Critical Appraisal and updates of Interventions in the ED
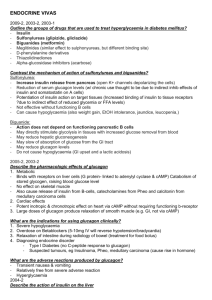
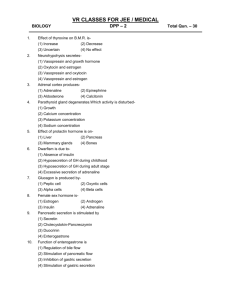
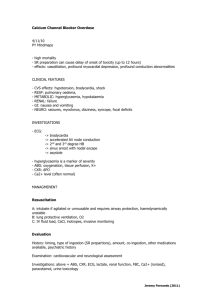
advertisement

Briefly discuss a rational ED approach to poisoning patients Assess level of evidence of toxicologic interventions to provide rational ED management Updates on management of specific xenobiotics requiring critical care at ED Poisoning has been likened to trauma on the cellular level, destroying the natural workings of a victim’s physiology Vanden Hoek et al (2010) Circulation: http://circ.ahajournals.org Emergency Department Intervention of acute poisoning: 90% of cases in a nutshell Gastrointestinal decontamination techniques Investigations Antidotes Increasing Elimination Disposition 10% Immediate care: BLS and Acute cardiac life support The evidence for recommendations : I: Definitely recommended. Definitive, excellent evidence provides support. II: Acceptable and useful. Good evidence provides support. III: May be acceptable, possibly useful. Fair-to-good evidence provides support. Indeterminate: Continuing area of research. Determine the need for lavage or charcoal Serious overdose presenting to the ED within one hour? Potentially serious overdose presenting to ED after one hour? Determine whether toxin is adsorbed to charcoal Routine administration in nontoxic ingestion is not indicated Determine the need for whole bowel irrigation: • Large ingestion of iron, heavy metals, lithium and other drugs poorly adsorbed by activated charcoal • Drug packets (body packers) Suicide attempt • • • • Gather lavage if life-threatening overdose within one hour of ED arrival (carries risk of aspiration , esophageal perforation) Class Interderminate Activated Charcoal 1 g/kg or 10:1 ratio of charcoal to toxin (Class II) MDAC: Antimalarials, Aminophylline, Barbiturates, Beta Blockers (Class II-III) Polyethelene glycol (1-2L in adults, 25 cc/kg in children orally by NG Tube (Class III) Determine suicide risk (Class I-II) Restrain as needed (Class II) Drug levels ECG? Yes, if Yes, if Xray ? • Cardiotoxin ingestion (known or potential • Chest pain or shortness of breath • Abnormal heart rate or hypotension • Any unstable patient (Class II) Chest x-ray (Class I-II) • Dyspnea , tachynea, coma, or obtundation • Cyanosis • Symptomatic patients who ingest: opiods, phenobarbital, phenothiazines and salicylates KUB – suspected metals or drug packets (Class II) Enteric coated preparations Cocaine /opiate packets Arsenic other heavy metals • • • • • • • • Diagnostics/Labs Abnormal vital signs Altered mental status Symptomatic patients and unknown toxin Ingestion of substance that can produce metabolic acidosis Toxic alcohol? Cyanosis or respiratory distress Suspected rhabdomyolysis Female of childbearing age CBG Electrolytes Serum osmolality, anion gap ABG CPK Pregnancy test, urinalysis Yes, if TOXICOLOGY SCREEN? Yes, if Need for antidote? Yes, if Dialysis? Yes, if Toxicology Screen Qualitative/Quantitative: plasma drug concentrations of : o Paracetamol o Salicylates :Symptomatic patient with o Iron of (Class II) ingestion Isopropanol o Lithium Specific Agents Salicylates o Ethylene glycol Theophylline Uremia o MEDICOLEGAL PURPOSES Methanol Barbiturates, beta blockers Lithium Ethylene Glycol AGENT paracetamol Anticholinergics benzodiazepines Beta blockers carbamates digoxin Ethylene glycol ANTIDOTES N-Acetylcysteine Physostigmine Flumazenil Glucagon Atropint AGENT ANTIDOTES iron Deferoxamine Isoniazid Pyridoxine metals BAL, EDTA, DMSA Nitrates/nitrites Methylene blue opiates Naloxone, nalmeferne Fab Fragments organophosphates Atropine, pralidoxime Ethanol, fomefizole snales Antivenin,crofab TOXICOLOGY UPDATES: Caveats: Patients may not be able to provide acute history of exposure to a toxic substance In cases of suicide attempts, multiple substance exposure Comprehensive toxicology laboratory testing is never available on time Basic life support and ACLS current standards should be followed, except for toxin-specific interventions recommended once with ROSC Hypotension Arrhythmia seizures A clinical syndrome – a constellation of signs , symptoms, and laboratory findings – suggestive of the effects of a specific toxin. THINK! Toxidrome Approach: Tachycardia/ hypertention Bradycardia/ hypotention