Sensitivity to implant materials in patients with total knee arthroplasties
advertisement

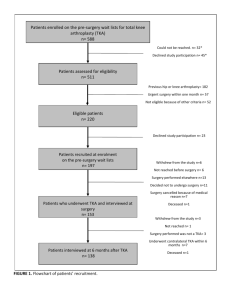
Sensitivity to implant materials in patients with total knee arthroplasties Materials used for total knee arthroplasty (TKA), may elicit an immune response whose role in the outcome of the arthroplasty is still unclear. The aim of this study was to evaluate the frequency of sensitization in patients who had undergone TKA, and the clinical impact of this event on the outcome of the implant Ninety-four subjects were recruited, including 20 patients who had not yet undergone arthroplasty, 27 individuals who had a well-functioning TKA, and 47 patients with loosening of TKA components. Sensitization was detected by using patch testing including haptens representative of cobalt-based alloys (CoCrMo), titanium-based alloys (TiAlV), and bone cements The frequency of positive skin reactions to metals increased significantly after TKA, either stable or loosened (No Implant 20%; Stable TKA 48.1%, p=0.05; Loosened TKA 59.6%, p=0.001, respectively). We found a higher frequency of positive patch testing to vanadium in patients who had a Stable TKA with at least one TiAlV component (39.1%, p=0.01). The medical history for metal allergy seems to be a risk factor, because the TKA failure was fourfold more likely in patients who had symptoms of metal hypersensitivity before TKA. The prognostic value was supported by survival analysis, because in these individuals the outcome of the implant was negatively influenced (the logrank test Chi square 5.1, p=0.02). This study confirms that in patients with a TKA the frequency of positive patch testing is higher than in the normal population, although no predictive value is attributable to the sensitization because patch testing was not able to discriminate between stable and loose implants. On the contrary, the presence of symptoms of metal allergy before implantation should be taken into account as a potential risk factor for TKA failure. At a recent international knee surgery symposium, the attendees were polled to identify how many had observed an allergic reaction in their arthroplasty patients. The result was an unimpressive 11% positive response.1 At the same time, one prosthesis manufacturer that specialized in ceramic knee implants suggested that more than half of all total knee arthroplasty (TKA) revisions are because of hypersensitivity to the cobalt-chromium alloy used in the failed knee implants. The difference is substantial and initiated a controversy about biomaterial allergy. Biomaterial hypersensitivity reactions involve a complex series of steps that elicit a T-lymphocyte cellular response to the antigen.2 This response is significantly different than the antibody response commonly seen in allergic reactions such as allergic rhinitis or hay fever. As implanted metals degrade (and all implanted metals degrade to some degree), the reaction products (ie, particulates, oxides, insoluble salts, and free metal ions) rapidly interact with host proteins in a process known as haptenization. The combination of protein and degradation product may become immunogenic, eliciting the hypersensitivity reaction. As expected, these reactions differ substantially from one material to another, but they also vary significantly among patients. Metal Allergies Nickel has long been identified as a cause of allergic dermatitis, with approximately 11% to 14% of patients in the United States and Canada demonstrating sensitivity.3 Anecdotally, nickel sensitivity seems to be more common in women and also in industrial areas, possibly indicating some form of sensitization. Cobalt sensitivity has been observed in approximately 1% to 2% of the same population, with a significant degree of cross-reactivity between the two metals.4 The first report of an allergic reaction to an orthopedic implant described an eczematous rash over a stainless steel fracture plate.5 Since then, numerous reports documented similar observations, with symptoms of discomfort, erythema, swelling, and skin changes in the general area of the implant.6 In addition, some patients report general malaise, fatigue, or weakness. The majority of reports involve implants manufactured from alloys containing nickel and cobalt.7 On the other hand, three orthopedic metals in particular appear to be nearly