Facial Lacerations - UCLA Head and Neck Surgery
advertisement
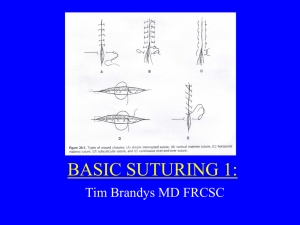
Facial Lacerations Nima Shemirani Eos Rejuvenation Lasky Clinic, Beverly Hills CA Objectives Basic principles of wound healing Suture and needle choices Techniques of effective closure to optimize scar outcomes Wound preparation Comparison of suture types Role of antimicrobials Evaluation of patient After ABCs, anesthetize laceration and explore locally Thoroughly clean all debris and blood from face to avoid missing a laceration Surgilube is a great way to clean dried blood – leave on for 2 minutes and wipe with 4x4 Assess depth of wound, layers affected, and look for fractures which may be at the base of the laceration Principles of wound management Thoroughly cleanse the wound with copious irrigation If there is any debris – it must be removed, residual debris will leave tatoos within the dermis (may need to use scrub brush) Reference Wound physiology and healing Only the dermis is capable of regeneration, not the epidermis Wounds will contract as they heal A tension-free closure is essential to help avoid widened scars Remove foreign bodies, devitalized tissue Features involving face Can be up to 9 degrees warmer than extremities High relative blood flow aids in preventing infection without the use of antibiotics Sutures to be left in 5-7 days to avoid tracking Anatomy of a needle 3 parts: point, body and swage Needle is rounded at swage end Needle is flat within body (best place to grab with needle driver Anatomy of a needle (cont) A = swage (needle rotates) B= body (needle secure) C= point (point is blunted) Needle choices Taper – stretches tissue, good for deep, soft and elastic tissue Conventional cutting – 3rd edge along inner aspect of needle – can pull needle through tissue inadvertantly Reverse cutting – 3rd edge along outer aspect of needle to minimize pulling the needle through Needle driver choice Jaws of needle driver should approximate 3035% of the length of the needle A= just right B= too big C= too small Suture choices Ideal suture: absorbable, minimal reactivity, minimal “memory,” and ease of use Absorbable - Fast gut, chromic gut, cat gut, Vicryl, Monocryl, PDS Non-absorbable – Nylon, Prolene Sutures and strengths Suture Type Chromic Gut Natural Tensile Strength (50%) 5 days Absorption Rate Fast Gut Natural 2-3 days Complete by day 5-10 Coated Vicryl Braided 3 weeks Complete by day 50-70 Monocryl Monofilament 1 week Complete by day 90-120 PDS II Monofilament 4 weeks Complete by 180 days Complete by day 90 Costs of suture (hospital wholesale) Black nylon (5-0) = $3.22 Blue Prolene (5-0) = $4.28 Fast gut (6-0) = $4.78 Dermabond capsule = $25 Deep suture technique Suture is tied on deep side of knot Important to enter and exit tissue at same levels Formation of “box” type knot (width=length) Matching uneven skin edges Use layer of skin to match levels (dermis to dermis) This will help ensure a even edge closure Importance of eversion Wound will contract over time Need to evert wound edges to prevent depressions and widening of scar For proper eversion Penetrate skin and tissue at 90 degree angles Form a “box” with the suture Injection Topical anesthetic may help For kids, give a dose of benadryl with topical Use 1% lido with epi (hemostasis) and bicarb in a 1cc bicarb to 9cc of lidocaine + epi For abscesses use 2% lido+epi (8cc) and bicarb (2cc) Use 30g needle and inject SLOWLY Try to enter the laceration in areas that are already anesthetized Forehead Simple interrupted sutures should only be left in place for 3-4 days to prevent track marks Usually this is not enough time for adequate healing and wound strength Alternatively, use a sub-cuticular running suture with prolene or nylon and use steri-strips so you can leave sutures in longer Very important to get good deep closure Example of Sub-Cuticular Eyelid Look for fat in the wound This is a sign that the orbital septum (continuous with the periosteum) has been violated - call occuloplastics Suture skin only with small bites, do not need to reapproximate orbicularis oculi - this may lead to scar contracture and inability to close eye Example of a bad outcome Example of a bad outcome Lip Extremely important to realign the vermillion A 1mm step-off in the closure will be noticeable Reaproximate the orbicularis oris musle to relieve tension in this active area Lip Closure Scars change over time Regional Blocks Work well in areas such as the lip whose anatomy can be altered with local injections To approximate the lip, align the red border Lido with epi may blanch the skin so re-aligning the lip can be difficult Infra-orbital block for upper lip, mental nerve 3-4-5 rule, use the 3rd tooth from the midline for upper, in between 4 and 5 for lower “How to block and tackle the face” - Zide Ear Skin is adherent to underlying cartilage Difficult to suture cartilage together and the overlap may lead to a deformity Just need to suture the overlying skin, the cartilage does not need to be sutured Timing of repair Berk et al looked at 372 patients, 204 of whom had followed up 7 days later in 2004 They concluded that wounds that were closed within 24 hours had no increased risk of infection if it is a clean laceration Visual analog scale (0-100mm) Quinn et al 1995 Cosmetic appearance score From Wound Registry: Hollander Wound Evaluation Scale Assessing outcomes in facial plastic surgery (Rhee et al 2008) Review of all outcomes in facial plastic surgery Other than the Quinn VAS and Hollender Wound Evaluation Score, there are 4 other scales Of note the Quinn and Hollander scales are reliable (good inter and intra rater