optimization in external beam therapy: Part 1
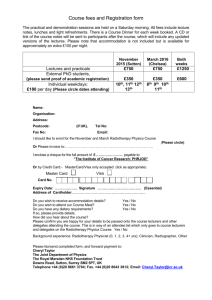
advertisement

IAEA Training Material on Radiation Protection in Radiotherapy Radiation Protection in Radiotherapy Part 10 Medical Exposure: Good Practice including Radiation Protection in External Beam Radiotherapy IAEA BSS: Medical Exposure • Exposure incurred by patients as part of their own medical or dental diagnosis and treatment • by persons, other than occupationally exposed, knowingly while voluntarily helping in support and comfort of patients • by volunteers in a program of biomedical research involving their exposure Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 2 Medical Exposure: Patients • In external beam radiotherapy (EBT) the quality of the treatment depends essentially on two parameters: • the accurate dose given, and • the exact localization of that dose in a welldefined target (by avoiding normal surrounding tissues as much as possible) Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 3 External beam radiotherapy • Support persons during irradiation: not applicable - no one must be in the treatment room during irradiation • Children are to be sedated or anesthetized during irradiation Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 4 External beam • Volunteers: not possible in the conventional way, however considered must be • participants in clinical trials • patients who undergo radiotherapy and are evaluated for other radiation effects • patients who undergo radiotherapy and have their treatment modified to answer research questions. Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 5 Objectives of the lecture(s): • Be aware of the implications of optimization on equipment design • Be able to discuss methods to ensure accurate dosimetry • Be able to understand the optimization process in radiotherapy planning and the delivery of the dose to the appropriate target • Be familiar with the radiotherapy treatment planning process Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 6 Contents • • • • Lecture 1: Equipment and Design Lecture 2: Dosimetry Lecture 3: Radiotherapy Treatment Planning Lecture 4: Treatment Verification and Reporting Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 7 IAEA Training Material on Radiation Protection in Radiotherapy Radiation Protection in Radiotherapy Part 10 Good Practice in EBT Lecture 1: Equipment design Equipment in radiotherapy • Radiotherapy relies - probably more than many other medical specialties - on equipment • Equipment design and performance is therefore of paramount importance for radiotherapy Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 9 Objectives • Be familiar with the ‘design considerations’ as stipulated by appendix II in the BSS • Be able to apply these design considerations in the context of radiotherapy equipment • Be aware of relevant international standards and other documents which provide specification for external beam radiotherapy equipment Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 10 Contents 1. Design considerations 2. Features of safe design in practice 3. Operational considerations Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 11 Design Considerations (BSS appendix II.11) • “Equipment used in medical exposure shall be so designed that: • failure of a single component of the system be promptly detectable so that any unplanned medical exposure of patients is minimized • the incidence of human error in the delivery of unplanned medical exposure be minimized” Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 12 Requires ‘Defense in Depth’ • • • • Redundant safety features Interactive equipment interface Self checks Intuitive software Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 13 Design Considerations BSS II.12 • “Registrants and licensees shall: (a) taking into account information provided by suppliers, identify possible equipment failures and human errors that could result in unplanned medical exposures (b) take all reasonable measures to prevent failures and errors, including the selection of suitably qualified personnel, the establishment of adequate procedures for the calibration, quality assurance and operation of diagnostic and therapeutic equipment, and the provision to personnel of appropriate training and periodic retraining in the procedures, including protection and safety aspects” Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 14 This would have prevented the following accident: Maintenance problem... • A misadjustment of the electron energy of an accelerator resulted in overdosage of 27 patients; the doses were between 3 and 10 times higher than intended, causing several deaths • Frequent failures of an accelerator, with frequent interruption of the treatments led to the decision to operate in “physical mode”; this decision resulted in one death Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 15 Accident after maintenance • Contributing factors to the accident (amongst others) • It was possible to operate the machine with the energy selector disabled • Conflicting displays and signals on the control panel were misinterpreted (the energy selector indicated different energy than an instrument on the control panel) Both factors should have been eliminated by good design Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 16 