inert, both with regard to dermal and implant reactivity. Titanium has a low incidence of immune hypersensitivity, and the reported cases almost always described either alloys containing vanadium, a relatively high concentration of nickel contaminates, or both.8 Tantalum has been reported once as a cause of an allergic response,9 and zirconium has never been shown to induce immune reactions . When the existence of immune hypersensitivity to implanted orthopedic materials is accepted, the surgeon must consider whether the problem is clinically significant. Certainly, the incidence of reactions to implanted metals approaching just 1% of the population does not match the 11% rate of dermal sensitivity, but several other factors must be considered.2 First, most patients who report metal allergies relate the manifestations to inexpensive jewelry. Second, implants such as fracture-fixation devices can be removed when no longer needed. For patients with fracture-fixation devices, the small risk of sensitivity is outweighed by the benefits of surgery. The risk must be considered seriously, however, in patients with a history of dermal sensitivity who are undergoing permanent placement of orthopedic implants such as arthroplasty components. The risk to these patients cannot yet be identified preoperatively in a reliable manner. Detecting Metal Allergies Skin testing is the conventional method of identifying material allergic hypersensitivities. Usually, the patient wears a small billet of metal against the skin for several days to 1 week, and the test result is positive if the area becomes erythematous (Figure 1). Skin testing as it is usually performed is unreliable for several reasons. One key issue is that skin is an excellent barrier, sealing the immune system from direct environmental contact. A better surface for allergy testing would be a mucous membrane such as the oral cavity,10 but placement and maintenance of test samples would be difficult, and they still would not have the same environment of proteins, cellular elements, and pH of a synovial cavity. The inability to implant test material on the joint surface has lead to the development of in vitro testing methods (Figure 1).11-13 Figure 1: Patient showing positive reaction for metal hypersensitivity to “skin test”. Figure 2: Reinforcement buttresses on the alumina ceramic femoral component (Kyocera Inc.; Japan) compared to the conventional geometry of the Oxinium oxidized zirconium alloy femoral component on the left (Smith & Nephew, Memphis, Tenn). The Oxinium implant also has a textured finish that allows for better cement adhesion. Figure 3: A zirconia ceramic femoral component (left) compared to an Oxinium implant. Both show hypoallergenic properties. Currently, there are several in vitro tests for metal sensitivity, based on leukocyte migration or proliferation.3 However, all have limited clinical application, and none are totally reliable. As a result, the issue of material hypersensitivity is most often addressed retrospectively, after the patient has developed symptoms of an immune response. These symptoms often resemble infection, with periincisional erythema, urticaria, effusion, and pain. However, if the infection work-up is negative, with the joint fluid showing few white cells, then the diagnosis is usually made by exclusion. This process is often a frustrating experience for both the surgeon and the patient. Other than revision surgery and removal of the insulting materials, few treatment options exist. Allergy medications are ineffective because they prevent histamine release, not T cell responses. Low-dose corticosteroids may be used as an immune suppressive in making the diagnosis, but their numerous adverse effects make them inappropriate for long-term use. Other biomaterial options may make it possible for most patients with metal hypersensitivity to benefit from TKA. Figure 4: A 56-year-old woman following TKA with a conventional cobalt-chrome femoral component. Metal allergy testing was positive for cobalt-chrome alloy and negative for titanium. Sepsis work-up, including aspiration of the joint, was negative. Range of motion was limited to 80° flexion with a 10° flexion contracture. Figures 5A and 5B: Results for same patient following revision with all-poly tibial insert and ceramic femoral component. The patient has subsequently