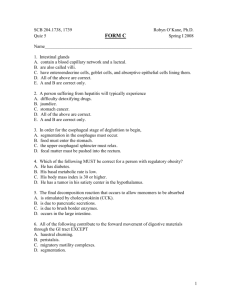
Gastrointestinal Hormones
advertisement

Gastrointestinal Hormones Overview of the GI Tract Digestion and Absorption Regulation of Digestive Functions GI Hormones and Paracrine Factors Integration of Neural and Endocrine Signals Signaling Mechanisms Functions of the GI Tract Ingestion: Taking in food Digestion: Chemical and Mechanical Absorption: moving nutrients from the lumen of the GI tract into the cells of the body Excretion: getting rid of undigested and unabsorbed material Movement: movement of ingested food throughout the GI tract Organs of the Digestive System Accessory Digestive Organs: Salivary glands Liver, gall bladder Pancreas Digestive Tract: Oral Cavity Pharynx Esophagus Stomach Small Intestine Large Intestine The Oral Cavity Boundaries are: - lips (anteriorly) - cheeks (laterally) - palate (superiorly) The oral cavity is important in: - mastication (chewing): mechanical digestion - secretion of saliva for digestion (amylase; digests starch), coating food (mucus) - no significant absorption of nutrients occurs in the oral cavity The Pharynx The pharynx is the passageway from the nose and mouth to the esophagus and respiratory tract Boundaries: uvula to epiglottis During swallowing, food is directed from pharynx to esophagus (away from respiratory tract). Esophagus The esophagus is a passageway from the pharynx to stomach Contains two sphincters: upper and lower esophageal sphincters (controls flow) Upper sphincter is skeletal (voluntary), lower sphincter is smooth muscle (involuntary) Peristaltic waves move food from pharynx to stomach. The Stomach The stomach stores food, and mixes and mechanically and chemically digests it The stomach also secretes digestive juices pepsin: digests protein hydrochloric acid (acidic pH, required for pepsin activity, and to kill ingested bacteria) Mucus: protects the stomach wall Partially digested food: chyme Little absorption occurs in the stomach (exceptions: alcohol, aspirin…) Histology of the Stomach Cell types: Chief cells: produce pepsinogen (inactive precursor to pepsin) Parietal cells: produce HCl and intrinsic factor (absorption of vitamin B12; important in RBC maturation) “Endocrine” cells: G cells: gastrin D cells: somatostatin (paracrine) Enterochromaffin-like cells: histamine (paracrine) Small Intestine Connects the stomach with the large intestine It is the major site of digestion It is also the major site of absorption Specialized structures (villi, microvilli) increase the surface area of the small intestine, aiding absorption. The small intestine has three parts (duodenum, jejunum, and ileum) The bile duct (from liver) and pancreatic duct (digestive juices) empty into the duodenum. Histology of the Small Intestine Absorptive cells Goblet cells (mucus) Enteroendocrine cells: secretin cholecystokinin Digestion & Absorption: Carbohydrates Carbohydrates: small amount of digestion begins in oral cavity (amylase). Most digestion in small intestine: Enzyme Digests pancreatic amylase polysaccharides to disaccharides disaccharidases disaccharides into (small intestine) monosaccharides What’s absorbed: monosaccharides Digestion & Absorption: Proteins Proteins: Digestion begins in stomach (pepsin), continues in small intestine: Enzyme Digests trypsin, chymotrypsin, polypeptides into carboxypeptidase small peptides (from pancreas) aminopeptidase dipeptidases small peptides into smaller peptides What’s absorbed: mono-, di-, and tri-peptides Digestion & Absorption : Lipids Lipids: Digestion begins in the small intestine (minor amount in oral cavity) Note: Lipids are not soluble in water. Thus, it is hard for enzymes to act on them. The first step in lipid digestion is emulsification of lipids with bile (secreted from the liver). Emulsification: transformation of large lipid droplets into small lipid droplets. This increases the surface area of lipid that can be acted on by the digestive enzyme, pancreatic lipase. Emulsification of Lipids by Bile Bile acts on lipids in a way similar to detergent acting on greasy water: large lipid droplet bile lipase Absorption of Lipids Bile also helps absorption of products of lipid digestion, forming micelles (free fatty acids, glycerol, cholesterol). Absorption of lipids is required for absorption of fat-soluble vitamins (vitamins A, D, E, K) Digestion and Absorption: Nucleic Acids Food also contains RNA and DNA (also from shed cells of the GI tract). The pancreas releases nucleases into the small intestine. Nucleases digest RNA and DNA into components. Digestion and absorption of dietary nucleic acids probably not important for DNA/RNA synthesis. Absorption in the Small Intestine: Water About 9 liters of water enters the