Diagnosing and Treating Mood Disorders
advertisement

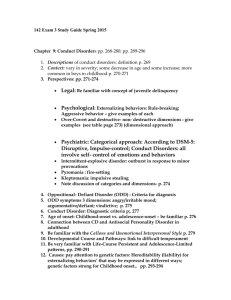
Diagnosing and Treating Mood Disorders: The Science and Ethics Chris Trimble, Leo Huizar, Fredah Kabbech, Megan Sieveke, Brandon Butler Mood Disorders Depression • Can refer to either: – A mood: a pervasive and sustained emotional response – A clinical syndrome: a combination of emotional, cognitive and behavioral symptoms How To Distinguish Depression From Normal Sadness • The mood change is pervasive across situations and persistent over time • The mood change may occur in the absence of any precipitating events • The depressed mood is accompanied by impaired ability to function in usual social and occupational roles • The change in mood is accompanied by a cluster of additional signs and symptoms • The nature or quality of the mood change may be different from that associated with normal sadness • • • • Four Types of Symptoms Associated With Mood Disorders Emotional Cognitive Somatic Behavioral Emotional Symptoms • Depressed or dysphoric mood is the most common and obvious symptom of depression • People who are depressed describe themselves as feeling utterly gloomy, dejected and despondent • Manic patients experience euphoric like symptoms Cognitive Symptoms • Involve changes in the way people think about themselves and their surroundings • Depressed people may have trouble concentrating and are easily distracted • Preoccupation with guilt and worthlessness • Manic patients report sped up thoughts and ideas Somatic Symptoms • Related to basic physiological or bodily functions • Include fatigue, aches and pains, and serious changes in appetite or sleeping patterns Behavioral Symptoms • Changes in the things that people do and the rate at which they do them • Psychomotor retardation often accompanies the onset of depression • Manic patients show energetic, provocative and flirtatious behavior Diagnosing Mood Disorders • Defined in terms of episodes – discrete periods of time in which the person’s behavior is dominated by either a depressed or manic mood Major Depressive Episode • Five or more of the following symptoms must have been present during the same two week period and represent a change from previous functioning • At least one of the symptoms is either – Depressed mood – Loss of interest or pleasure Major Depressive Episode Symptoms • Depressed mood most of the day, nearly every day • Diminished pleasure in all, or almost all activities • Significant weight loss (without dieting) or weight gain • Insomnia or hypersomnia nearly every day • Psychomotor agitation or retardation • Fatigue or loss of energy • Feelings of worthlessness or guilt • Diminished ability to think or concentrate • Recurrent thoughts of death or suicidal ideation Manic Episode • A distinct period of abnormally and persistently elevated, or expansive mood, lasting at least one week • During the period of mood disturbance, three of more of the following symptoms have persisted and have been present to a significant degree Manic Episode Symptoms • Inflated self esteem or grandiosity • Decreased need for sleep • More talkative than usual • Flight of ideas • Distractibility (drawn to unimportant stimuli) • Increase in goal directed activity • Excessive involvement in pleasurable activities that have a high potential for painful consequences Mood Disorders • Two primary types: – Unipolar mood disorder: the person experiences only episodes of depression – Bipolar mood disorder: the person experiences episodes of mania as well as depression Types of Mood Disorders and Frequency Types of Mood Disorders • Unipolar Mood Disorders – Major Depressive Disorder – Dysthymic Disorder • Bipolar Mood Disorders – Bipolar I Disorder – Bipolar II Disorder – Cyclothymic Disorder • Subtypes Major Depressive Disorder • One or more major depressive episodes • No manic or unequivocal hypomanic episodes • Lifetime prevalence of 15% • Major Depressive Disorder 15% suicide mortality • VA 1991 Study – Major Depressive Disorder mortality 38.7% – 13% no psychiatric monitoring Major Depressive Disorder • Course is variable – Some having episodes years apart, clusters of episodes, and some with frequent episodes throughout life – Only about 20% have chronic episodes • After the first episode, 50%- 