Total Rewards
advertisement

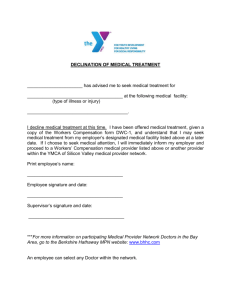
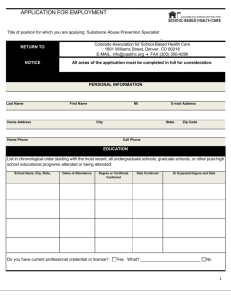
Employee Benefits TCHRA 2014 Larry Morgan, SPHR, GPHR, MAIR Total Rewards Compensation and Benefits 19% PHR 13% SPHR Compensation is “direct” Benefits are considered “indirect compensation” Agenda Review employee benefits History Benefit planning and assessment Legal, tax and regulatory issues Plan design issues Cost Employee communications Identify items most likely to appear on exam A Total Compensation System Total compensation Direct compensation Pay systems + Indirect compensation Benefit programs Indirect compensation • Designed to ▫ ▫ ▫ ▫ ▫ • Attract (limited value) Retain Improve productivity, work quality, and competitiveness Protect employee/family physical and financial well being Tax favorable treatment Must be affordable for employers and attractive to employee Objectives of a Total Compensation System Compatible with organizational mission, values and strategy Compatible with corporate culture Appropriate for the workforce Attract and retain talent Externally equitable Internally equitable Easy to communicate and understand Cost effective Legally compliant Conflicts Employees want everything at lowest costs Employers want to control expenses Government want revenues Burden on private employers / citizens vs. federal/state government programs Medicare/ Medicaid vs. private health insurance Social security vs. pension, 401k/403b and savings More on conflict Tax Code and Department of Labor define balance between conflicting priorities “Qualified plan” definition If not “qualified”, the employer must delay taking a deduction on the expense Plans cannot “favor” highly compensated employees (HCE), owners, officers, etc. Definition of HCE varies by benefit plan Total Compensation and the Organizational Life Cycle Introduction Growth Maturity Decline Wages and salaries Competitive but conservative Moderate At or above market Pressure to reduce Incentives Stock possibilities Bonuses tied to objectives, stock options Bonuses, incentive plans, stock options Reduced bonuses, costsaving incentives Benefits Basic Moderate, with limited executive perks Comprehensive, with expanded executive perks Looking to limit benefit costs, “frozen” executive perks A brief history of Benefits Societal issues drive changes Early 1900’s saw few employee benefits 1930’s 1940’s and 1950’s 1970’s 1990’s Competitive Marketplace Benefits as “hidden paycheck” Conducting a Benefit Needs Assessment Review organizational strategy Review current benefits Conduct gap analysis Review compensation philosophy Review employee needs The purpose of a gap analysis is to A. determine which employees are underinsured. B. revise benefits that are not meeting employee or organizational needs. C. eliminate benefits that are the most costly. D. ensure that all employees receive the same benefits. Types of Benefits 1. Mandated 2. Voluntary Mandated COBRA FMLA FUTA SUTA Workers comp Social Security FICA Medicare Voluntary (Optional) Benefits Health and Welfare ▫ Health care ▫ Dental ▫ Vision ▫ Section 125 Other Tuition Discounts Training Legal EAP Memberships Publications Cell phone Training • Retirement ▫ ▫ • Pension Defined Benefit Defined Contribution Retiree Medical Perquisites • • • • • • • Car Computer Home security Physical First class air Financial planning Legal Paid Time Off • • • • Sick leave Vacation Holidays PTO A closer look at specific Benefit Programs COBRA Regulations Update general and qualifying event notices. Provide an initial notice within 90 days of the date an employee/spouse is covered under the plan and mail the summary plan description to the residence. Establish reasonable notification procedures and communicate them to all employees. • Notify all employees who inform the company of a qualifying event within 14 days even if they do not qualify for COBRA. • Notify individuals whose coverage ends before the maximum continuous coverage period allowed. Consolidated Omnibus Budget Reconciliation Act (COBRA) Provides continuous group medical coverage after a qualifying event. Type of event determines the length of coverage (18 to 36 months). Voluntary, involuntary, reduction of hours, divorce, age attainment Employer can charge actual cost plus an administration fee. Initial notice. Qualifying event notice. COBRA timeframe • • Termination for gross misconduct – O months Other termination (voluntary or involuntary) – 18 months Layoff or reduction in hours – 18 months Disability – 29 months* Divorce or death of employed spouse – 36 months