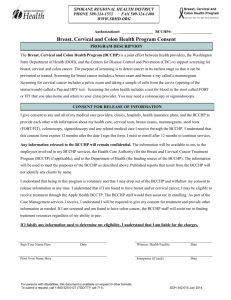
serial #: ph rfp 12-023, breast and cervical cancer
advertisement

NOTICE OF SOLICITATION SERIAL #: PH RFP 12-023 REQUEST FOR PROPOSAL FOR: BREAST AND CERVICAL CANCER EARLY DETECTION SCREENING, DIAGNOSTIC, & TREATMENT SERVICES Notice is hereby given that sealed proposals will be received by the Maricopa County Department of Public Health, 4041 N. Central Avenue, #1400, Phoenix, AZ 85012, until 2:00 P.M. Arizona time on FEBRUARY 24, 2012 for the furnishing of the following services for Maricopa County. Proposals will be opened by the Public Health Procurement Officer (or designated representative) at an open, public meeting at the above time and place. To participate in this solicitation process, vendors shall register through BidSync.com. To register with BidSync, please go to www.BidSync.com and click on the orange ‘Register’ link. Registration has no cost, and will allow you to access all of the proposal information, proposal documents, and receive proposal notifications. For assistance with registration, please contact BidSync Vendor Support Department via phone or email, during regular business hours: 1-800-990-9339 or agencysupport@BidSync.com All Proposals must be signed, sealed and addressed to the Maricopa County Department of Public Health, 4041 N. Central Avenue, #1400, Phoenix, AZ 85012, and marked “SERIAL #: PH RFP 12-023 REQUEST FOR PROPOSAL FOR: BREAST AND CERVICAL CANCER EARLY DETECTION SCREENING, DIAGNOSTIC, & TREATMENT SERVICES.” The Maricopa County Procurement Code (“The Code”) governs this procurement and is incorporated by this reference. Any protest concerning this Request for Proposal must be filed with the Procurement Officer in accordance with Section MC1-905 of the Code. ALL ADMINISTRATIVE INFORMATION CONCERNING THIS REQUEST FOR PROPOSAL CAN BE LOCATED AT http://www.maricopa.gov/materials ANY ADDENDA TO THIS REQUEST FOR PROPOSAL WILL BE POSTED THROUGH THE MARICOPA COUNTY MATERIALS MANAGEMENT WEB SITE AS WELL AS ONLINE AT WWW.BIDSYNC.COM. PROPOSAL ENVELOPES WITH INSUFFICIENT POSTAGE WILL NOT BE ACCEPTED BY THE MARICOPA COUNTY DEPARTMENT OF PUBLIC HEALTH DIRECT ALL INQUIRIES TO: CHERYL RENTSCHELER PROCUREMENT OFFICER TELEPHONE: (602) 506-6886 EMAIL: cherylrentscheler@mail.maricopa.gov NOTE: MARICOPA COUNTY PUBLISHES ITS SOLICITATIONS ONLINE AND THEY ARE AVAILABLE FOR VIEWING AND/OR DOWNLOADING AT THE FOLLOWING INTERNET ADDRESS: http://www.maricopa.gov/Materials/solicitation.aspx Page 1 of 73 SERIAL #: PH RFP 12-023 TABLE OF CONTENTS NOTICE TABLE OF CONTENTS SECTIONS: 1.0 INTENT 2.0 BACKGROUND 3.0 WWHP ELIGIBILITY 4.0 SCOPE OF WORK 5.0 SPECIAL TERMS & CONDITIONS ATTACHMENTS: ATTACHMENT A PRICING ATTACHMENT B AGREEMENT/SIGNATURE PAGE ATTACHMENT C REFERENCES EXHIBITS: EXHIBIT 1 VENDOR REGISTRATION PROCEDURES EXHIBIT 2 LETTER OF TRANSMITTAL SAMPLE EXHIBIT 3 WWHP CLINICAL GUIDELINES EXHIBIT 4 SCHEDULE A Page 2 of 73 SERIAL #: PH RFP 12-023 REQUEST FOR PROPOSAL FOR: 1.0 BREAST AND CERVICAL CANCER EARLY DETECTION SCREENING, DIAGNOSTIC, & TREATMENT SERVICES INTENT: The Maricopa County Department of Public Health’s (MCDPH), Well Woman Healthcheck Program (WWHP) is seeking proposals from qualified primary health care providers and/or institutions (private practices, multi-specialty practices, hospitals, and other health care provider institutions) with a history of, or capability of, providing breast and cervical cancer screening, diagnostic, and treatment services to women 40 years of age and older who are either uninsured or underinsured and whose household income falls at or below 250% of the Federal Poverty Level Guidelines. Successful candidates will provide breast and cervical cancer screening exams, including clinical breast exams, screening mammography, breast selfexam education, pelvic exams, and pap smears, and diagnostic services, in accordance with their capabilities, as well as completion of all program forms. Those with the capacity shall also provide treatment services. Multiple contracts with successful candidates may be awarded. Other governmental entities under agreement with the County may have access to services provided hereunder (see also Section 4.4 below). The County reserves the right to add additional contractors, at the County’s sole discretion, in cases where the currently listed contractors are of an insufficient number or skill-set to satisfy the County’s needs or to ensure adequate competition on any project or task order work. 2.0 BACKGROUND: The Arizona Department of Health Services, Bureau of Health Systems Development, is funded