60% chance of a second , and a 5%-10% chance of a manic episode (i.e. developing bipolar I disorder) • After second episode, 70% chance of a third • After third episode, 90% chance of a fourth • The greater number of previous episodes is an important risk factor for recurrence Major Depressive Disorder • By definition, Major Depressive Disorder cannot be due to: – Physical illness, alcohol, medication, or street drug use. – Normal bereavement. – Bipolar Disorder – 7Mood-incongruent psychosis (e.g., Schizoaffective Disorder, Schizophrenia, Delusional Disorder, or Psychotic Disorder Not Otherwise Specified). Major Depressive Disorder Co-occurring Disorders • Substance Abuse • Anxiety – 80 to 90% of individuals with Major Depressive Disorder also have anxiety symptoms (e.g., anxiety, obsessive preoccupations, panic attacks, phobias, and excessive health concerns). • Cancer, COPD (Chronic Obstructive Pulmonary Disease), Pain, eating disorders • Causation: – Meds: steroids – Diseases: hypothyroidism Dysthymic Disorder • Depressed mood for at least two years • Never without at least two of the following symptoms for more than two months – Poor appetite or overeating, insomnia or hypersomnia, low energy, low self esteem, poor concentration, feelings of hopelessness Dysthymic Disorder • No major depressive episode during the first two years • Lifetime risk of 3% Bipolar I Disorder • One or more manic episodes • Lifetime risk of 1% These positron emission tomography scans of the brain of a person with bipolar disorder show the individual shifting from depression, top row, to mania, middle row, and back to depression, bottom row, over the course of 10 days. Bipolar II Disorder • One or more major depressive episodes • At least one hypomanic episode – A hypomanic episode is a less severe version of a manic episode. • No manic episodes Subtypes of Mood Disorders • Melancholia: describes a particularly severe type of depression • Psychotic features: when hallucinations or delusions were present during the most recent episode • Rapid cycling: the person experiences at least 4 episodes within a 12 month period Subtypes of Mood Disorders • Postpartum Onset: when episodes begin within 4 weeks after childbirth • Seasonal affective disorder: when the onset of episodes is regularly associated with changes in seasons Prevalence of Mood Disorders • Depression accounts for more than 10 percent of all disabilities in the US • Younger generations are experiencing higher rates of depression, and those who become depressed are doing so at an earlier age • Depression affects 1314 million people each year Prevalence of Mood Disorders • Ratio of unipolar to bipolar is at least 5:1 • Lifetime prevalence of all mood disorders is 8%, ranked third behind substance abuse disorders and anxiety disorders Gender Differences • Women are two or three times more vulnerable to depression than men – Sex hormones, stressful life events, childhood adversity, etc – May be more likely to seek treatment – May be more likely to be labeled as depressed • No differences seen in bipolar disorders Children Statistics • Up to 2.5% of children in the US suffer from depression • Up to 8.3% of adolescents in the US suffer from depression • Girls entering puberty are twice as likely to experience depression as boys Types of Causes • Environmental Factors • Psychological Factors • Biological Factors Environmental Factors: Stress – Levels of stress may vary from person to person. – Depressive episodes can make a person more vulnerable to further episodes, so small amounts of stress can activate depression • “Learner Helplessness”- after experiencing chronic or repeated stressful events, people can learn to feel helpless Environmental Factors: Substance Abuse – Depression that is a result of drug abuse, medication, or toxin exposure – Associated with use and withdrawl from: alcohol, amphetamine, cocaine, hallucinogens, inhalants, opioids, phencyclidine, sedaitves, hypnotics and anxiolytics – Exposure or habitual use of chemicals can alter brain structure and function resulting in depression Environmental Factors: Childhood Difficulties – Depression can develop in children who have experienced a traumatic event including but not limited to: • • • • Death of family member or friend Natural disaster