Dependent child loses eligibility – 36 months** State laws may vary Note changes under Patient Protection and Affordable Health Care Act to age 26 mandate (through calendar year of age 26 allowed) According to COBRA, a company with at least 20 employees must offer A. Health insurance to its employees. B. Continued medical coverage to employees terminated for gross misconduct. C. COBRA benefits to workers if the company terminates its health plan. D. COBRA benefits to spouses of deceased workers. Social Security Employer pays 7.65% Employee pays 7.65% Two components • Social Security 6.2% • Medicare 1.45% • 2013 maximum limit on SS portion is $113,700 • No limit on Medicare portion 1.45%** • Deduction still made on 401(k)!!! • No deduction on FSA pre-tax accounts • ** 2.35% on income over $200,000 Social Security Provides: Retirement income. Disability, death, and survivor’s benefits. To qualify: People must work 40 quarters, or ten years. Calculated as a set percentage of salary: Yearly maximum limit Deducted from employees’ pay People who work and receive payments must still pay in. Social Security Retirement Benefits Retirement income: Depends on individual’s average earnings. Indexes benefits to inflation. Pays reduced benefits at age 62. Indexes retirement age for full benefits to year of birth. Social Security Disability Benefits Are paid to workers (and eligible dependents) under full retirement age. Are paid when workers: Cannot work for at least five months. Have an impairment that is expected to continue for 12 months or result in death. Start after a five-month waiting period. Social Security Death and Survivor’s Benefits Death benefits $255 lump-sum payment to a surviving spouse Survivor’s benefits are paid to: Spouse at age 60 (50 if disabled). Spouse caring for a child under age 16/disabled child. Unmarried children under age 18. Children if disabled before age 22. Dependent parents, age 62 or older. Medicare • • • • Not dependent on income or ability to pay. Employee and employer pay a percentage of salary; there is no yearly maximum. All individuals are eligible at age 65. Employer benefits are primary for employees 65 and over who are working. • • • • • Part A (hospitalization) is mandatory. Part B (medical insurance) is optional. Managed care option. Part C (Medicare Advantage Plans) allows participation in different health care plans such as HMO and PPO Part D (prescription drugs) Medicare Part D Adds an outpatient prescription drug benefit. Benefits include: Annual deductible of $325. Coverage gap between $2,970 and $4,750. Catastrophic level of coverage reached after $6,734 in out of pocket. Unemployment Insurance • • • State run program Mandatory benefit funded primarily by employers. Eligibility in most states includes: ▫ ▫ ▫ ▫ ▫ ▫ • • Being available and actively seeking work. Not refusing suitable employment. Not having left job voluntarily. Not being unemployed because of labor dispute. Not being terminated for misconduct. Working a minimum number of weeks. Duration: 26 weeks Note: Federal program may extend this during periods of high unemployment with supplemental unemployment benefits (SUB) Workers’ Compensation State insurance paid by the employer. Protects workers in case of a work-related injury or disease. Experience-rated; employers who have a high number of claims pay more. Employers assume all costs, regardless of who is to blame. Workers’ Compensation Benefits include: Medical care. Disability income. Rehabilitation. Death benefits. Compensation is tied to fixed schedules. States regulate workers’ compensation. An employee drops a cup of coffee on the shop floor, slips, and breaks a leg. The cost of the injury will be covered A. by the employer B. by the employee C. jointly by the employer and employee D. by Medicare Qualified vs. Non-qualified benefits Qualified Meets IRS and ERISA standards Employer may take immediate tax deduction Non-qualified Typically used for executives Keeps executives “whole” Employer cannot take deduction until it is taxable to the employee Employee Retirement Income Security Act (ERISA) Establishes standards for taxfavored status of ALL benefits. Allows organization to deduct cost. Allows employee tax favored status Minimum eligibility standards Sets standards for retirement plans. Operate plans for exclusive benefit of participants and their beneficiaries. Sets up the Pension Benefit Guaranty Corporation (PBGC). Defines minimum vesting schedules for cliff and graded vesting. Sets procedures for claims administration and appeals of adverse determinations. Establishes