reliability), and validated (use of lit reviews, expert opinions) Ethibond vs Monofilament (Quinn 1998) Paid for by manufacturers of Ethibond 136 randomized patients to pediatric ER to either 5-0/6-0 closure or ethibond Reassess wound at 10days, 3mos, 1 year Use of Hollander wound score and VAS by 2 research RNs on follow-up and a validated wound VAS by a cosmetic plastic surgeon (based on photographs) Results of Ethibond closure No significant difference in optimum wound scores (73% for Ethibond, 68% suture) or VAS No correlation between 10 days and 3 mos, but excellent correlation between 3 mos and 1 year in appearance of wound Essentially all future studies use 3 mos f/u in their methods based on the results of this study Consideration: application of Ethibond cannot be within wound, cannot use on lips Cochrane review of tissue adhesives (2001, updated 2007) Used VAS and cosmetic wound score to examine a total of 889 lacerations, with 364 having follow-up 9-12 mos out from 9 studies No difference in wound scores noted Less pain involved with application and absence of suture removal Time to apply adhesive was ~5 minutes shorter than suturing There was a slightly higher risk of dehicience with adhesive (6.6% vs 2.2%) which was stat sig Fast gut vs Nylon closure (Luck 2008) Pediatric ED patients comparing suture choices Wounds 1-5cm without irreg borders, 1-2 layer closure Follow-up at 5-7days and 3 months Use validated VAS for cosmesis by 3 blinded observers (peds ED attendings) based on photographs, and parental VAS 90 patients total randomized with 60% f/u rate at 3 months Luck et al. results Mean VAS was 92mm (FG) and 93mm (N) Parental VAS was 86mm (FG) and 91mm (N) Parental survey found fast gut to be more convenient (91% vs 75%) and were more likely to request it in the future (96% vs 79%) 3 parents (13%) perceived complications in fast gut group compared to nylon (1 large scar after dehiscience, 2 with premature unraveling) Limitations 70% of fast gut patients had at least one suture that needed to be removed at 5-7d follow-up Photographs do not show 3D anatomy Only 60% follow-up rate Note that the parental VAS was 5mm higher for the nylon group - this was statistically insignificant based on the study, but is it clinically insignificant? Comparison of nylon, fast gut and Dermabond (Holger 2004) 146 patients randomized to each group 9-12 mos of follow-up, ~60% follow-up rate VAS used to assess wound No significant differences between 3 groups in wound outcome Metanalysis of absorbable vs nonabsorbable suture (Al-Abdullah 2007) 2 studies from Holger (2004) and Karounis (2004) showed no difference in long term cosmetic outcome scores when results were pooled together 3 studies pooled showed no difference in hypertrophic scarring 7 studies pooled together revealed no difference in infection rate Choice of closure method Whatever method you choose, make sure you perform it correctly (dermabond, steri strips) Fast gut may have an unpredictable absorption rate, if it stays in too long, track marks may form as well as prolonged erythema Dermabond cannot get into the wound 6-0 Prolene is a good choice, gives control over wound closure and suture removal Choice of irrigant/cleanser Normal saline, water, Shur-Clens shown to be least toxic to fibroblasts and keratinocytes in vitro (Wilson et al 2005) Povidine-iodine and hydrogen peroxide among the most toxic, but iodine not shown to prevent infection (Gravett et al 1987) Since commercial detergents and normal saline have been shown to be equally effective in preventing infection, normal saline is adequate for cleaning of the wound Role of antimicrobials In animal models 105 colonies/g tissue Typical ED laceration (clean) has 102/g tissue Systemic antimicrobials for complicated wounds (next slide) Dire et al found a decreased infection rate with the application of triple abx ointment (4.5%) vs bacitracin (5.5%) vs silvadene (12%) vs petrolatum (17%) Assess risk factors Extremes of age DM, renal disease Immunocompromised state Malnutrition Obesity Bite injuries (Amox/clav x 3-5 days to cover Eikenella, Pasturella) Crush injuries Grossly contaminated wounds Laceration involving muscle Open fractures Intraoral lacerations (5 days of PCN adequate) Appropriate use of antibiotics Nakamura and Daya did a review of clinical trials involving the use of anitbiotics They concluded that antimicrobials should be used in open fractures, intra-oral wounds and bites In addition, since there are no randomized trials for assessing risk factors, it is accepted that it would be appropriate to use antimicrobials for the previously mentioned risk factors Pearls and techniques Zen-like - need to visualize and practice entering and exiting the skin at 90 degree angles Formation of a “square” with the suture Wound eversion is necessary Have the proper equipment - need fine instruments with delicate lacerations, small children Most of all, be patient and achieve a correct closure, spending an extra 10 minutes will make for a better outcome Practice Carry a needle driver in your pocket Practice opening and closing without using your fingers This will make it more efficient and help prevent inadvertently pulling the needle out Conclusions Proper suture placement and eversion of wound is essential for optimum scar outcome Antibiotics have not been shown to be effective in noncontaminated wounds Closure with fast gut appears to have similar wound outcomes when compared with non-absorable sutures at 1 year Dermabond has similar wound outcomes, but requires special attention when applying Cleaning of the wound with normal saline is adequate to prevent infection