undergone a primary replacement on the right knee with equally good results using an Oxinium femoral component. (Figures 5A and 5B reprinted from Nasser S. Biology of Foreign Bodies: Tolerence, Osteolysis, and Allergy. In: Bellemans J, Ries MD, Victor JMK, eds. Total Knee Arthroplasty. Heidelberg, Germany; 2005: 343352; Figures 55-8, 55-10B. Copyright © Springer Medizin Verlag Heidelberg 2005. Reprinted with kind permission of Springer Science and Business Media.) Other Options Ceramics, both alumina and zirconia, are among the least reactive biomaterials.14 Ceramic knee femoral components manufactured from both types of ceramic have been available for some time in Europe and Japan. Some designs are currently under evaluation by the US Food and Drug Administration and may soon be available in the United States. When combined with all polyethylene tibial and patellar components, metal can be totally eliminated from the knee replacement. Some characteristics of ceramic implants limit their usefulness. Bioinert ceramics are brittle, and ceramic fractures can occur. As a result, the design and manufacture of ceramic implants often require compromises such as buttresses to support posterior condyles and gentle curves rather than sharp angles that can act as stress risers (Figure 2). In addition, ceramic femoral heads are substantially more expensive than those made of cobalt-chromium alloys. Oxinium oxidized zirconium implants (Smith & Nephew; Memphis, Tenn) are an option for unicompartmental, patellofemoral, and TKA (Figure 3). Oxinium has a base of 97.5% zirconium/2.5% niobium that is surface oxidized to zirconia, forming a metal/ceramic composite. Oxidized zirconium has the hypoallergenic properties of ceramics15 without the adverse material properties and can cost less than ceramics. Preliminary studies show Oxinium particulate is as inert as zirconia and alumina ceramics. A recent clinical comparison of Oxinium femoral implants with alumina and zirconia ceramics implants showed no difference in immune response, including response in revision cases in which the Oxinium implants replaced ceramic components placed for reasons of metal allergy (Figures 4 and 5).15 Conclusion Several studies show that immune hypersensitivity to implanted biomaterials is more common in patients with failed joint prostheses than in patients with stable implants.16-18 The obvious question is “do failing or loose implants stimulate the immune system to generate this response, or do some patients have a preexisting sensitivity that leads to implant failure?” If the first is the case, then it may soon be possible to modify the immune response by using medications or gene therapy, for example, to limit osteolysis and material hypersensitivity. It may also be possible in the near future to determine which materials are appropriate for the individual patient to avoid provoking the immune response. Such an integration of material science with immunology can only serve to improve total joint replacement surgery in the future. Inflammatory Arthritis Following Total Knee Arthroplasty Researchers writing in the Journal of biomedical materials research. Part A; say "Joint effusion after total knee arthroplasty (TKA) is considered as a manifestation of certain inflammatory reactions within prosthetic joints," and investigated causes of joint effusion following TKA. Niki Y, Matsumoto H, Otani T, Tomatsu T, Toyama Y. Five types of inflammatory arthritis following total knee arthroplasty. J Biomed Mater Res A. 2007 Jun 15;81(4):1005-10. Joint effusion after total knee arthroplasty (TKA) is considered as a manifestation of certain inflammatory reactions within prosthetic joints. This study investigated causes of joint effusion following TKA and analyzed phenotypic characteristics of synovial fluid leukocytes for each cause. Forty-six TKAs for rheumatoid arthritis (RA) and 49 TKAs for osteoarthritis (OA) displaying joint effusion were investigated. Causes of joint effusion were clinically identified and frequencies of each cause were compared between RA and OA. Synovial fluid cell phenotypes were analyzed using a fluorescence-activated cell sorter. Clinical diagnoses for joint effusion were classified into five different groups: deep infection (DI); increased activity of RA (IRA); particle-induced synovitis (PS); metal sensitivity (MS); and nonspecific synovitis (NS). The most frequent cause of post-TKA effusion was IRA in RA, and NS in OA. Biomaterial-related arthritis such as PS and MS were more frequent with OA than with RA. Analysis of synovial fluid cell phenotypes revealed that the characteristic cells for each diagnosis were CD16(+)CD14(-) neutrophils in IRA and DI, CD14(+) macrophages in PS, and CD3(+)CD45RO(+) T cells in MS. Post-TKA joint effusion is clinically caused by five different types of arthritis. Phenotypic characteristics of synovial fluid leukocytes reflect joint pathology and contribute to diagnosis and exclusion of biomaterial-related arthritis. 