Cardiac conduction delays (wide QRS) • Amphetamines* anticholinergic drugs*antihistamines*cocaine*theophylline/caffeine • Beta blockers/calcium channel blockers; clonidine, digoxin, and related glycosides, organophosphates and carbamates • Cocaine/ tricyclic antidepressants, local anethetics, antiarrythmics (quinidine, flecanide) seizures • Cyclic antidepressants;isoniazid; selective and nonselective norepinephrine reuptake inhibitors; withdrawal states CNS or respiratory depression • Antidepressants, benzodiazepines, carbon monoxide, ethanol, methanol, opiods, oral hypoglycemics Metabolic acidosis • Cyanide, ethylene glycol, metformin, methanol and salicylates Intravenous fluids NOREPINEPHRINE Peripheral vasodilation Opioids Beta blockers digoxin Epinephrine for myocardial depressants Greene et al (2005) Postgrad Med J; 81:204216 Naloxone Glucagon Digoxin specific antibodies Anti arrythmics : not first line agents Proarrythmics Electrical Cardioversion May produce asystole in a poisoned myocardium Correction of: Acidosis Hypokalemia Hypomagnesemia Hypoxia Immediate antidotal therapy Watch out for : conduction delays (widened QRS) Torsade de pointes Greene et al (2005) Postgrad Med J; 81:204-216 Benzodiazepines as first line agents Agitation: avoid phenothiazines or butyrophenones Resistant seizures: General anesthetics: IV barbiturates Supportive care (intubation and mechanical ventilation) Caveats: NO PHENYTOIN for: TCAs and cocaine •has sodium channel blocking properties Benzodiazepines (BZD) exert their action by potentiating the activity of Gamma-aminobutyric acid (GABA) is the major inhibitory neurotransmitter in the CNS Flumazenil as an antidote Evidence: administration of flumazenil to patients with undifferentiated coma confers risk and is not recommended (Class III, LOE B) : seizures, hypotension and arrhythmia with TCAs Indication: reversal of excessive sedation during procedural sedation Lheureux P, Vranckx M, Leduc D, Askenasi R. Flumazenil in mixed benzodiazepine/tricyclic antidepressant overdose: a placebo-controlled study in the dog. Am J Emerg Med. 1992;10:184 –188. Pitetti RD, Singh S, Pierce MC. Safe and efficacious use of procedural sedation and analgesia by nonanesthesiologists in a pediatric emergency department. Arch Pediatr Adolesc Med. 2003;157:1090 –109 β-Blockers: myocardial membrane-stabilizing activity >>> QRS widening and decreased myocardial contractility Cardiovascular complications of B-blocker toxicity: include hypotension, bradycardia, AV blocks of different degrees, and CHF with or without pulmonary edema. Most common: propranolol seizure is highest with propranolol, particularly when the QRS complex is > 100 ms Beta Blockers Glucagon Drug of choice for -blocker (& CCB) O.D. • Secreted by pancreas secondary to hypoglycemia • Glucagon Receptors found in heart muscle • Acts by stimulating adenylate cyclase. independent of -receptor glucagon -blocker + Glucagon receptor Beta Blockers: Glucagon The final outcome: positive chronotropic and inotropic effects despite -adrenergic blockade. Onset within minutes, peak levels in 5-7 minutes, duration of action of 10-15 minutes. Beta Blockers Glucagon - precautions 1. Diluent contains 2 mg/ml phenol as preservative i. ii. Max 10-h dose of phenol = 50 mg = 5mg glucagon Use sterile water instead of diluent 2. Side effects from glucagon include: i. dose-dependent nausea and vomiting aspiration ii. hyperglycemia, hypokalemia (not clinically important) iii. Some Reports of treatment failure Beta Blockers: Insulin Insulin?? Shown to have positive inotropic effects on animal and human myocardium Kerns, et al. Ann Em Medicine. 1997. 29:748-757 24 dogs, anesthetized and infused with propanol. Hemodynamics before & after treatment with: i. ii. iii. iv. Normal Saline (n=6) Insulin (4IU/min) + glucose PRN (n=6) Glucagon (50 ug/kg) + infusion (n=6) Epinephrine (1ug/kg/min) + titrated (n=6) Beta Blockers Results: 6/6 Controls died within 150 min 5/6 Epinephrine animals died after 240 min 2/6 Glucagon animals died “ “ “ 0/6 Insulin animals died “ “ “ Kaplan-Meier Survival Curve Insulin vs. Glucagon (p<0.05) Insulin vs. Epinephrine (p<0.02) Beta Blockers Insulin in Acute Beta Blocker OD. Pathophysiology ?: 1. May enhance catecholamine release 2. May enhance myocardial substrate use In normal myocardium, FFA