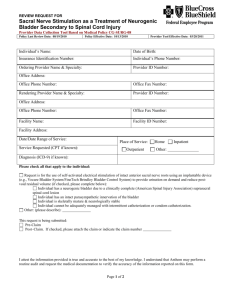
Intraoperative Monitoring
advertisement

Intraoperative Monitoring Behrouz Zamanifekri, MD Neurophysiology Fellow KUMC March 2013 Intraoperative monitoring The most primitive method of monitoring the patient 50 years ago were continuous palpation of the radial pulsations throughout the operation or wake up test!! History 1921, Dr Penfield, intraoperative neurophysiology research 1950s, Dr Penfield, electrical stimulation to find epileptic foci 1970s, Dr Brown used SSEP for scoliosis operation 1974 , among 7,800 operations conducted with Harrington instrumentation, 87 patients had subsequently developed significant spinal cord problems Early 1980, IOM in operations for large skull base tumors 1980, the American Society for Neurophysiological Monitoring [ASNM]) Introduction What is IOM ? use of neurophysiological recordings for detecting changes caused by surgically induced insults assess the function of specific parts of the nervous system continuously during an operation It is becoming part of standard medical practice What is the purpose of IOM? 1. Reduce the risk of postoperative neurological deficits 2. Identify specific neuronal structures and landmarks that cannot be easily recognized 3. Research purposes in basic science, pathophysiology and therapeutic management What are the most common types of recording? Spontaneous activity EEG EMG Evoked responses (through external stimulation of a neural pathway) Sensory : 1- visual 2-auditory 3-somatosensory Motor The type of test to be used and the sites of recording and stimulation are chosen on a case by case Complications during surgery ischemia mechanical insult PRACTICAL ASPECTS OF MONITORING SPINAL CORD Spinal Monitoring Spinal cord, nerve roots, and blood vessels are frequently placed at risk for injury Electrophysiological modalities for monitoring: SSEPs MEPs free run or spontaneous EMG (sEMG) triggered EMG (tEMG) Spine Surgery: surgical insults to the ventral parts of the cord, using motor evoked potentials (MEPs) dorsal columns of the spinal cord , SEP the purpose of IOM is to detect response changes due to surgery, not to make a clinical diagnosis Monitoring of Somatosensory Evoked Potential Earliest used method in IOM 1970s in operations for scoliosis Stimulation of peripheral nerve and recorded from scalp Only monitor dorsal(sensory) spinal cord patient sensory examination for position and vibration is recommended prior to surgery SSEP By electrical stimulation of peripheral nerves Median nerve at wrist for injury above C8 Posterior tibial nerve at ankle for injury below C8 spinal cord through the dorsal roots, ascending pathways, thalamus and, finally, to the primary sensory cortex Recording P9 from P11 P14-16 P20 brachial plexus Dorsal horn Dorsal column nuclei Primary sensory cortex(contralat.) upper limb SSEP N37 Primary sensory cortex(contralat.) lower limb SSEP Location of the stimulating and recording posterior tibial nerve SEPs. It is important to note - Earlier peaks tend to be less sensitive to anesthesia - used to differentiate SSEP monitoring changes resulting from anesthetic effects from surgical manipulation. Alarm criteria -50% reduction in amplitude -10% increase in latency Factors that affect the SSEP amplitude include halogenated agents, nitrous oxide, hypothermia, hypotension, and electrical interference Normal SSEPs from median nerves and posterior tibial nerves SSEP in Peripheral nerves? sciatic nerve injury during pelvic fracture Injuries to brachial plexus in positioning of pt is common Prolong latency of all peaks and decrease amplitude Nerve root SSEP: insensitive to changes in nerve root function Why? SSEP in nerve root injury? SSEP used during placement of pedicle screws Risk of spinal nerve root injury If one root damaged, no change in SSEP Dermatomal stimulation is better Inhalational anesthetics, cortical responses Intravenous Agents - Propofol increases the latency by approximately10% - Benzodiazepines reduce the amplitude of cortical SEP - Etomidate : cortical SEP amplitude augmented 200–600%, increases SEP latencies - Opiates, cause a slight increase in SEP latency - Muscle relaxants, not affect SEPs SEP changes due to surgical maneuvers (e.g., spinal distraction) or ischemia (e.g., after placement of an artery clamp) are abrupt and localized and only one side of the body may be affected whereas changes due to anesthesia or body temperature changes are relatively slower Detection of cord injury due to misplaced instrumentation just after placement of instrumentation, both the cortical (peak N45) and cervical (peak N30) responses disappear SEPs obtained after cross-clamping of the internal carotid ,which resulted in ischemia (time 9:45) that later deteriorated (9:55). After placement of a shunt, response amplitude is restored to within normal limits (time 10:01). Procedures