prudent person rule. Characteristics of Qualified Plans Under ERISA, plans must: Be in writing and be communicated to employees. Be established for exclusive benefit of employees/beneficiaries. Satisfy rules concerning eligibility, vesting, and funding. Not favor officers, shareholders, or HCEs. Prudent Person Rule- SPHR only Fiduciary role Employer sponsor must follow prudent person rule Cannot take risks that a reasonably knowledgeable, prudent investor would take under similar circumstances Retirement plans Defined Benefit Plans • Benefit amount is based on a formula. • Employer funds the plan and bears the risk. • Insured by the PBGC. Flat-dollar formula Career-average formula Cash balance plan Final-pay formula Cash Balance Plan- hybrid Type of defined benefit plan Expresses promised benefit in terms of hypothetical account balance Employer assumes investment risks and rewards Is portable At retirement, employees receive either: Lifetime annuity Lump sum Defined Contribution Plans Profit-sharing plans • Employees and employers pay a specific amount per person into the fund. • Benefits are determined by fund performance. Money purchase plans ESOPs 401(k) / 403(b) plans Other Tax-Deferred Plans IRAs SEPs SIMPLE 403(b) plans 457 plans For individuals For self-employed individuals and very small businesses For employees (with contributions and matching) For certain tax-exempt 501(c)(3) organizations For employees of states, state agencies, and political subdivisions and certain tax-exempt organizations Catch up contributions DC limit employee contributions to $17,500 in 2013 However, persons turning age 50 or above to supplement IRA and 401k/403b contributions 2013 catch up limit is $5,500 Rollovers Unemployment Compensation Amendments (UCA) imposes a 20% federal income tax withholding requirement on plan rollovers unless there is a trustee-to-trustee transfer. Which of the following tax-deferred plans applies to employees of colleges, universities, and public charities? A. SEPs B. IRA C. 457 D. 403(b) Economic Growth and Tax Relief Reconciliation Act (EGTRRA) Adjusts minimum vesting schedules for employer matching contributions to defined contribution plans. Three-year cliff vesting Six-year graded vesting (20% after two years and 20% per year thereafter) Vesting for DB Pension Plans Five year cliff vest or 20% after three years and 100% after seven years Economic Growth and Tax Relief Reconciliation Act (EGTRRA) Sets permissible compensation limits— Code Section 401(a)(17). Sets limits on annual pensions—Code Section 415(b). Permits catch-up contributions for employees age 50 and older. Modifies distribution and rollover rules. Nonqualified Deferred Compensation Plans Provide additional benefits to key executives. Employees defer reporting income; not subject to the limits placed on qualified plans. Employer contributions are not deductible. Funds are not protected by ERISA or PBGC. Examples: Rabbi trusts, top hat, mirror plans and excess deferral plans Qualified Domestic Relations Orders (QDROs) Create or recognize the right of an alternative payee to receive all or a portion of an employee’s pension benefits. Orders must relate to child support, alimony, or marital property rights and must be made under state domestic relations law. Health Care Health-Care Plans • Indemnity (fee-for-service) plans ▫ ▫ ▫ • Full-choice plan Employees can go to any qualified physician. Fees are generated when services are used. Managed care plans ▫ ▫ ▫ Prepaid health-care plans Physician is paid per capita (per head) rather than for actual treatment provided. Members enroll and pay a set monthly or annual fee. Types of Managed Care Plans HMO- Health maintenance organizations Group, staff, and IPA models PPO- Preferred provider organizations POS- Point-of-service organizations EPO- Exclusive provider organizations PHO- Physician hospital organizations More than one health plan? Coordination of benefits apply First the claim goes to the employee Then, to other plans Birthday rule For dependents, primary coverage is whichever employee (parent) has birthday first in calendar year An employee is covered under more than one employer-sponsored insurance plan. A health claim requires A. utilization review. B. coordination of benefits. C. establishment of out-of-pocket maximums. D. premium sharing. Other Health-Care Options Dental plans Vision care plans Prescription drug plans Employee assistance programs Alternative health care Cancer plans Health-Care Funding Fully insured Minimum premium Partially self-funded Administrative-services-only