are preferred substrate. In poisoned myocardium, glucose becomes 1o substrate 3. May increase cytosolic calcium Supportive therapy : activated charcoal for decontamination; combinations of fluid resuscitation, vasopressor agents, atropine, transvenous pacing Specific antidotes: glucagon bolus of 3 to 10 mgadministered slowly over 3 to 5 minutes, followed by an infusionof 3 to 5 mg/h (0.05 to 0.15 mg/kg followed by an infusion of 0.05 to 0.10 mg/kg per hour) (Class IIb, LOE C) high-dose IV insulin, accompanied by IV dextrose supplementation (Class IIb,LOE C) Other: Calcium, 0.3 mEq/kg of calcium (0.6 mL/kg of 10% calcium gluconate solution or 0.2 mL/kg of 10% calcium chloride solution) IV over 5 to 10 minutes,followed by an infusion of 0.3 mEq/kg per hour. hypotension and bradycardia extended-release (ER) formulations can result in delayed onset of arrhythmias, shock, sudden cardiac collapse, and bowel ischemia. Treatment: IV insulin/Dextrose Calcium (Calcium chloride (1-4 g IV; preferably via central line; (30 mL) of 10% calcium gluconate can be administered IV over 10-15 minutes in adults. Boluses may be repeated every 15-20 minutes for a total of 3 doses) Haddad LM. Resuscitation after nifedipine overdose exclusively with intravenous calcium chloride. Am J Emerg Med. Oct 1996;14(6):602-3 Hung YM, Olson KR. Acute amlodipine overdose treated by high dose intravenous calcium in a patient with severe renal insufficiency. ClinToxicol (Phila). 2007;45(3):301-3 Arrhythmia, hypertension, acute coronary syndrome HX: Onset and duration of symptoms depend on route of administration, dose, and patient tolerance Clinical Presentation Central Nervous System: agitation, psychosis, AMS etc Cardiovascular: ACS (6% ), hypertension, hyperthermia Acute Pulmonary Syndrome: y dyspnea, diffuse infiltrates, and hemoptysis Can act as a Vaughan-Williams class Ic antiarrhythmic, producing wide-complex tachycardia through several mechanisms, including blockade of cardiac sodium channels >>> Wide complex tachycardia Methamphetamine – MDAC Ascorbic acid no longer recommended Cocaine related ACS Diagnosis of cocaine related MI is difficult as 84% of patients with cocaine related chest pain have abnormal ECGs Half of all cocaine users have increased creatinine kinase concentrations in the absence of myocardial infarction Troponin concentrations are more sensitive and specific Pathophysiology: sympathomimetic action of cocaine produces an increase in myocardial oxygen demand and direct cocaine induced coronary artery vasospasm Benzodiazepines (lorazepam, diazepam), calcium channel blockers (verapamil), morphine, and sublingual nitroglycerin (Class IIb, LOE B) Aspirin for Cocaine ACS ; Lidocaine? Supportive: rapid cooling measures Caveats: phentolamine can be used but not propranolol, labetalol ineffective ( Class IIb, LOE C) (+) Wide complex tachycardia Sodium bicarbonate 1 mL/ kg (cocaine) IV as a bolus, repeated as needed until hemodynamic stability is restored and QRS duration is < 120 ms cyanide can be found in jewelry cleaners, electroplating solutions; fire smoke Joint DOH-DENR Advisory: Series of 2010001 on reporting of cases to DOH-FDA Clinical Manifestations: causes rapid cardiovascular collapse, which manifests as hypotension, lactic acidosis, central apnea, and seizures Enhancement of body’s natural mechanisms for dealing with cyanide: i. oxygen ii. Sodium thiosulphate Cyanide will also bind to methaemoglobin formed after administration of: i. Amyl nitrite; ii. Sodium nitrite, or; iii. 4-dimethylaminophenol (4-DMAP) Cobalt containing drugs: i. ii. Hydroxocobalamin, or Dicobalt edetate. Approach using evidenced based toxicologic interventions and supportive care guided by expert referrals on intervention and disposition from poison control centers Consider the toxidromes In critical care situations utilize standard AHA/ECC guidelines for BLS and ACLS Consider exceptions among severely poisoned individuals with exposure to specific toxic agents UP PGH NPMCC: 02-5218451 loc 2311 Department of Health: East Avenue Medical Center: (02) 4342511 Rizal Medical Center: (02) 5241078 Batangas Regional Medical Center: (043) 7233578 “Give a man a fish, and he can eat for a day. But teach a man how to fish, and he’ll be dead of mercury poisoning inside of three years.” —Charlie Haas (1889-1964)