involves the ICA, MCA, PCA, P.Com, or BA? Median nerve SEPs procedure involves the ACA or the A.Com artery? Posterior tibial nerve MONITORING SPINAL MOTOR SYSTEM Introduction SSEP for sensory pathway MEP for motor SSEP + MEP: Small reversible changes in SSEP that occur when motor pathway are injured MEP 1990s, TC-MEP as a method to monitor the corticospinal tracts Prior to MEP monitoring, the only way to assess corticospinal tract during surgery was wake-up test TC-MEPs stimulation through the skull with signal recording at the level of muscle (CMAP) nerve (neurogenic MEP) spinal cord ( D-wave ) -the newer technologies is continuous free-running EMG throughout the surgery Recording of Muscle Evoked Potentials Stimulation of cortex, activation of coticospinal, EMG of distal( Hand m., abd hallucis, tibialis anterior) Muscle relaxant can not be used MEP Interpretation of MEP Recording 4 methods : 1) all-or-nothing criterion: the most used method, complete loss of the MEP signal from a baseline recording is indicative of a significant event 2) amplitude criterion: 80% amplitude decrement in at least 1 out of 6 recording sites 3) threshold criterion: increases in the threshold of 100 V or more required for eliciting CMAP responses that are persistent for 1 h or more 4) morphology criterion: changes in the pattern and duration of MEP waveform morphology TcMEP monitoring contraindicated in -deep brain stimulators or cochlear implants Tongue biting is the most common complication Normal MEPs Recording of the response from spinal cord(D, I wave) Recording from epidural electrodes D (direct activation of corticospinal) I ( indirect, through transsynaptic) Not affected by muscle relaxants, but latencies increase with cooling Subdural electrodes can be substituted for epidural electrodes Needle electrodes can be place in interspinous ligaments both sides of surgery area major benefits reported during intramedullary spinal cord tumor resection a complete loss of MEPs with at least 50% preservation of the D-wave amplitude generally results in a transient paraplegia Spontaneous EMG monitor nerve roots recording electrodes placed in the muscles no stimulation is performed monitoring of 2 muscles is recommended C5 nerve root injury, The deltoid and biceps brachii MEPs be obtained intermittently sEMG no paralytic agents train-of-4 testing should indicate that at least 3 out of 4 Myasthenia gravis, Botox treatments, and muscular dystrophy are classic conditions that interfere with EMG Abnormal sEMG spikes Bursts trains Trains are continuous, repetitive EMG firing caused by continuous force applied to the nerve root. Example of EMG activity indicating irritation of the nerve Baseline recordings. Note the low amplitude background activity High amplitude spikes are present Artifacts may be mistaken for spikes or trains a neurostimulator the surgical table the surgeon’s head light bipolar electrocautery device Triggered EMG (Pedicle Screw Stimulation) used to determine whether screws have breached the medial or inferior pedicle wall and thus pose a risk to the exiting nerve root at that level When a pedicle screw is accurately placed, the surrounding bone acts as an insulator to electrical conduction, and a higher amount of electrical current is thus required to stimulate the surrounding nerve root. When a medial pedicle wall breach occurs, the stimulation threshold is significantly reduced False negative response muscles relaxants fluid, blood, or soft tissue around the head of the screw , shunt current away from the screw it is important that the stimulation probe be placed directly on the top of the screw and not the tulip, as these 2 structures are not structurally fused Presence of preexisting nerve root injury. Injured nerve roots will have higher triggering thresholds, Due to the variation in thickness and shape between thoracic and lumbar pedicles, different stimulation thresholds exist for these regions A threshold < 10 mA for screw stimulation, suggest a medial wall breach in the lumbar pedicles A thresholds > 15 mA indicate a 98% likelihood of accurate screw positioning For thoracic pedicle screw placement, stimulation threshold < 6 mA suggest a medial pedicle breach In cervical and thoracic procedures, the spinal cord are of greater importance Conversely, in lumbar or sacral procedures the nerve roots are at greater risk of injury Overview of IOM classified by spinal region Conclusions Multimodality neurophysiological monitoring is extremely valuable in the prevention of neurological injury Knowledge of the benefits and limitations of each modality helps maximize the diagnostic value of IOM during spinal procedures Neurosurg Focus / Volume 27 / October 2009 A concise guide to intraoperative monitoring / George Zouridakis, Andrew C. Papanicolaou.2001 Intraoperative neurophysiological monitoring / Aage R. Moller. -- 2nd ed.