digestive tract each day. About 8 liters of this is absorbed by the small intestine (by osmosis, following movement of ions). Large Intestine Last portion of the digestive tract. No digestion occurs in the large intestine. In the large intestine, there is absorption of water (about 1 liter/day) and salts from feces (undigested, unabsorbed food). Bacteria produce vitamin K, B vitamins. Secretion of mucus (lubrication of feces) Contractions move feces along large intestine and rectum, to be expelled out of the anal canal. Accessory Digestive Organs Pancreas: exocrine portion produces digestive enzymes, bicarbonate Liver: Produces bile, stores glycogen, interconverts nutrients (gluconeogenesis), detoxifies toxic substances (alcohol, drugs, ammonia…), makes blood proteins (albumin, fibrinogen, clotting factors) Gallbladder: concentrates and stores bile Regulation of Digestion Allow communication between different parts of the digestive tract Ensure the presence of sufficient secretions when food present Help avoid overabundance of secretions in absence of food Two types of mechanisms: neural and endocrine Neural Control of Digestion Neural control of digestion is controlled largely by the parasympathetic nervous system, and local (enteric) reflexes. Activation of the parasympathetic system results in secretion of digestive juices, increased motility of the stomach, and slowing down movement of food from the stomach to small intestine. Stimuli: Thought, sight, taste of smell of food; distension of GI tract; chemoreceptors detecting nutrients, pH. Example: Thought, chewing, or taste of food activates parasympathetic system, resulting in increased release of mucus, HCl, and pepsin in the stomach. The goal of this is to prepare the stomach for oncoming food. Intestinal Phase of Gastric Secretion (~ 10% of total) (due to some G cells extending from antrum into the duodenum) Important aspect of intestinal phase is feedback regulation and inhibition Involves interactions between duodenal contents and duodenal hormones, including their actions on pancreas, liver, gall bladder, and stomach B. Functional Phases of Gastric Secretion 2. Gastric Phase of 1. Cephalic Phase of Gastric Secretion (approx. 30% of total) Gastric Secretion (approx 60% of total) (initiated by brain) (initiated by gastric events) vagus nerve vagus nerve FOOD HCl HCl Distension Peptides circulation G circulation G gastrin gastrin C. G.I. HORMONES + + + + + H+ psnogn motil. LES growth + + + - Gastrin (17 AA) HCO3 output psnogn synrg w/ CCK gastr emptying H+ Cholecystokinin (CCK (33 AA)) + + + - Structure of Secretin (27 AA) (comparison with other GI hormones) panc enz G.B. growth Oddi gastr emptying synrg w/ Secretin Endocrine Control of Digestion Gastrin: - produced from the stomach (G cells) - release increased by stomach distension, peptides, amino acids, alcohol, caffeine, parasympathetic innervation - release inhibited by highly acidic pH (< 2.0) - functions: increases gastric (stomach) secretions (primarily HCl); increases histamine release; increases gastric motility; opens pyloric sphincter (between stomach and small intestine), relaxes ileocecal sphincter, stimulates growth of gastric mucosa. Endocrine Control of Digestion Histamine: Produced by enterochromaffin-like cells (ECL cells) of the stomach. Release is stimulated by gastrin. Action: increase HCl secretion from parietal cells (major factor in HCl secretion). HOW IT WORKS AT THE RECEPTOR LEVEL Combined neurocrine, endocrine and paracrine events in the activation of gastric HCl secretion Acetylcholine neural input neurocrine ACh receptor PARIETAL cell histamine receptor H/K P ECL cell transductionactivation events histaminesecreting cell HCl secretion H/K P gastrin receptor Gastrin hormonal input endocrine paracrine release of histamine ECL cell = enterochromaffin-like cell G cell = gastrin-secreting cell G cell HOW IT WORKS AT THE RECEPTOR LEVEL Combined neurocrine, endocrine and paracrine events in the activation of gastric HCl secretion Acetylcholine neural input neurocrine ACh receptor PARIETAL cell histamine receptor H/K P ECL cell HCl transductionactivation events histaminesecreting cell secretion H/K P gastrin receptor Gastrin hormonal input endocrine paracrine release of histamine G cell H-2 receptor blockers Tagamet ECL cell = Zantac enterochromaffin-like cell Pepcid H/K ATPase pump G cell = inhibitors gastrin-secreting cell Prilosec Nexium Aciphex Turning the G-cell On and Off vagus nerve ACh gastric mucosa ACh ACh - GRP cell (Gastrin) SS + H+ + G D (Somatostatin) Gastric Lumen GRP neuron cholinergic neuron cell + digested protein Gastric Lumen Circulating Gastrin Turning the G-cell On and Off vagus nerve ACh gastric mucosa