2007 Wiley Periodicals, Inc. J Biomed Mater Res, 2007. Sensitivity to implant materials in patients with total knee arthroplasties. Granchi D, Cenni E, Tigani D, Trisolino G, Baldini N, Giunti A. Laboratory for Pathophysiology of Orthopedic Implants, Istituti Ortopedici Rizzoli, via di Barbiano 1/10, 40136 Bologna, Italy. donatella.granchi@ior.it <donatella.granchi@ior.it> Materials used for total knee arthroplasty (TKA), may elicit an immune response whose role in the outcome of the arthroplasty is still unclear. The aim of this study was to evaluate the frequency of sensitization in patients who had undergone TKA, and the clinical impact of this event on the outcome of the implant. Ninety-four subjects were recruited, including 20 patients who had not yet undergone arthroplasty, 27 individuals who had a well-functioning TKA, and 47 patients with loosening of TKA components. Sensitization was detected by using patch testing including haptens representative of cobalt-based alloys (CoCrMo), titanium-based alloys (TiAlV), and bone cements. The frequency of positive skin reactions to metals increased significantly after TKA, either stable or loosened (No Implant 20%; Stable TKA 48.1%, p=0.05; Loosened TKA 59.6%, p=0.001, respectively). We found a higher frequency of positive patch testing to vanadium in patients who had a Stable TKA with at least one TiAlV component (39.1%, p=0.01). The medical history for metal allergy seems to be a risk factor, because the TKA failure was fourfold more likely in patients who had symptoms of metal hypersensitivity before TKA. The prognostic value was supported by survival analysis, because in these individuals the outcome of the implant was negatively influenced (the logrank test Chi square 5.1, p=0.02). This study confirms that in patients with a TKA the frequency of positive patch testing is higher than in the normal population, although no predictive value is attributable to the sensitization because patch testing was not able to discriminate between stable and loose implants. On the contrary, the presence of symptoms of metal allergy before implantation should be taken into account as a potential risk factor for TKA failure. [Prevalence of allergic reactions to implant materials in total hip and knee arthroplasty] [Article in German] Schuh A, Lill C, Hönle W, Effenberger H. Research Unit Orthopädie und Chirurgie, Klinikum Neumarkt, Akademisches Lehrkrankenhaus der Friedrich-Alexander-Universität Erlangen-Nürnberg. Alexander.Schuh@klinikum.neumarkt.de INTRODUCTION: Several case reports have been published on allergic reactions like eczema, urticaria, persistent swelling, sterile osteomyelitis or aseptic implant loosening in the context of orthopaedic implants. There is, however, a lack of data concerning incidence or prevalence of allergies in this special group of patients. The aim of this study was to analyse a consecutive series of patients with a total hip or knee arthroplasty to gain information about prevalence of allergic reactions to constituents of the alloys or bone cement. MATERIAL AND METHOD: Between February and September 2005, a consecutive series of 300 patients after total hip (THA) or total knee (TKA) arthoplasty were interviewed during regular follow-up using the standardised questionnaire of the working group 20 "Implant and Allergy" of the DGOOC with respect to allergies, especially to different metals or constituents of bone cement. In this study 100 males and 200 females with 214 THA and 86 TKA were included. The mean follow-up time was 33.3 months (min: 3, max: 174). RESULTS: Different allergies were found in 39 patients. In 12 cases (4 %) allergic reactions against nickel, in 4 cases (1.3 %) against cobalt, in 2 cases (0.7 %) against chromium and in 2 cases (0.7 %) against benzoyl peroxide were detected by means of epicutaneous testing. One patient each suffering from a nickel allergy showed signs of osteolysis or recurrent effusion after THA with a metal-on-metal bearing. One patient each suffering from recurrent effusion or eczema following TKA showed allergic reactions to benzoyl peroxide. In all the other patients with allergies to the alloy constituents, the follow-up was uneventful. CONCLUSION: The prevalence of allergic reactions in an unselected group of orthopaedic patients is significantly lower in comparison to that in dermatological studies. Most patients suffering from allergies tolerated the implant uneventfully. Further studies are needed to identify those groups of patients with allergies who may not tolerate the implant in order to provide better care or use special implants. [Prevalence of allergic reactions to implant materials in total hip and knee arthroplasty] [Article in German] Schuh A, Lill C, Hönle W, Effenberger H. Research Unit Orthopädie und Chirurgie, Klinikum Neumarkt, Akademisches Lehrkrankenhaus der Friedrich-Alexander-Universität Erlangen-Nürnberg. Alexander.Schuh@klinikum.neumarkt.de INTRODUCTION: Several case reports have been published on allergic reactions like eczema, urticaria, persistent swelling, sterile osteomyelitis or aseptic implant loosening in the context of orthopaedic implants. There is, however, a lack of data concerning incidence or prevalence of allergies in this special group of patients. The aim of this study was to analyse a consecutive series of patients with a total hip or knee arthroplasty to gain information about prevalence of allergic reactions to constituents of the alloys or bone cement. MATERIAL AND METHOD: Between February and September 2005, a consecutive series of 300 patients after total hip (THA) or total knee (TKA) arthoplasty were interviewed during regular follow-up using the standardised questionnaire of the working group 20 "Implant and Allergy" of the DGOOC with respect to allergies, especially to different metals or constituents of bone cement. In this study 100 males and 200 females with 214 THA and 86 TKA were included. The mean follow-up time was 33.3 months (min: 3, max: 174). RESULTS: Different allergies were found in 39 patients. In 12 cases (4 %) allergic reactions against nickel, in 4 cases (1.3 %) against cobalt, in 2 cases (0.7 %) against chromium and in 2 cases (0.7 %) against benzoyl peroxide were detected by means of epicutaneous testing. One patient each suffering from a nickel allergy showed signs of osteolysis or recurrent effusion after THA with a metal-on-metal bearing. One patient each suffering from recurrent effusion or eczema following TKA showed allergic reactions to benzoyl peroxide. In all the other patients with allergies to the alloy constituents, the follow-up was uneventful. CONCLUSION: The prevalence of allergic reactions in an unselected group of orthopaedic patients is significantly lower in comparison to that in dermatological studies. Most patients suffering from allergies tolerated the implant uneventfully. Further studies are needed to identify those groups of patients with allergies who may not tolerate the implant in order to provide better care or use special implants. Sensitivity to implant materials in patients with total knee arthroplasties References and further reading may be available for this article. To view references and further reading you must purchase this article. Donatella Granchia, , , Elisabetta Cennia, Domenico Tiganib, Giovanni Trisolinob, Nicola Baldinia, b and Armando Giuntia, b for Pathophysiology of Orthopedic Implants, Istituti Ortopedici Rizzoli, via di Barbiano 1/10, 40136 Bologna, Italy bDepartment of Orthopedics and Traumatology, Istituti Ortopedici Rizzoli, Bologna, Italy aLaboratory Received 26 September 2007; accepted 27 November 2007. Available online 21 December 2007. Abstract Materials used for total knee arthroplasty (TKA), may elicit an immune response whose role in the outcome of the arthroplasty is still unclear. The aim of this study was to evaluate the frequency of sensitization in patients who had undergone TKA, and the clinical impact of this event on the outcome of the implant. Ninety-four subjects were recruited, including 20 patients who had not yet undergone arthroplasty, 