Regulation of Respiration
advertisement

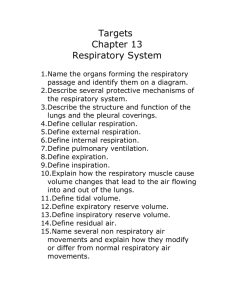
Regulation of Respiration Learning Objectives Regulation of ventilation by the CNS and PNS. • Know the basic anatomy of the CNS respiratory center. • Know how the dorsal respiratory group, ventral respiratory group and the pneumotaxic center control respiration. • Understand how chemical changes in the CNS and PNS influence the respiratory changes. • Know how respiration is regulated during exercise. • Understand the changes in the pulmonary system that cause Cheyne-Stokes breathing and sleep apnea. Review of Gas Exchange Review Mechanics of Breathing 1. Diaphragm contracts during inspiration and relaxes during expiration (major force during normal, quiet breathing). 2. Intercostal muscles elevate and depress the ribs. 3. Abdominal muscles contract during heavy expiration. These are skeletal muscles that need stimulation from the CNS to contract. Respiratory Centers of the CNS • The primary portions of the brainstem that control ventilation are the medulla oblongata and the pons. Respiratory Centers 6 Two respiratory nuclei in medulla oblongata Inspiratory center (dorsal respiratory group, DRG) • more frequently they fire, more deeply you inhale • longer duration they fire, breath is prolonged, slow rate Expiratory center (ventral respiratory group, VRG) •involved in forced expiration 7 Dorsal Respiratory Group • Sets the basic respiratory rate. • Stimulates the inspiratory muscles to contract (diaphragm). • The signals it sends for inspiration start weakly and steadily increase for ~ 2 sec. This is called a ramp and produces a gradual inspiration. • The ramp then stops abruptly for ~ 3 sec and the diaphragm relaxes. Control of Dorsal Respiratory Group The vagus nerve and glossopharyngeal nerves receive input from: • Peripheral chemoreceptors • Baroreceptors • Several pulmonary receptors Sensory input can change 2 qualities of the ramp: • The rate of increase (e.g., increase during heavy breathing to fill lungs more rapidly). • The timing of the stop (e.g., stopping the ramp sooner shortens the rate of inspiration and expiration, thus increasing the frequency of respiration). Ventral Respiratory Group • Inactive during normal, quiet respiration. • At times of increased ventilation, signals from the dorsal group stimulate the ventral group. • The ventral group then stimulates both inspiratory and expiratory muscles. E.g., the abdominal muscles are stimulated to contract and help force expiration. Respiratory Centers in Pons Pneumotaxic center (upper pons) •Sends continual inhibitory impulses to inspiratory center of the medulla oblongata, •As impulse frequency rises, breathe faster and shallower Apneustic center (lower pons) •Stimulation causes apneusis •Integrates inspiratory cutoff information 11 Pneumotaxic Center • Controls stopping point of the dorsal group ramp. • Strong pneumotaxic stimulation shortens the duration of inspiration and expiration. This increases the breathing rate. • Strong pneumotaxic stimulation can increase the rate of breathing to 30-40 breaths/min and weak pneuomotaxic stimulation can decrease the breathing rate to 3-5 breaths/min. Respiratory Structures in Brainstem 13 2. Rhythmic Ventilation (Inspiratory Off Switch) • Starting inspiration – Medullary respiratory center neurons are continuously active (spontaneous) – Center receives stimulation from receptors and brain concerned with voluntary respiratory movements and emotion – Combined input from all sources causes action potentials to stimulate respiratory muscles 14 •Increasing inspiration –More and more neurons are activated •Stopping inspiration –Neurons receive input from pontine group and stretch receptors in lungs. –Inhibitory neurons activated and relaxation of respiratory muscles results in expiration. –Inspiratory off switch. 15 3. Higher Respiratory Centers Modulate the activity of the more primitive controlling centers in the medulla and pons. Allow the rate and depth of respiration to be controlled voluntarily. During speaking, laughing, crying, eating, defecating, coughing, and sneezing. …. Adaptations to changes in environmental temperature -Panting 16 Respiratory Center • We will discuss the following groups of neurons in the respiratory center. • Dorsal respiratory group (medulla). • Ventral respiratory group (medulla). • Pneumotaxic center (pons). Control of Respiratory Center • We have discussed the CNS structures that control ventilation. • Now, we will go over the following: 1. How chemical changes in the CNS and PNS influence the respiratory center. 2. Respiration during exercise. 3. Some disorders of respiration. Chemical Signals in the CNS • The levels of what chemicals are going to control respiration? CO2, H+ ions and O2. • In the CNS, CO2 and H+ are particularly important. • O2 has a greater effect in the PNS. H+ is the Main Stimulus (in the CNS) • In the chemosensitive areas of the respiratory center, increased H+ is the main stimulus. • Activation of the central chemoreceptors by H+ excites the dorsal respiratory group of neurons (inspiratory area) and thus increase the respiration rate. • Why then, does activation of central chemoreceptors occur mainly after a rise in peripheral CO2, but not so much with peripheral H+? CO2 and H+ are Linked • The blood-brain barrier is not very permeable to H+; however, CO2 easily diffuses across the BBB (as usual). • As we have discussed, increases in CO2 cause increases