Divorce Loss of parent’s job, home, etc... – Many of these children are emotionally damaged or lack emotional development and often have difficulties adjusting – Traumatic Event may affect the development of the Limibic System Depression In Disease • Estimated 1/3 people with chronic disease have depression. • Alzheimer’s – Boston Study • 14% had history of depression • HIV – 1/3 estimated to have depression Continued… • The rate for depression occurring with medical illness*: – – – – – – – Heart attack: 40-65% Coronary artery disease (without heart attack): 18-20% Parkinson's disease: 40% Multiple sclerosis: 40% Stroke: 10-27% Cancer: 25% Diabetes: 25% *Reviewed by the doctors at The Cleveland Clinic Department of Psychiatry and Psychology. Psychological Factors • Cognitive Vulnerability – People responding differently to the same negative experience involving loss, failure and disappointment https://www.depressionadvances.com/animation/brainAnimations.html HYPOTHYROIDISM COMMON SYMPTOMS Delayed reflexes Depressed mood Weight changes Cardiac failure Apathy Appetite problems Cold intolerance Weight gain Sleep problems Brittle hair Fatigue Dry skin Impaired concentration Thoughts of suicide Delusions Decreased appetite DEPRESSION Biological Factors • Neurotransmitters and Neurons – The signal enters the neuron through the dendrite and proceeds through the cell body to the axon where it is switched from a electric signal to a chemical one – Theses chemical signals are called neurotransmitters • Neurotransmitters can fit into many receptors, but receptor sites can only receive specific transmitters • Upon release the transmitter is broken down by mono amine oxidase (MAO) or its taken back in by the neuron that released it, called “reuptake” Biological Factors • Of the 30 or so known neurotransmitters, depression effects Serotonin, Norepinephrine, and Dopamine • Depression has been linked to both low and elevated Norepinephrine concentrations. Biological Factors: Serotonin • The permissive hypothesis of serotonin function postulates that the deficit in central serotonergic neurotransmission permits the expression of bipolar disorder but is not sufficient to cause it. – According to this theory, both the manic and the depressive phases of bipolar illness are characterized by low central serotonin function but differ in high versus low norepinephrine activity. Biological Factors: Norepinephrine • The catecholamine hypothesis of affective disorders proposes that some forms of depression are associated with a deficiency of catecholamine activity (particularly norepinephrine) at functionally important andrengeric receptor sites in the brain, whereas mania is associated with a relative excess. Biological Factors: Dopamine • Evidence is substantial that enhanced dopamine activity may play a primary role in psychotic depression. Biological Factors: Hormones – About one half of all depressed persons have a high level of the hormone cortisol in their blood – A person with a depressive mood disorder may not have their hypothalamus regulating the cortisol production in the adrenal gland correctly – Normal cortisol levels peak at 8:00a.m. and 4:00p.m. for non depressed person, while a person with depression may have the hormone released at a constant level Biological Factors: Genetics • There is a 1.5 to 3% greater chance for a person to develop a depressive disorder if a parent or sibling has it as well – 50% of those with bipolar disorder have a parent with history of clinical depression – 25% of children of a parent who is bipolar develop a depressive disorder – 50-75% of children of two parents with bipolar disorder develop a depressive disorder Biological Factors: Twin Studies • If one twin develops depression there is a 76% chance that the other twin will develop a disorder as well – When raised apart the percentage is 67% – Because this number is not closer to 100%, there is indication that other factors are also responsible • Fraternal twins have a 19% chance of developing a depressive disorder if the other develops one Bipolar Causes Relation to Person w/Bipolar 2nd degree relative Risk of Developing Bipolar 1% Sibling 3-7% Fraternal Twin 15-25% One Parent 15-30% Both Parents 50-75% Identical Twin 70% Causes of Depression • Depression has been linked