Poisoning: An Overview - UNC School of Medicine
advertisement

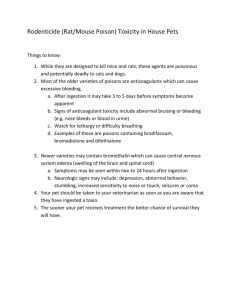
Toxicology UNC Emergency Medicine Medical Student Lecture Series Objectives • General approach to the poisoned patient • Toxidromes • Specific antidotes • Decontamination and enhanced elimination General Approach • • • • • • ABC’s History Physical examination Labs, imaging Diagnosis, antidotes Disposition ABC’s Airway • Airway obstruction can cause death after poisoning – Flaccid tongue – Aspiration – Respiratory arrest • Evaluate mental status and gag/cough reflex • Airway interventions – – – – – – Sniffing position Jaw thrust Head-down, left-sided position Examine the oropharynx Clear secretions Airway devices: nasal trumpet, oral airway • Intubation? – Consider naloxone first Breathing • • • • • Determine if respirations are adequate Give supplemental oxygen Assist with bag-valve-mask Check oxygen saturation, ABG Auscultate lung fields – Bronchospasm: Albuterol nebulizer – Bronchorrhea/rales: Atropine – Stridor: Determine need for immediate intubation Circulation • • • • IV access Obtain blood work Measure blood pressure, pulse Hypotension treatment: – Normal saline fluid challenge, 20 mL/kg – Vasopressors if still hypotensive – PRBC’s if bleeding or anemic • Hypertension treatment: – Nitroprusside, beta blocker, or nitroglycerin • Continuous ECG monitoring – Assess for arrhythmias, treat accordingly Supportive Care • • • • Foley catheter Rectal temperature Accucheck, treat hypoglyemia Coma cocktail – Thiamine: 100 mg IV, before dextrose – Dextrose: 50 grams IV push – Naloxone: 0.01 mg/kg IV Supportive Care • Treat Seizures – Lorazepam 2 mg IV, may repeat as needed – Dilantin 10 mg/kg IV • Control agitation – Haldol 5-10 mg IM – Ativan 2-4 mg IM or IV – Geodon 20 mg IM • Think about trauma REASSESS . . . frequently History • • • • • • What, when, how much, why? Rx, OTC, herbals, supplements, vitamins Talk to family, friends, EMS Pill bottles, needles, beer cans, suicide note Call pharmacy Allergies, medical problems Physical examination • • • • • • • • Vital signs: BP, HR, RR, T, O2 sat Mouth: odors, mucous membranes Pupils Breath sounds Bowel sounds Skin Urination/defecation Neurologic exam Essential Laboratory Tests • • • • • • • • • • Electrolytes Glucose BUN and creatinine LFT’s, CK Urinalysis, urine drug screen Etoh, alcohol screen Serum osmolality Acetaminophen, salicylates Specific drug levels Pregnancy test Anion Gap • Na – (HCO3 + Cl) • Normal: 8-12 mEq/L • Causes: – – – – – – – – Methanol Uremia DKA Paraldehyde, phenformin Iron, isoniazid, ibuprofen Lithium, lactic acidosis Ethylene glycol Strychnine, starvation, salicylates Osmolar Gap • • • • Calculated osmolality – measured osmolality 2(Na) + glucose/18 + BUN/2.8 Normal = 285-290 mOsm/L Gap > 10 mOsm/L suggests the presence of extra solutes: – Ethanol, methanol – Ethylene glycol, isopropyl alcohol – Mannitol, glycerol • Clinical Pearl: Anion gap acidosis with an osmolar gap should suggest methanol or ethylene glycol poisoning Electrocardiogram • Prolonged QRS – – – • Sinus bradycardia/AV block – – – – • TCAs Phenothiazines Calcium channel blockers Beta-blockers, calcium channel blockers TCAs Digoxin organophosphates Ventricular tachycardia – – – – – Cocaine, amphetamines Chloral hydrate Theophylline Digoxin TCAs Diagnosis • • • • May not identify ingested substance(s) Provide ABCs and supportive care Give antidote when appropriate Call regional poison control center – Carolinas Poison Center, Charlotte – 800-848-6946 Disposition • • • • Case-based ICU admission Period of observation Psychiatric evaluation Toxidromes Cholinergic Toxidrome Diarrhea Urination Miosis Bradycardia Bronchospasm Emesis Lacrimation Limp Salivation, sweating Salivation Lacrimation Urination Defecation GI upset Emesis Cholinergics • Organophosphates – Irreversibly bind cholinesterases • Carbamate – Reversibly bind cholinesterases, poor CNS penetration • Muscarinic and nicotinic effects • Pesticides, nerve agents – – – – Military personnel Field workers, crop dusters Truckers Pest control, custodial workers • Antidote – Atropine for muscarinic effects – Pralidoxime reverses phosphorylation of cholinesterase Anticholinergics • • • • • Atropine Scopolamine Glycopyrrolate Benztropine Antispasmotics – – – – Dicyclomine