27 individuals who had a well-functioning TKA, and 47 patients with loosening of TKA components. Sensitization was detected by using patch testing including haptens representative of cobalt-based alloys (CoCrMo), titanium-based alloys (TiAlV), and bone cements. The frequency of positive skin reactions to metals increased significantly after TKA, either stable or loosened (No Implant 20%; Stable TKA 48.1%, p = 0.05; Loosened TKA 59.6%, p = 0.001, respectively). We found a higher frequency of positive patch testing to vanadium in patients who had a Stable TKA with at least one TiAlV component (39.1%, p = 0.01). The medical history for metal allergy seems to be a risk factor, because the TKA failure was fourfold more likely in patients who had symptoms of metal hypersensitivity before TKA. The prognostic value was supported by survival analysis, because in these individuals the outcome of the implant was negatively influenced (the logrank test Chi square 5.1, p = 0.02). This study confirms that in patients with a TKA the frequency of positive patch testing is higher than in the normal population, although no predictive value is attributable to the sensitization because patch testing was not able to discriminate between stable and loose implants. On the contrary, the presence of symptoms of metal allergy before implantation should be taken into account as a potential risk factor for TKA failure. Keywords: Knee replacement; Hypersensitivity; Cobalt alloy; Titanium alloy Screening for symptomatic metal sensitivity: a prospective study of 92 patients undergoing total knee arthroplasty References and further reading may be available for this article. To view references and further reading you must purchase this article. Yasuo Niki, , a, Hideo Matsumotoa, Toshiro Otania, Taku Yatabea, Makoto Kondob, Fumihiro Yoshiminec and Yoshiaki Toyamaa a Department of Orthopaedic Surgery, Keio University, 35, Shinanomachi, Shinjuku-ku, Tokyo 160-8582, Japan b Department of Orthopaedic Surgery, Kashiba-asahigaoka Hospital, 834-3 Uenaka, Kashiba-shi, Nara-ken 639-0265, Japan c Department of Orthopaedic Surgery, Tokyo Metropolitan Ohkubo Hospital, 2-44-1 Kabukicho, Shinjuku-ku, Tokyo 160-8488, Japan Received 11 November 2003; accepted 29 March 2004. Available online 25 May 2004. Abstract Metal sensitivity (MS) reactions to implant metals represent a rare but well-documented complication following total joint arthroplasty (TJA). Although 20–25% of post-TJA patients develop MS, only a few highly susceptible patients (<1%) exhibit symptoms. Whether surgeons should perform screening for MS is currently a matter of debate. The present study investigated the clinical importance of screening for patients predisposed to symptomatic MS, and the specific metals causing symptomatic MS following total knee arthroplasty (TKA). Between 2000 and 2002, a total of 108 primary TKAs were performed on 92 patients. Preoperatively, all patients underwent modified lymphocyte stimulation test (mLST) to Ni, Co, Cr, and Fe. Of the 92 patients, 24 (26%) displayed positive preoperative responses to at least one metal. Five patients displayed implant metal-related eczema and were all mLST-positive preoperatively, suggesting that screening for symptomatic MS is clinically useful. Two of these underwent revision TKA and thereafter, eczema healed and mLST results changed from positive to negative. All mLSTpositive patients were divided into three groups: Group I, patients with eczema; Group II, patients with clear history of MS; and Group III, patients neither eczema nor history of MS. When the type of sensitive metals were compared among the three groups, a significant association between presence of Cr-sensitivity and development of eczema (P<0.05) was identified. No significant association was observed between other metals and development of eczema or history of MS. This indicates that Cr is a potential candidate metal for causing eczema in our TKA series, and Cr-sensitivity may offer a potential predictor for symptomatic MS. The present study indicates that the surgeons should undertake routine preoperative screening for MS, particularly to Cr. Orthopaedic implant related metal toxicity in terms of human lymphocyte reactivity to metal-protein complexes produced from cobaltbase and titanium-base implant alloy degradation Authors: Hallab N.J.1; Mikecz