Design Considerations BSS II.12 (continued) • “Registrants and licensees shall: (c) take all reasonable measures to minimize the consequences of failures and errors that may occur (d) develop appropriate contingency plans for responding to events that may occur, display plans prominently, and periodically conduct practice drills” Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 17 Mitigation and emergency plans • Discussed in part 13 of the course Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 18 Design Considerations BSS II.13 • “Registrants and licensees, in specific cooperation with suppliers (a) the equipment conform to applicable standards of the International Electrotechnical Commission (IEC) and the ISO or to equivalent national standards (b) performance specifications and operating and maintenance instructions, including protection and safety instructions, be provided in a major world language understandable to the users and in compliance with the relevant IEC or ISO standards with regard to 'accompanying documents', and that this information be translated into local languages when appropriate” Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 19 IEC standards • In reference list • Often adopted into national standards these may contain additional requirements • http://www.iec.ch/ Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 20 Design Considerations BSS II.13 (cont.) • “Registrants and licensees, in specific cooperation with suppliers (c) where practicable, the operating terminology (or its abbreviations) and operating values be displayed on operating consoles in a major world language acceptable to the user (d) radiation beam control mechanisms be provided, including devices that indicate clearly and in a fail-safe manner whether the beam is ‘on’ or ‘off’” Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 21 In radiotherapy practice • Clear Indicators shall be provided at the control console and in the treatment room to show when the equipment is in operation • A secondary independent indicator (e.g. a radiation monitor inside the treatment room) may also be useful Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 22 General Safety Requirements • Warning Signals and Signs RADIATION DO NOT ENTER When RED LIGHT is on. Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 23 Design Considerations BSS II.13 (cont.) • “Registrants and licensees, in specific cooperation with suppliers (e) as nearly as practicable, the exposure be limited to the area being examined or treated by using collimating devices aligned with the radiation beam (f) the radiation field within the examination or treatment area without any radiation beam modifiers (such as wedges) be as uniform as practicable and the non-uniformity be stated by the supplier (g) exposure rates outside the examination or treatment area due to radiation leakage or scattering be kept as low as reasonably achievable” Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 24 In radiotherapy practice • From a practical point these are the most important stipulations regarding medical exposure within the BSS • They direct the user towards conformal (limit the area) intensity modulated (homogenous dose distribution) radiotherapy using best possible equipment (leakage is minimized) Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 25 Conformity • Shielding of areas which shall not be irradiated • Use of blocks - best customized for each individual patient Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 26 Customization of blocks • Use block outline on simulator film to cut the block shape into a Styrofoam block Huestis Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 27 Customization of blocks • Pour low melting alloy into foam • Customized blocks include divergence of the beam • Blocks are mounted on trays Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 28 Conformal radiotherapy • Conform the treated volume (receiving a therapeutic dose) to the planning target volume • shield all areas surrounding it • MLC is an option for this Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 29 Quick Question What are the differences between blocks and MLC for shielding in practice? Blocks versus MLC • Blocks • More work • Lifting of heavy blocks required • No leakage • Divergence covered • Isolated blocks (e.g. larynx shield) possible Radiation Protection in Radiotherapy • MLC • Interleaf leakage needs • • • • to be considered Flexible Dynamic shielding possible Required for most IMRT High initial investment, no additional cost per patient Part 10, lecture 1: Equipment design 31 Intensity modulation • • • • Optimize the dose distribution Make dose in the target homogenous Minimize dose out of the target Different techniques • physical compensators • intensity modulation using multileaf collimators Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 32 Physical Compensator Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 33 Compensator manufacturing • Sheets of lead glued together (compare previous slide) • Automatic milling into foam - this can be filled with low melting alloy or steel shot Par Scientific Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 34 Compensator manufacturing • Several manufactures of automatic compensator cutters • QC for each compensator is required