to size/function in the temporal and frontal lobes and the cingulate gyrus. However, it is unclear as to whether the depression causes the abnormalities or the depression is a result of the abnormalities. Treatment of Mood Disorders Treatments: • Unipolar Mood Disorders – Cognitive Behavioral Therapy – Antidepressant Medication • Bipolar Mood Disorders – Lithium – Anticonvulsant Medication – Psychotherapy • Others – Electroconvulsive Therapy – Vagus Nerve Stimulation – Transcranial Magnetic Stimulation Cognitive Behavioral Therapy • CBT combines both cognitive therapy and behavioral therapy – Cognitive Therapy teaches a person how certain thinking patterns are causing their symptoms-by giving them a distorted picture of what's going on in their life, and making them feel anxious, depressed or angry for no good reason, or provoking them into ill-chosen actions. Cognitive Behavioral Therapy – Behavioral Therapy helps patients weaken the connections between troublesome situations and their habitual reactions to them. It also teaches them how to calm their mind and body, so they can feel better, think more clearly, and make better decisions Cognitive Behavioral Therapy • Identification of Skill Deficits: – Help patient to identify deficits so that they can learn better ways to manage life • Evaluation of Life-Experiences – Help patient develop realistic expectations about life, and help distinguish between what the patient needs and what they want • Self-talk – Help patient identify negative self-talk, teach them how to combat these thoughts and to replace them with positive thought Cognitive Behavioral Therapy • Automatic thoughts – Help patient identify negative automatic thoughts and ways to replace these thoughts with positive ones • Irrational ideas and Beliefs – Teach patient how to identify their irrational thoughts and how to differentiate between irrational and rational thought • Overgeneralizing and Catastrophizing – Help patient identify and change negative overgeneralizations Cognitive Behavioral Therapy • Cognitive Distortions – Help patient determine what evaluations are distortions by providing objective feedback of their evaluations of the world • Pessimistic Thinking – Help patient develop more optimistic view of world Treatment: Antidepressants • Four types of drugs are used in the treatment of depression and other associated mood disorders: – Tricyclic antidepressants – Monoamine Oxidase Inhibitor – Selective Serotonin Reuptake Inhibitors – Serotonin Norepinephrine Reuptake Inhibitors Tricyclic Antidepressants • From 1960s until late 1980s, tricyclic antidepressants represented the major pharmaceutical treatment for depression • They still provide the surest antidepressant response for moderately to severe depression Tricyclic Antidepressants • TCAs work by increasing the concentration of norepinephrine and serotonin in certain regions of the CNS • TCAs impede the reuptake of norepindephrine and serotonin • They are safe and effective for up to 80% of patients Tricyclic Antidepressants • There are two broad chemical classes: – Tertiary Amines • They have a greater effect in boosting serotonin than norepinephrine. – amitriptyline, imipramine, trimipramine and doxepin – Secondary Amines • Greater increase of norepinephrine levels – nortriptyline, desipramine, and protriptyline Monoamine Oxidase Inhibitors • MAOIs treat depression by inhibiting the effect of monoamine oxidase which causes the concentrations of serotonin, norepinephrine and dopamine to increase • Most doctors will not prescribe MAOIs unless a patient is not responding to other antidepressants Monoamine Oxidase Inhibitors • Definitely Effective – – – – – – – – – Atypical Depression Major Depression Dysthymia Melancholia Panic Disorder Bulimia Atypical facial pain Anergic Depression Treatment-resistant depression – Parkinson’s Disease • Other Possible Uses – Obsessivecomplusive Disorder – Narcolepsy – Headache – Chronic pain syndrome – Generalized anxiety disorder Selective Serotonin Reuptake Inhibitors • SSRIs work by inhibiting the reuptake of serotonin into the neuron that made it • Includes fluoxetine and paroxetine Serotonin Norepinephrine Reuptake Inhibitors • This class of drugs is most recent addition to the family of antidepressants and has a structure