K.2; Vermes C.2; Skipor A.2; Jacobs J.J.2 Source: Molecular and Cellular Biochemistry, Volume 222, Numbers 1-2, June 2001 , pp. 127-136(10) Publisher: Springer < previous article | next article > | view table of contents Key: - Free Content - New Content - Subscribed Content - Free Trial Content Abstract: Metal toxicity from sources such as orthopaedic implants was investigated in terms of immune system hyper-reactivity to metal implant alloy degradation products. Lymphocyte response to serum protein complexed with metal from implant alloy degradation was investigated in this in vitro study using primary human lymphocytes from healthy volunteers (n = 10). Cobalt chromium molybdenum alloy (Co-Cr-Mo, ASTM F75) and titanium alloy (Ti-6Al-4V, ASTM F-136) beads (70 m) were incubated in agitated human serum at 37 degrees Celsius to simulate naturally occurring metal implant alloy degradation processes. Particulate free serum samples, which were incubated with metal, were then separated into molecular weight based fractions. The amounts of soluble Cr and Ti within each serum fraction were measured and correlated with lymphocyte proliferation response to the individual serum fractions. Lymphocytes from each subject were cultured with 11 autologous molecular weight based serum fractions either with or without added metal. Two molecular weight ranges of human serum proteins were associated with the binding of Cr and Ti from Co-Cr-Mo and Ti implant alloy degradation (at < 30 and 180–330 kDa). High molecular weight serum proteins ( 180 kDa) demonstrated greater lymphocyte reactivity when complexed with metal released from Co-Cr-Mo alloy and Ti alloy than with low (5–30 kDa) and midrange (30–77 kDa) serum proteins. When the amount of lymphocyte stimulation was normalized to both the moles of metal and the moles of protein within each fraction (Metal-Protein Complex Reactivity Index, MPCRI), Cr from Co-Cr-Mo alloy degradation demonstrated approximately 10 fold greater reactivity than Ti in the higher molecular weight serum proteins ( 180–250 kDa). This in vitro study demonstrated a lymphocyte proliferative response to both Co-Cr-Mo and Ti alloy metalloprotein degradation products. This response was greatest when the metals were complexed with high molecular weight proteins, and with metal-protein complexes formed from Co-Cr-Mo alloy degradation. Titre du document / Document title Phenotypic characteristics of joint fluid cells from patients with continuous joint effusion after total knee arthroplasty Auteur(s) / Author(s) NIKI Yasuo ; MATSUMOTO Hideo ; OTANI Toshiro ; YATABE Taku ; FUNAYAMA Atsushi ; MAENO Shinichi ; TOMATSU Taisuke ; TOYAMA Yoshiaki ; Résumé / Abstract Joint effusion after total joint arthroplasty (TJA) is a manifestation of inflammatory reactions within the prosthetic joint. Among the various causes for joint effusion following TJA, deep infection (DI), wear particle-induced synovitis (PS) and metal sensitivity to the implant should be excluded as soon as possible, as these may result in the failure of TJA. The present study analyzed joint fluid cells from patients after total knee arthroplasty (TKA) using fluorescence-activated cell sorter (FACS), and examined the feasibility of using FACS to exclude the possibility of biomaterial-related complication. A total of 72TKAs from 64 patients suffering from joint effusion were examined in this study. Joint fluid was aspirated in outpatient clinics and applied to FACS. The results indicated that patients could be clearly classified into four types based on forward/side scatter profiles. Analysis of specific CD markers revealed that leukocytes were selectively recruited from blood to inflamed prosthetic joints. Dominant cell types were CD16+neutrophils in DI and increased rheumatoid activity, CD14+macrophages in PS, and CD3+CD45RO+T cells in metal sensitivity. These findings suggest the feasibility of diagnosing joint effusion by analyzing dominant cell type recruited using FACS. In conclusion, FACS may offer a useful tool for analyzing joint fluid cells from post-TJA patients and for excluding biomaterial-related complication following TJA. Revue / Journal Title Biomaterials ISSN 0142-9612 Source / Source 2006, vol. 27, no8, pp. 1558-1565 [8 page(s) (article)] Langue / Language Anglais Editeur / Publisher Elsevier Science, Oxford, ROYAUME-UNI (1980) (Revue)