Hyoscyamine Oxybutynin clidinium • TCAs • Mydriatics • Antihistamines – – – – – – Chlorpheniramine Cyproheptadine Hydroxyzine Diphenhydramine Meclizine promethazine • Antipsychotics – Clozapine – Olanzapine – Thioridazine • Jimson weed Anticholinergic Toxidrome • • • • • • • • • • • Dry mucus membranes (Dry as a bone) Mental status changes (Mad as a hatter) Flushed skin (Red as a beet) Mydriasis (Blind as a bat) Fever (Hot as a hare) Tachycardia Hypertension Decreased bowel sounds Urinary retention Seizures Ataxia Toxidromes • Opioids – Respiratory depression – Miosis – Hypoactive bowel sounds • Sympathomimetics – – – – – Hypertension Tachycardia Hyperpyrexia Mydriasis Anxiety, delirium Clinical Pearl: Sweating differentiates sympathomimetic and anticholinergic toxidromes Antidotes • • • • • • • • • • Acetaminophen Organophosphates Anticholinergic Arsenic, mercury, gold Benzodiazepines Beta blockers Calcium channel block Carboxyhemoglobin Cyanide Digoxin N-acetylcysteine Atropine, pralidoxime physostigmine dimercaprol flumazenil glucagon calcium 100% O2 nitrite, Na thiosulfate digoxin antibodies Antidotes • • • • • • • • • • Ethylene glycol Heparin Iron Isoniazid Methanol Methemoglobin Opioids Salicylate TCA’s Warfarin fomepizole, HD protamine deferoxamine pyridoxime fomepizole, HD methylene blue naloxone alkalinization, HD sodium bicarbonate FFP, vitamin K Decontamination Principles of Decontamination • External – Protect yourself and others – Remove exposure – Irrigate copiously with water or normal saline – Don’t forget your ABC’s • Internal – Patient must be fully awake or intubated – Most common complication is aspiration – Very little evidence for their use Decontamination • Skin – Protect yourself and other HC workers – Remove clothing – Flush with water or normal saline – Use soap and water if oily substance – Chemical neutralization can potentiate injury – Corrosive agents injure skin and can have systemic effects Decontamination • Eyes – – – – – remove contact lens Flush copiously with water or normal saline Use local anesthetic drops Continue irrigation until pH is normal Slit lamp and fluorescein exam Decontamination • Inhalation – Give supplemental humidified oxygen – Observe for airway obstruction – Intubate as necessary GI Decontamination • Syrup of ipecac – Within minutes of ingestion – Aspiration, gastritis, Mallory-Weiss tear, drowsiness – Rarely, if ever, given in ED • Gastric lavage – – – – – Does not reliably remove pills and pill fragments Used 30-60 minutes after ingestion Useful after caustic liquid ingestion prior to endoscopy Not used for sustained release/enteric coated ingestions Perforation, nosebleed, vomiting, aspiration • Recent studies suggest that activated charcoal alone is just as effective as gut emptying followed by charcoal. GI Decontamination • Activated charcoal – – – – – Limits drug absorption in the GI tract Within 60 minutes of ingestion Patient must be awake or intubated Vomiting, aspiration, bezoar formation Contraindication: bowel obstruction or ileus with distention – 1 gram/kg PO or GT Activated Charcoal • Not good for: – – – – – – Lithium Iron Alcohols Lead Hydrocarbons Caustics GI Decontamination • Cathartics – – – – Hasten passage of ingestions or AC Contraindications: obstruction or ileus Severe fluid loss, hypernatremia, hyperosmolarity 10% magnesium citrate 3ml/kg or 70% sorbitol 1-2 …./kg • Whole bowel irrigation – Large ingestions, SR or EC tablets, packers (ex. cocaine) – Contraindications: obstruction or ileus – Aspiration, nausea, may decrease effectiveness of charcoal Enhanced Elimination • Urinary manipulation – Forced diuresis – Alkalinization • Repeat-dose activated charcoal – Very large ingestions of toxic substance – Sustained release and enteric coated preparations • Carbamazepine, phenobarbital, phenytoin • Salicylate, theophylline, digitoxin • Hemodialysis, Hemoperfusion • Peritoneal dialysis, Hemofiltration Enhanced Elimination • Does the patient need it? – Severe intoxication with a deteriorating condition despite maximal supportive care – Usual route of elimination is impaired – A known lethal dose or lethal blood level – Underlying medical conditions that can increase complications Specific Toxins • Acetominophen • Salicylates • Tricyclic Antidepressants (TCA) Acetominophen (apap) Magic