and chemical profile that distinguishes them both tricyclic antidepressants and SSRIs. • Work by increasing levels of Serotonin and Norepinephrine by inhibiting their re-absorption back into the cell. Venlafaxine • Venlafaxine inhibits serotonin and norepinephrine reuptake without significant effects on muscarinic, cholinergic, histaminic, or alphaandrenergic receptors. • Therefore, venlafaxine activity is similar to tricyclics and SSRIs but has a less adverse side-effect profile. Bupropin • Bupropin is the newest drug for treating depression, although the exact neurochemical mechanism is not known – Does not inhibit monoamine oxidase or inihibit the reuptake serotonin and norepinephrine – Does inhibit the reuptake of dopamine to some extent • It is a stimulant type drug that is used in the treatment of major depression. Treatments: Antidepressants • 50-65% of people given an antidepressant show much improvement over 3 months, compared to 25-30% of people given a placebo. – Indicates that although drug is effective, antidepressants, like most medicines, may have some benefits due to placebo affect Treatments: Antidepressants • Medication must be used every day or at every time prescribed. If not taken correctly treatment will not be effective and may have adverse effects. • Antidepressants will usually take 1-2 weeks work, however some may take up to six weeks Treatments: Antidepressants • On the basis of clinical research and experience, the consensus is that most people can be taken off their antidepressants after six to eight months of clinical response without doing worse than patients continuing on the drug Bipolar Treatments • Psychiatric Management • Acute Treatment • Maintenance Treatment Psychiatric Management At this time, there is no cure for bipolar disorder; however, treatment can decrease the associated morbidity and mortality. Bipolar Treatments: Lithium • Lithium is prescribed to people with bipolar disorder to even out the “highs” and “lows.” • Because bipolar disorder requires long term treatment, a patient may have to take Lithium for many years, often in combination with other antidepressants Bipolar Treatments: Lithium • Lithium interferes with the synthesis and reuptake of chemical messengers by which nerves communicate with each other (neurotransmitters). Lithium also affects the concentrations of tryptophan and serotonin in the brain. • Lithium's effects usually begin within one week of starting treatment, and the full effect is seen by 2 to 3 weeks. Bipolar Treatment: Anticonvulsants • Often prescribed to patients who do not respond to lithium • Include carbamazepine (Tegretol) or valproic acid (Depakene) • More than 50% respond positively to these drugs • Reduce the frequency and severity of relapse Treatments: Electroconvulsive Therapy – Patient is put to sleep and temporarily paralyzed, so that their muscles do not contract and cause injuries like fractures. An electric current is then run through the brain to initiate a seizure. – ECT is sometimes the most effective, rapid method of treating severe major depressive disorder (MDD). • • • • for patients with poor response to medications, poor tolerance of usual antidepressants, severe vegetative symptoms, or psychotic features Treatment: Vagus Nerve Stimulation • • VNS stimulates the limbic system, a group of related structures that affect mood, motivation, sleep, appetite, alertness and other factors commonly altered by depression. VNS is delivered to the left cervical vagus nerve by the NeuroCybernetic Prosthesis (NCPâ) System which is implanted just under the skin in the left chest area. – Delivers a pre-programmed, intermittent electrical pulse to cervical vagus nerve 24 hours a day Transcranial Magnetic Stimulation • TMS is a procedure in which the electrical activity in the brain is influenced by a magnetic pulse. • This procedure can be used to alter function of certain areas of the brain, especially those involved in depression Side Effects of Treatments Side Effects: Tricyclics • Initially: • they cause blurred vision • Constipation • Light-headedness when standing or sitting up suddenly • Dry mouth • Difficulty urinating • Feelings of confusion • Cognitive Dysfunction – A small percentage of people will have other side effects such as: • sweating, a