Third-party administrator Self-insured Section 105 Health insurance purchasing cooperative Controlling Health-Care Costs Balance billing Consumer Directed Health Care Increase deductibles Increase co-pays Redesign policies Promote wellness Employee education Reasonable and customary Utilization review Nonprescription Drugs Nonprescription over the counter drugs or medicines can no longer be reimbursed through an FSA without a doctors note. Expenditures must be for medical care defined as the diagnosis, cure, mitigation, treatment, or prevention of disease. Health Reimbursement Accounts (HRA) • • • Employer-funded plan. Combines a high deductible health care plan with individual HRAs the employer funds. HDHP deductible levels for 2013 • • • • • Individual $1,250 Family $2,400 Plan reimburses employees for eligible and substantiated health-care expenses. Employees may NOT contribute on any pretax basis. Not portable Health Savings Account (HSA) Tax-sheltered savings • Earnings grow tax-free account similar to an IRA and distributions for that is created to pay for qualified medical medical expenses expenses are tax-free. Individual must be • Unused funds can be covered by a high carried over from year to deductible health plan year, are portable, and (HDHP) and must not be can be used into covered by any other retirement. non-HDHP. Contributions can be made by the employer, employee, or both. In order for the employee to gain a favorable tax treatment from benefits Must comply with ERISA Plan document Cannot favor highly compensated employees Summary plan description Must comply with Section 125 regulations Section 125 Plans Premium-only plans Employees receive favorable tax treatment on benefits already offered. NOTE CHANGES UNDER ACA Full cafeteria plans Benefit credits are used to purchase benefits. Unused credits can be cashed out. Flexible Spending Accounts Flexible spending accounts Pretax dollars are set aside to pay for dependent care $5000 or unreimbursed medical expenses $2500. Medical Spending account “Use-it-or-lose-it” options include Grace period of two and one-half months at the end of the plan year or $500 carryover No over the counter medications Limited use FSA for HRA plans Domestic Partners If same sex couples married in state or jurisdiction which recognizes the marriage, favorable federal tax treatment regardless of state of residence. State tax law may differ. Opposite sex couples not recognized, imputed income tax on value of benefits to employee. Key Provisions of the Patient Protection and Affordable Care Act Continues to evolve Requires employees to have coverage* Exchange programs created Large employer penalty delayed until 2015 (50 or more FTE working 30 or more hours/week) Reporting of employer and employee cost on W-2 Minimum essential coverage Affordable coverage (individual only) Must cover dependents to age 26 No requirement to cover spouse Summary of Benefit Coverage statements Additional taxation under PCORI and Transitional fees Paid and unpaid leave plans Paid Leave Paid leave for events: Break time Holiday pay Vacation pay Community service pay Leave of absence Bereavement leave Volunteer projects Paid-time-off banks Paid time off is lumped into one account. Proven to be effective at controlling absenteeism. Family and Medical Leave Act (FMLA) • • • • • • Provides 12 weeks of unpaid leave for employees to handle birth, adoption, or serious illness of a child, spouse, parent, or the employee. In loco parentis New ruling on domestic partners Serious illness requires inpatient hospital, hospice, or residential care, or continuing physician care. Military emergency exigency and caregiver leave Modified duty (light duty) vs. same position issues Family and Medical Leave Act (FMLA) Covers employers with 50 or more employees. Employee must have worked at least 12 months and 1250 hours within 12 month period Entitles employees to: Health benefit continuation. Reinstatement rights. Must treat the employee as an “active employee” while on leave. Employers may determine if leave is paid or unpaid Employers may define 12 month basis Employers must notify employee in writing of FMLA leave status Immediate supervisor CANNOT contact medical provider According to the FMLA, which of the following is true? A. B. C. D. Employers must pay all health benefit costs for employees on leave. Employees must return to a job with equivalent status, pay, and benefits. A week containing a holiday does not count as a full week of FMLA leave. Employees are eligible for FMLA leave after six months. Income Replacement