number to remember is 140 • Max dose: – 4g/day adults – 90 mg/kg day kids • Peak serum levels: 4 hours after overdose • What are the three methods of APAP metabolism? – Glucuronidation (90% normal thru pathway) – Sulfonation – P450 mixed oxidase enzymes (5% nl thru pathway) Acetominophen (apap) • Toxicity • 140mg/kg acute ingestion • Direct hepatocellular toxicity with centrolobular distribution (hepatic vein) • Can also have renal damage and pancreatitis Stages of Tylenol Toxicity • I (0-24hrs): n/v, but most asymptomatic • II latent stage (24-48hrs): subclinical increase in ast/alt/bili • III hepatic stage (3-4dys): liver failure, ruq pain, vomiting, jaundice, coagulopathy, hypoglycemia, renal failure, metabolic acidosis • IV recovery stage (4dys-2wks): resolution of hepatic dysfunction Need 4 hour level and N-acetylcysteine (NAC) • Dx: 4 hour level compared to the Rumack and Matthews nomogram • 150ug/ml at 4 hours • Rx: NAC 140mg/kg then 70mg/kg every 4 hours for 17 doses • We Have PO and IV dosing • Only useful for one time ingestion (not chronic ingestions) Acetominophen (apap) • If time of ingestion unknown, draw level immediately and again at 2-4 hours. • Labs: LFTs, coags, lytes, aspirin, ETOH, tox screen NAC indications • Ingestions with potential toxicity • Late presentations with potential or ongoing toxicity • Chronic overdose with evidence of hepatic damage Tylenol Overdose Disposition • Admit if….. – Known toxicity / potential toxic levels – Lab evidence of hepatic damage – Unknown time of ingestion and sx consistent with toxicity – Unknown ingestion time with measurable acetaminophen levels. Salicylates (asa) • • • • • • Weak acid, rapidly absorbed Enteric coated has delayed absorption Toxic dose: 160 mg/kg Lethal dose 480 mg/kg Mixed respiratory alkalosis-metabolic acidosis Stimulates respiratory drive causing hyperventilation, but limits ATP production metabolic acidosis • Oil of wintergreen, 1ml = 1400mg Salicylates Symptoms • Tachypnea, tachycardia, hyperthermia • Resp alkalosis-metabolic acidosis • Altered serum glucose • AG metabolic acidosis (MUDPILES) • Dehydration (vomiting, tachypnea, sweating) • Abd pain/n/v • Tinnitus, hearing loss • lethargy, seizures, altered mental status • Noncardiogenic pulmonary edema Evaluation of ASA Overdose • Lytes, ABG, LFTs, CBC, preg.test, urine PH • Serum salicylate levels (toxicity at 25mg/dl) • Toxicity correlates POORLY with levels • Evaluation with DONE nomegram based on single ingestion of regular ASA at levels drawn 6 hrs after ingestion • Underestimates toxicity in cases of severe acidemia or chronic ingestion Therapy for ASA Overdose • ABC’s • Activated charcoal • Urinary alkalinization (start if serum level is greater than 35mg/dl) – 3 amps bicarbinate in 1 L D5W at 150 ml/hr • By increasing urinary pH to greater than 8, ASA gets trapped in tubes and cannot be reabsorbed • Dialysis for severe acidemia, volume overload, pulmonary edema, cardiac or renal failure, seizures, coma, levels > 100mg/dl in acute ingestion, or > 60-80 mg/dl in chronic ingestion Disposion for ASA Overdose • Pt gets charcoal and remain asymptomatic after 6-8 hours = Possible D/C • Sustained release requires longer observation period • Pts with toxic levels, symptomatic, or develop symptoms = Admission TCA (Tricyclic Antidepressants) • Leading cause of death by intentional overdose • Blocks sodium channels • Death by cardiovascular dysrhythymias and cardiovascular collapse • Most TCA’s have anticholinergic effects – Dry skin, blurry vision, hot • Severe OD: hypotension, seizures, respiratory depression • In severe cases: ARDS, rhabdomyolisis, DIC GET AN EKG What do you see? Prolonged QRS, sinus tachycardia, “tall R in R” – tall R wave in lead aVR Treatment of TCA Overdose • Sodium Bicarbinate – Initial bolus of 2 amps – Drip 3 amps in 1 L D5W at 150 ml/hr • • • • Titrate for serum pH of 7.45-7.5 IV fluids Lidocaine for perisistent arrhythymias AVOID Class Ia drugs (procainimide quinidine) Thank You! Any Questions? References • Poisoning & Drug Overdose, California Poison Control System. KR Olson, 3rd edition, Appleton & Lange, 1999. • Emergency Medicine Board Review Series. L Stead, Lippincott Williams & Wilkins, 2000. • Emergency Medicine, A comprehensive study guide. Tintinalli, 6th edition, McGraw Hill, 2004.