racing heartbeat, low blood pressure, allergic skin reactions or sensitivity to the sun. – Side effects usually disappear once therapeutic effects if medication take hold Side Effects: Tricyclics • More serious side effects, although rare, can be aggravation of narrow angle glaucoma and seizures • Some tricyclic side effects relate to the fact that these medications have similar effects on other neurotransmitters in the CNS, notably histamine and acetylcholine Drug Interactions: Tricyclics • Drug • MAOIs • Norepinephrine pressure arrhyhmias • Phenothiazines • Barbiturates metabolism • Cimetidine heterocyclics • Haloperidol • Methylphanidate heterocyclics Interaction Stroke, hypertension Large increase in blood and incidence of Psychosis, agitation Increase heteocyclic Blocks metabolism of Can block metabolism of heterocyclics Blocks metabolisms of Side Effects: MAIOs • The side effects of MAOIs are generally more severe or frequent than for other antidepressants Side Effects: MAIOs • • • • • • • • • • Drowsiness Constipation Nausea Diarrhea Stomach upset Fatigue Dry mouth Dizziness Low blood pressure Lightheadedness, especially when getting up from a lying or sitting position • • • • • • • • • • • • • Decreased urine output Decreased sexual function Sleep disturbances Muscle twitching Weight gain Blurred vision Headache Increased appetite Restlessness Shakiness Trembling Weakness Increased sweating Drug Interactions: MAOIs • Because of the extensive inhibition of monoamine oxidase by MAOIs enzymes raises the potential for a number of drug interactions. – Many of these interaction occur with overthe-counter medications Drug Interactions: MAOIs Drug Interaction Other MAOIS Increase risk for side effect; covulsions Hypertension; convulsions TCAs, Carbamazepine, Cyclobenzaprine SSRIs Stimulants (dextromamphetamine); Busirone Meperidine Dextromethorphan Direct Sympathomimetics Indirect Sympathomimetics Oral Hypoglycemics (insulin) Fenfluramine, L-Tryptophan Serotonin Syndrome Increased blood pressure Potentially fatal interaction Brief psychosis Increased blood pressure Hypertensive crisis possible May worsen hypoglycemia Serotonin Syndrome possible Food Interactions: MAOIs • Food Restrictions • MAOIs inhibit – Avoid: monoamine oxidase in • Cheese, overripe aged gut that is responsible fruit, fava beans, sausage, salami, sherry, for the break down of liquors, sauerkraut, tyramine. A build up of monosodium glutamate, pickled fish, brewer’s tyramine can lead to a yeast, beef and chicken sudden increase in liver, fermented products, red wine blood pressure and a – Used in moderation chance of heart attack • Coffee, chocolate, or stroke. colas, tea, soy sauce, beer, other wines Side Effects: SSRIs • • • • • • • • • • • • • • • loss of appetite, weight loss increased appetite, weight gain allergic reactions dry mouth irritability / anxiety sleeplessness drowsiness headache shaking dizziness fits / convulsions disturbance of sexual function (but this is also a feature of depression) sweating bruising manic or hypomanic behaviour • • • • • • • • • • • • • shaking dizziness fits / convulsions disturbance of sexual function (but this is also a feature of depression) sweating bruising manic or hypomanic behaviour abnormal movements low sodium level suicidal ideas abnormal movements low sodium level suicidal ideas Drug Interactions: SSRIs • Although the potential for interaction does exist, SSRIs are not associated with many of the interactions are seen with other antidepressants – Paroxetine and fluvoxamine have been associated with increased bleeding when given with wafarin – Does not effect Lithium levels Suicide and SSRIs • There is evidence that the use of antidepressants, especially SSRIs, can cause an increase in suicidal thoughts, however it does not show an increase in cases. – A severely depressed patient, or those with bipolar syndrome in a “low” phase, usually only have the energy to focus on their low. As the medication begins to take affect they will have an increase in energy and suicidal thoughts as they transition from their “low” or depressed episode. It is this time when the patient is still in a “depressed state of mind,” that they are able to think more about and idealize suicide because oh their higher energy level. Side Effects: SNRIs • • • • • • • • Nausea and vomiting Dizziness Insomnia Sleepiness Abnormal dreams Constipation Sweating Dry mouth • • • • • • • • Yawning Tremor Gas Anxiety Agitation Abnormal vision Headache Sexual dysfunction Side Effects: Bupropin • 28% of patients will lose five pounds or more • 0.04% of patients will experience seizures – Common: Agitation, constipation, diarrhea, dizziness, dry mouth, headache, increased perspiration, insomnia, nausea, vomiting – Rare: Acne, blurred vision, chest pains, chill, coordination problems, confusion, decrease in white blood cell count, fainting, fever,hair color change Withdrawls: SNRIs • Stopping treatment with SNRIs, especially when done suddenly, can cause withdrawal-like symptoms: – nausea, vomiting, anxiety, diarrhea, agitation, confusion, headaches, nightmares, coordination changes, or skin-tingling or shock-like sensations » Sometimes referred to as discontinuation syndrome Side Effects: Electroconvulsive Therapy • Anxiety or nervousness • Gastrointestinal distress (nausea and diarrhea) • Headache • Insomnia • Rash • Slight weight loss • Sexual impotence in men (about 10%) • Lose of interest in sex for both men and women; inability to achieve orgasm The Chris Pittman Case • In 2001, the 12 year boy shot and killed his grandparents while being under the influence of Zoloft, a popular antidepressant for the previous couple of days The Chris Pittman Case • Defense attorneys argued that Chris suffered adverse reactions to the drug including akathisia (a neurological reaction characterized by extreme internal restlessness, which has been associated with suicide and violence), emotional blunting, mania and psychosis with testimonies by Chris’s aunt and sister The Chris Pittman Case • Former FDA scientist Dr. Richard Kapit, who had approved Zoloft for human clinical trials even testified in Chris’s defense stating that some antidepressants can alter the behavior of people under 18, causing mania and even suicide • Chris was charged and sentenced as an adult on February 15, 2005, and is now serving 30 years in prison Ethics Ethics • Ethical issue arises over a depressed patients ability to make decisions concerning treatment. • An elderly patient that has been diagnosed with depression has recently become gravely ill, requiring dialysis. Ethics • If you are not given an effective dosage of antidepressant medication, suicide rates increase. Is the hit-or-miss method of treatment with medication ethical? • Untreated Depression has a high risk of suicide that accompanies the disorder Ethics • 54% of patients with bipolar disorder are misdiagnosed as having depression • Misdiagnoses and treatment of patients with bipolar disorder as having a unipolar disorder can magnify the patients symptoms • Many antidepressants can cause a patient with bipolar disorder to have exaggerated and prolonged “highs” and “lows” • Should we be quick to treat Depression with medication when misdiagnosis can have serious consequences. References • • • • • • • • • • • Downing-Orr, Kristina. Rethinking Depression - Why Current Treatments Fail. 1st ed. New York: Plenum Press, 1998. Higgins, Edmund S. "Is Depression a Neurochemical or Neurodegenerative?." Current Psychiatry 3.9 (2004): 39-40. Kline, Nathan S., M.D., Factors in Depression, Rockland State Hospital, Raven Press Books, Inc., 1974 Lazarus, Jeremy A. "Ethics in Split Treatment." Psychiatric Annals 31.10 (2001): 611-614. Oltmanns, Thomas F., Case studies in Abnormal Psychology, 3rd, John Wiley and Sons, Inc., 1991 Oltmanns, Thomas F., and Robert E. Emery. Abnormal Psychology. 5th ed. Upper Saddle River: Prentice Hall, 2004. Schatzberg, Alan F., and Charles B. Nemeroff. Textbook of Psychopharmacology. 2nd ed. Washington: American Psychiatric Press Inc., 1998. Spitzer, Robert L., Psychopathology, A case book, Columbia University, McGraw-Hill, Inc., 1993 Diagnostic and Statistical Manual of Mental Disorders. IV txt revision ed. Washington: American Psychiatric Association, 2000. "Depression Caused by Chronic Illness." Web MD. July 2005. WebMD Inc.. 02 Apr. 2006 <http://www.webmd.com/content/article/45/1663_51215.htm>. "Neurotransmitter Animation." Depression Advances. 2006. Eli Lilly and Company. 05 Apr. 2006 <https://www.depressionadvances.com/animation/brainAnimations.html>.