Huestis Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 35 Intensity Modulation MLC pattern 1 • Achieved using a Multi Leaf Collimator (MLC) • The field shape can be altered MLC pattern 2 MLC pattern 3 • either step-by-step or • dynamically while dose is delivered Radiation Protection in Radiotherapy Intensity map Part 10, lecture 1: Equipment design 36 BSS appendix II: Requirements for radiation generators and irradiation installations for radiotherapy • II.15. “Registrants and licensees, in specific cooperation with suppliers, shall ensure that: (a) radiation generators and irradiation installations include provisions for selection, reliable indication and confirmation (when appropriate and to the extent feasible) of operational parameters such as type of radiation, indication of energy, beam modifiers (such as filters), treatment distance, field size, beam orientation and either treatment time or preset dose; …” Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 37 Two important thoughts • Radiotherapy depends on manufacturers and should be working with them to achieve common goals • Many parameters determine a particular radiation treatment - equipment should both allow unambiguous selection of these parameters AND indication of what has been selected Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 38 BSS appendix II Design criteria specific to radiotherapy • II.15. “Registrants and licensees, in specific co-operation with suppliers, shall ensure that: ... (b) irradiation installations using radioactive sources be fail-safe in the sense that the source will be automatically shielded in the event of an interruption of power and will remain shielded until the beam control mechanism is reactivated from the control panel; ...“ Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 39 Fail to safety concept • If something fails the unit automatically turns the beam OFF • This includes power failures: • X Ray units / linacs turn off • radioactive sources must be withdrawn automatically e.g. via a spring mechanism or gravity (fail safe…) Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 40 BSS appendix II Design criteria specific to radiotherapy • II.15. “Registrants and licensees, in specific co-operation with suppliers, shall ensure that: ... (c) high energy radiotherapy equipment: (i) have at least two independent 'fail to safety' systems for terminating the irradiation; and (ii)be provided with safety interlocks or other means designed to prevent the clinical use of the machine in conditions other than those selected at the control panel; …” Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 41 In radiotherapy practice • These 'fail to safety' systems for terminating the irradiation could be for example: • two independent integrating in-beam dosimeters (e.g. most linacs) • or two independent timers (e.g. 60-Co units) • or an integrating dosimeter and timer • Each system should be capable of terminating the exposure Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 42 A linac control example Additional timer Two independent dosimeters: MU1 and MU2 Varian Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 43 A kV X Ray unit Two independent timers: elapsed time and remaining time Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 44 BSS appendix II Design criteria specific to radiotherapy • II.15. “Registrants and licensees, in specific co-operation with suppliers, shall ensure that: ... (d) the design of safety interlocks be such that operation of the installation during maintenance procedures, if interlocks are bypassed, could be performed only under direct control of the maintenance personnel using appropriate devices, codes or keys; …” Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 45 Safety requirement • All modes of the equipment must be accessible only via a key and password • This affects in particular ‘physics’ or ‘maintenance’ modes, in which interlocks can be overwritten and system parameters changed • No treatment must be performed in service mode NEVER give your password to anyone... Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 46 BSS appendix II Design criteria specific to radiotherapy • II.15. “Registrants and licensees, in specific cooperation with suppliers, shall ensure that: ... (e) radioactive sources for either teletherapy or brachytherapy be so constructed that they conform to the definition of a sealed source; and (f) when appropriate, monitoring equipment be installed or be available to give warning of an unusual situation in the use of radiation generators and radionuclide therapy equipment.” Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 47 In radiotherapy practice... • This is a wide ranging requirement • Usually it is sufficient if conditions which affect correct operation do just make the treatment unit inoperable… • One may then check later WHY this is the case... Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 48 A note on ‘suppliers’ • All the BSS quotes so far have included the phrase: in specific co-operation with suppliers • This emphasizes the close collaboration which is required between manufacturers and operators of a radiotherapy facility • The collaboration is essential in regards to: • documentation • service/maintenance • training Radiation Protection in Radiotherapy Part 10, lecture 1: Equipment design 49