ACh GRP neuron cholinergic neuron GRP ACh D (Somatostatin) cell SS + H+ Circulating Gastrin + G (Gastrin) cell + digested protein Gastric Lumen SS = somatostatin Endocrine Control of Digestion Somatostatin Produced by D cells of the stomach Secretion is stimulated by activation of the sympathetic nervous system and by acidic pH, and is inhibited by activation of the parasympathetic nervous system, continuously released, overridden by gastrin and nerves. Actions: inhibit gastrin and histamine secretion (decreased acid release and gastric motility); also directly inhibits acid release from parietal cells. Endocrine Control of Digestion Secretin: - Produced by duodenum (enteroendocrine cells of the small intestine); crypts of Lieberkühn - stimulated by arrival of acidic chyme in duodenum. - functions: stimulates bicarbonate secretion from pancreas; inhibits gastric secretion (decreases HCl production by inhibiting gastrin release); decreases gastric motility (slowing rate of gastric digestion and delivery to the small intestine), increases hepatic bile production, increases CCK, promotes growth and maintenance of the pancreas. Endocrine Control of Digestion Cholecystokinin (CCK): - produced by enteroendocrine cells of the duodenum - release stimulated by fatty acids in duodenum (also amino acids, acidic chyme) - functions: causes gallbladder contraction (bile to small intestine); stimulates release of pancreatic enzymes; decreases gastric motility and secretion (increases somatostatin release). Endocrine Control of Digestion Gastric Inhibitory Peptide (GIP): Secretion: Enteroendocrine cells in the small intestine mucosa Crypts of Lieberkuhn Stimulus: Chyme rich in triglycerides, fatty acids, and glucose enter the small intestine. Actions: Stimulates release of insulin by beta cells Inhibits gastric secretion and motility Stimulates lipogenesis by adipose tissue Stimulates glucose use by skeletal muscle cells Endocrine Control of Digestion Vasoactive Intestinal Peptide (VIP): Secretion: Enteroendocrine cells in the small intestine mucosa Crypts of Lieberkuhn Stimulus: Chyme entering the small intestine. Actions: Stimulates buffer secretion Inhibits gastric secretion Dilates intestinal capillaries Control of Gastric Acid Secretion How does a parietal cell secrete hydrochloric acid? H+ Cl- CO2 + H20 H2CO3 H+ + HCO3- HCO3- Cl- Control of Gastric Acid Secretion D Cell CCK SECRETIN somatostatin (-) G Cell Gastrin ECL histamine HCl parietal cell Integration of Neural and Endocrine Functions: Central Effects CNS: Thoughts, taste, smell of food; chewing – activates parasympathetic nervous system (neurotransmitter: acetylcholine). ACh acts directly on parietal cells to increase acid secretion. Ach increases gastrin release, inhibits somatostatin release (increased gastric secretion and motility). Sympathetic input (activity, stress): increased somatostatin release (inhibiting gastrin secretion – decreased gastric secretion and motility) Integration of Neural and Endocrine Functions Vagus N. ACh (-) D Cell CCK SECRETIN somatostatin (-) G Cell Gastrin (+) Digested protein ECL histamine (+) (+) HCl parietal cell Integration of Neural and Endocrine Functions: Local Reflexes Mechanoreceptors in the walls of the GI tract detect movement of food into an organ Example: In the stomach distension causes activation of the parasympathetic system, increasing gastrin secretion and acid release, and decreasing somatostatin secretion. Chemoreceptors detect nutrients and pH. Example: Presence of amino acids, alcohol, or caffeine in the stomach increases gastrin release. Presence of fatty acids in the duodenum causes release of CCK. Signaling Mechanisms Histamine: Receptor coupled to Gs – increases cyclic AMP production and acts via PKA. Results in phosphorylation and increased transport of proton pumps to cell membrane. Gastrin: Receptor coupled to Go/IP3/DAG; increased intracellular calcium, and activation of PKC (PKC also phosphorylates proton pumps). Somatostatin: Receptor coupled to Gi – inhibits cyclic AMP production, decreasing PKA signaling. Signaling Mechanisms CCK: Receptor coupled to Go (increased calcium causes somatostatin release) Secretin: Receptor couple to Gs (increased cyclic AMP, causes increased secretion of bicarbonate from the pancreas) Integration of Gastric Secretion + + + + + + Integration of Gastric Secretion - + + - - + + + + + + D. Duodenal Integration & Control: 1. Response to Acidity Regulation by Secretin liver + HCO3 + gall bladder - HCl motility NaCl + H2O HCl + HCl HCl + NaHCO3 NaCl + CO2 + H2O 2. Duodenal Response to Food Regulation by CCK (Cholecystokinin) liver Bile gall + + bladder fat & protein digestion - HCl bile & enzymes fats & peptides FOOD