Protection • Sick leave • Short term disability • Long term disability • SSDI Illness Paid time off programs Sick leave No fault plan- covers any absence Not covered under ERISA Common to require doctor statement after three days Only used for employee or family member illness Disability- usually a waiting period Workers comp Disability Coverage If employer provides, any income is taxable If employee pays, any income is not taxable Worker comp pays for job related illness or injury Short term generally covers continuous illness / injury up to six months LTD may have same occupation clause of 2-3 years Some plans have inflation or cost of living escalation and waiver of premium clauses Other benefits Life Insurance Protection May be paid by employer or employee Group-term life insurance First $50,000 in group life is not taxable income Excess group-term life insurance Dependent group life insurance Split-dollar plans for executives Accidental death and dismemberment Supplemental life Long term care insurance Provides for supplemental coverage in nursing home or at home care In addition to Medicare levels Premiums may be taken on pre-tax basis Which of the following statements about voluntary benefits is true? A. Employers can deduct their part of a long-term care premium from annual income taxes. B. Group-term life insurance policies of less than $75,000 are not taxed. C. Employees do not have to pay taxes on supplemental unemployment benefits. D. Insurance provided only to executives is not taxable Section 529 plans Provides college or education savings May be employer sponsored Post tax, but interest is not taxable May be transferred to other family members Excise tax if not used for education Wellness Employers may provide incentive up to 20% of health care premium for PARTICIPATION in wellness programs Cannot be outcome based Must have alternatives for persons not able to participate GINA concerns HIPAA concerns Other Benefits Flexible Spending Accounts • Non-reimbursed medical care • • • Dependent care: ▫ ▫ ▫ $245 month limit Tuition reimbursement (Section 127) Child-care services Elder care $5000 maximum Transportation assistance (Section 132) Over the counter medications no longer covered Employer is “at risk” if employee leaves $5250 annual limit Legal insurance Severance Which of the following items is generally subject to federal taxation? A. $1,000 reimbursement for a business trip B. $300 per month for parking C. $20 gift from a vendor D. $1,500 for a job-related training seminar An employer pays an FSA medical claim for $500 in March. In April, the employee leaves the company after setting aside only $250. What happens in this situation? A. B. C. D. The employee must return $250 to the company. The employer may withhold $250 from the employee’s last paycheck. The employee is entitled to the reimbursement as paid. The employee becomes ineligible for COBRA coverage. Executive Perquisites Travel upgrades Airline lounge Company car Golden parachute Golden handcuffs Employment agreements Physical exam Tax preparation Financial planning Legal services SERP Additional medical Emergency evacuation Country club or health club Business expense account Internet use Security system Driver Cell phone / Smartphone Cost of Benefits Benefits are very expensive US Chamber of Commerce survey in 2009 suggests employee benefits are 44% of payroll Employee satisfaction rises as level of understanding increases Employer may or may not contribute based on type of benefit (eg. Defined benefit pension or HRA vs. health care) Major Legislative and Regulatory actions Regulatory Agencies and Programs IRC FASB IRS State Mandates Treasury Dept DOL SEC State Insurance Key laws affecting Benefits ADEA COBRA EGTERRA ERISA FMLA GINA HIPAA IRC Mental Health Parity Act OWBPA Patient Protection and Affordable Care Act PBGC Pension Protection Act REA Sarbanes Oxley Unemployment Compensation Genetic Information NonDiscrimination Act (GINA) Protects individuals from having genetic information used: In employment. To impact health plan eligibility, enrollment, or premiums. Limits exceptions for genetic testing to: Wellness programming. Physician’s request. Checking biological effects of toxic substances in the workplace. Covered under HIPAA Health Insurance Portability and Accountability Act (HIPAA) Limits exclusions for preexisting conditions. Guarantees workers leaving a job with employer-sponsored health coverage the right to purchase coverage on their own. Guarantees renewability as long as premiums are paid. Makes health coverage portable. Health