in H+. • So, once CO2 diffuses into the chemosensitive regions of the CNS, H+ is formed and stimulates the dorsal group. Effect of PCO2 and pH on Ventilation Acute and Chronic Elevation of CO2 and H+ • An acute increase in CO2/H+ stimulates respiration, which helps remove the excess CO2/H+. • What system regulates the long-term levels of H+? Renal Control of Acid-Base Balance • Bicarbonate must react with H+ before it can be reabsorbed. • If H+ is high, the kidneys reabsorb nearly all the bicarbonate. The excess H+ in the tubular lumen combines with phosphate and ammonia and is excreted as salts. • The extra bicarbonate will then slowly diffuse into the CNS and bind the excess H+. Sensing PO2 in the CNS Why does the CNS directly monitor levels of CO2 or H+ ions more than O2? • Remember the O2-hemoglobin dissociation curve. • Hemoglobin buffers O2 delivery to the tissues even with large changes in PO2. • Also remember, the brain receives a very steady supply of blood under normal conditions. • So, O2 delivery in the brain is fairly stable under normal conditions and there is no as much of a need to directly monitor PO2. Peripheral Chemoreceptors • Peripheral chemoreceptors are located in carotid and aortic bodies and sense the level of O2 (PO2). • Blood flow to the receptors is very high; so very little deoxygenated (venous) blood accumulates. • Thus, they sense arterial O2 levels. • Low PO2 levels stimulates the dorsal respiratory group. • The signal is sent to the respiratory center via the vagus or glossopharyngeal nerve Effect of Arterial PO2 on Ventilation Effect of CO2 and H+ on Peripheral Chemoreceptors • Elevated CO2 and H+ also stimulate peripheral chemoreceptors. • This effect is less powerful than the effect on CNS chemoreceptors, but it occurs ~ 5 x faster than occurs in the CNS. Hering-Breuer Inflation Reflex • When the lungs become overinflated, streth receptors in the muscle portions of bronchi and bronchioles send a signal through a vagus nerve to the dorsal respiratory group of neurons. • This signal switches off the inspiratory ramp sooner. This decreases the amount of filling during inspiration, but increases the rate of respiration. Respiration During Exercise • During exercise, O2 consumption and CO2 formation can increase 20-fold. • What happens to the partial pressures of O2 and CO2 in the blood? The partial pressures do not change much. This can occur if the ventilation increases in proportion to the increase in O2 consumption and CO2 production. O2 Consumption and Ventilation During Exercise • The increase in ventilation during exercise prevents large changes in the partial pressure of O2 or CO2. • The increase in ventilation occurs before there is a change in blood chemicals. • Neuronal signals are sent to the respiratory center during exercise, possibly at the same time signals are being sent to the skeletal muscles. Alveolar Ventilation and Arterial PCO2 During Exercise • The decrease PCO2 at the onset of exercise demonstrates that increasing blood CO2 does not trigger the increase in ventilation during exercise. • However, chemical changes do fine-tune the ventilation rate. Notice the decrease in ventilation associated with the decrease in PCO2 at the onset of exercise. Cheyne-Stokes Breathing • Not having local control over ventilation can be an issue if there is a delay or problem in communication between the lungs and the CNS. • E.g., Cheyne-Stokes breathing occurs when there is a long delay in the transport of blood from the lungs to the brain. Cheyne-Stokes Breathing – Cardiac Failure • Because of the delay in getting blood to the CNS, changes in alveolar O2 or CO2 progress longer than normal. Then, once the change is sensed by the CNS, the resulting change in ventilation proceeds longer than is needed. • This type of Cheyne-Stokes breathing can occur in patients with severe cardiac failure because the blood flow is slow. Cheyne-Stokes Breathing – Brain Damage • Cheyne-Stokes breathing can also occur in patients with brain damage. In these patients, the response to changes in blood gases is exaggerated. As a result, changes in ventilation overcompensate for changes on blood gases. This is a particularly bad sign, as death often follows this breathing pattern in patients with brain damage. Sleep Apnea • Apnea is the temporary suspension of breathing. • Normally, some episodes of apea occur. In people with sleep apnea, the episodes are longer and more frequent. • 2 types of sleep apnea are: Obstructive sleep apnea Central sleep apnea Obstructive Sleep Apnea • This occurs when the pharynx collapses during sleep. The pharynx is normally held open by muscles, which at night, relax. • In patients with sleep apnea, the pharynx is collapsed while the muscles relax. Some of the factors that cause this collapse include: – Excess fat deposits in the soft tissues of the pharynx or fat masses in the neck. – Nasal obstruction – Enlarged tonsils – Very large tongue – Certain shapes of the palate Symptoms of Obstructive Sleep Apnea • Loud snoring and labored breathing that often progressively worsens. • Long silent periods (apnea) that cause increases in PCO2 and decreases in PO2. • This stimulates respiration, which results in loud snorts and gasps. • This repeats. Central Sleep Apnea • Less common than obstructive sleep apnea. • The CNS signal to the respiratory muscles stops. • Can be caused by damage to the central respiratory center or respiratory neuromuscular junction.