoma ) or Ectopic ACTH-producing tumours .
Clinical features of Cushing’s syndrome :
1. Weight gain/central obesity
2.Diabetes
3.Hirsutism
4. Hypertension
5.Skin changes (abdominal striae, facial plethora, ecchymosis, acne)
6.Muscle weakness
7.Menstrual irregularity/impotence
8.Depression/mania
9.Osteoporosis
10.Hypokalaemia
Diagnosis : Biochemical , MRI or CT .
Treatment : Surgery when indicated .
M.A.Kubtan
15
M.A.Kubtan
16
M.A.Kubtan
17
M.A.Kubtan
18
M.A.Kubtan
19
Phaeochromocytoma
(adrenal paraganglioma)
This is a tumour of the adrenal medulla, which is derived from chromaffin cells and which produces catecholamines.
Approximately 10% of phaeochromocytomas are malignant.
About 8% of patients with an apparently benign phaeochromocytoma subsequently develop metastases.
M.A.Kubtan
20
M.A.Kubtan
21
M.A.Kubtan
22
M.A.Kubtan
23