Insurance Portability and Accountability Act (HIPAA) Classifies long-term care expenses as medical expenses. Increases the tax deduction for medical expenses of self-employed individuals. Provides tax exemptions on premature IRA withdrawals used for medical expenses. Includes fraud and abuse provisions. Requires employer to safeguard information and protect against data release and identify theft HIPAA Privacy Rule: Administrative Duties • • • • Establish a system of consistently enforced sanctions. Keep records for six years. Establish written contracts with third parties who have access to protected information. Review data protection and access • Filing systems restricted • Employee benefit information kept out of personnel files • System security • Data encryption HIPAA Privacy Rule: Administrative Duties • • • • • • • • Health Information Technology for Economic and Clinical Health (HITECH ) Establish systems for tracking protected health information. Safeguards for protecting private information PHI and ePHI definition• Includes diagnosis, medical treatment and payment • Safeguards DOB, SS, sharing of health related information • Other reasons require release of information Designate a privacy officer. Establish a complaint mechanism. Ensure that individuals cannot waive their rights. Provide training to the workforce. Mental Health Parity Act (MHPA) Employers are not mandated to have mental health coverage Requires same dollar limits for mental health, substance abuse and medical benefits Copays and deductibles must be the same Annual and lifetime limits must be the same . Note preventative care requirement for depression and eating disorders as part of Health Care Reform Act Older Worker’s Benefit Protection Act (OWBPA) • • • Prohibits discrimination in employee benefits and includes specific requirements for waivers of claims. Prohibits older workers from waiving their ADEA rights unless they are given 21 days to consider the agreement and consult an attorney; in group terminations, workers must receive 45 days. Comply with ADEA Omnibus Budget Reconciliation Act (OBRA) Reduced compensation limits in qualified retirement programs. Triggered increased activity in nonqualified retirement programs. Pension Protection Act • PPA made provisions of EGTRRA permanent ▫ ▫ ▫ ▫ Catch up contributions SIMPLE IRA and 401(k) Roth 401K and 403b Accelerating vesting schedules for DB and DC plans • 20% minimum at two years, 20% each year thereafter and 100% at end of six years (by year seven) OR Cliff vest at three years Automatic enrollment into a 401k plan with default contribution levels Retirement Equity Act (REA) Provides legal protections for spousal beneficiaries of retirement plan participants. Requires written spousal consent for: Changes in retirement plan distribution elections. Changes in spousal beneficiary designations. In-service withdrawals. Sarbanes-Oxley Act (SOX) Requires administrators to notify plan participants of blackout periods for 401(k) or defined contribution plans. Protects employees who report violations of federal security laws or fraud against shareholders. Administered by DOL’s Employee Benefits Security Administration. Securities and Exchange Act Affects company stock option and purchase plans. Requires: Registration of all securities sold. Disclosure and restriction of “insider” trading. Black out periods Special filings Regulates discounts on stock purchase by employees Blackout Notice Requirements Must be done in writing 30 days in advance and must contain: Reasons for blackout. Identification of affected rights and investments. Expected beginning date and length of blackout. Statement that individuals should evaluate the appropriateness of their current investment decisions. Uniformed Services Employment and Reemployment Rights Act (USERRA) Addresses employer’s obligation to employees on active military duty. Prohibits discrimination in employment, job retention, and advancement (now included within EEOC including “hostile work environment”). Allows military leave for up to five years with vesting toward retirement and paid time off. Requires employees to give notice of their need for leave. Emergency exigency Uniformed Services Employment and Reemployment Rights Act (USERRA) Requires service members to notify employers of their intention to return to work. Requires employers to make health coverage available to employees and covered dependents at the employees’ expense (including a 2% administrative fee). Health care duration is for 24 months or length of military service, whichever is less. According to USERRA, employees called up for active duty are entitled to A. higher limits for salary deferral contributions. B. credited service for retirement plan purposes. C. lower copayments and deductibles for continued family medical benefits. D. an early vesting schedule for retirement benefits. Some states have additional rights (Not on exam) • Minnesota Parental Leave Act ▫ ▫ ▫ • Minnesota COBRA ▫ ▫ ▫ • • • Similar to FMLA 20 or more employees Six weeks Two or more employees Shorter time frames If divorced or disabled, longer extensions Minnesota School Conference Leave Employee sick leave allowed for relatives Minnesota Bone Marrow Leave Federal vs. State Laws Generally, federal law supersedes state laws Not necessarily true with Employee Rights Most favorable given to employee Examples: Minimum wage COBRA and state health insurance continuation Tax and Accounting Treatment FASB decides how financial firms should report financial information to shareholders. Requires companies to treat employee stock options as an expense on financial statements beginning in 2005. IRS implements and interprets tax legislation: Revenue rulings Private-letter rulings International issues – SPHR only • • • • • • • • • • • • • Standardization vs. localization Culture Home vs. host country expenses Competitive labor market Nationalized programs Laws and regulations Collective bargaining Paid time off Maternity / paternity Special allowances Taxation Expatriation and repatriation issues Totalization agreements Evaluating the Total Compensation System Is it in compliance? Is it compatible with the mission and strategy? Does it fit the corporate culture? Is it internally equitable? Is it externally competitive? Do employees understand the programs? Do employees understand the value? Required Communication ERISA requires: Summaries of the plan description, annual report, and material modifications. Filing Form 5500 with the DOL. Other required communications include: COBRA Notice CHIPs ACA notifications re: grandfather status, dependents covered to age 26, well woman care, etc. HIPAA privacy notice Continuation of benefits’ notice. Explanation of stock options (SEC regulation). Posting of all required federal and state employment laws such as FMLA, GINA, etc. Other Employee Communication Communication plans Written compensation philosophy, policies, practices, procedures, and announcements, as well as open enrollment periods, benefit fairs, etc. Direct communication Confidential communication with HR or a manager Trends Health Care Reform Act providing greater coverage and controls Continued movement toward cost containment Consumer Driven Health Care Employee education and awareness Total reward statements Baby boomers will be influential Trend away from defined benefit plans and retiree medical Key Terms to know ADEA Cliff vesting COBRA Consumer directed health care Coordination of benefits Copayment Deferred compensation Defined benefit plan Defined contribution plan ERISA ESOP Excess deferral FMLA FASB 529 plan Flexible spending account 401(k) plan 403(b) plan 457 plan Full cafeteria plan Fully insured plan Terms, continued GINA Golden handcuffs Golden parachute Graded vesting Group term life insurance HIPAA Health insurance purchasing cooperative HMO HRA HSA Highly compensated employee In loco parentis Indemnity health care plans Indirect compensation IRA International social security agreements (Totalization agreements) Involuntary deductions Lifetime maximum benefit Long term care insurance Long term disability Terms, continued Managed care Medicare Medicare carve out Mental Health Parity Act Modified duty program Money purchase plan Non-duplication of benefits Non-qualified deferred compensation Older Worker Benefit Protection Act Out of pocket maximum Paid time off bank Parachutes PBGC Pension Protection Act Perquisites Point of service organization Preexisting condition PPO Premium only plan Profit sharing plan Terms, continued Qualified plan Qualified domestic relations orders Qualifying event Rabbi trust Reasonable and customary Roth 401(k)/403(b) plans Roth IRA SOX SIMPLE Section 125 plans SEC Serious health condition Severance Short term disability Sick leave SEP Social Security Stop loss coverage Supplemental unemployment benefits Top hat plan Total rewards Totalization agreements Terms, continued Unemployment compensation USERRA Utilization review Vesting Voluntary deductions Whistleblower Work opportunity tax credit Work related disability Workers compensation Contact information Larry Morgan 952-210-0742 Larry.morgan@orionhr.com