through a cooperative agreement with Centers for Disease Control and Prevention (CDC) and the State of Arizona to provide a statewide breast and cervical cancer screening program, known locally as Well Woman HealthCheck (WWHP). The WWHP is part of the National Breast and Cervical Cancer Early Detection Program (NBCCEDP), which was authorized when the U.S. Congress passed the Breast and Cervical Cancer Mortality Prevention Act of 1990, Public Law 101-354. The Act not only established CDC’s NBCCEDP; it also provided the foundation of the NBCCEDP’s policies and requirements in regard to the program eligibility and operations. The Breast and Cervical Cancer Mortality and Prevention Act of 1990 strictly prohibit the use of NBCCEDP funds for cancer treatment. In October 2000, U.S Congress passed the Breast and Cervical Cancer Prevention and Treatment Act of 2000, Public Law 106-354; this law gives states the authority to provide optional Medicaid coverage to certain breast and cervical cancer patients. In the spring of 2001, the Arizona Legislature passed H.B. 2194 that authorizes the Arizona Health Care Cost Containment System (AHCCCS), effective January 1, 2002, to provide certain women diagnosed through the WWHP with breast, pre-cancerous cervical lesions and cervical cancer with cancer treatment. To be eligible for treatment, women must be screened through the Well Woman HealthCheck Program on or after April 1, 2001, under the age of 65, a resident of Arizona, have no credible health insurance coverage, and be a U.S. citizen or qualified alien. 3.0 WWHP ELIGIBILITY: 3.1 3.2 To be eligible for breast and cervical cancer screening and diagnostic services under the Well Woman HealthCheck Program all women regardless of age, must be between 101% and 250% of the Federal Poverty Level guidelines; a resident of Arizona for at least one-day with the intention of establishing permanent residence in Arizona; and be uninsured or under-insured. Under-insured is defined as health insurance that does not cover preventative healthcare, or the co pay exceeds $100.00. The women enrolled in the WWHP must mirror the racial/ethnic demographics of the county in which the program resides. Women 65 years of age or older: Women 65 years of age or older who do not have Medicare Part B may be enrolled. Women with an intact cervix or history of cervical neoplasia are eligible to receive a Pap test screening in accordance to the WWHP cervical screening policy. The annual clinical breast examination and pelvic examination are included in the office visit reimbursement, an allowable expense that may be included in the Contractor’s Expense Report. However, if diagnosed with cancer this population of women are not eligible to receive treatment services under the Breast and Cervical Cancer Prevention and Treatment Act 2000. These women, when Page 3 of 73 SERIAL #: PH RFP 12-023 3.3 3.4 3.5 possible, should be referred to healthcare organizations or agencies providing benefits provided under Medicare Parts A and B. If a client is unable to pay Medicare premiums, she may be eligible for assistance under AHCCCS. Women 50-64 years of age: Women 50-64 years of age are the priority population for mammography screening services. Women 50 years of age and older must account for 75% of the mammography services utilizing funding provided to WWHP contractors. The focus for this priority population includes screening with initial program Pap tests who have rarely (within the past 3 years) or never been screened for cervical cancer. Women 40-49 years of age: Mammography services, utilizing State funding, will be provided to women 40-49 years of age. Women with an intact cervix or history of cervical neoplasia are eligible to receive Pap test screening in accordance with the WWHP cervical screening policy. The annual clinical breast examination and pelvic examination are included in the office visit reimbursement. Women under 40 years of age: Women less than 40 years of age may only be enrolled for breast cancer screening and diagnostic services if they exhibit clinically confirmed symptoms of breast cancer. Breast Cancer symptoms include: Painless lump or mass Spontaneous, unilateral, serous or serosanguinous nipple discharge Spontaneous, unilateral, bloody nipple discharge Dermatitis of nipple/areola Change in contour of breast Dimpling of the breast skin Nipple retraction (this does not include women with a history of inverted nipples) Fixation of a mass to the chest wall or adjacent tissue Edema and erythema of breast skin Axillary adenopathy Once the client’s abnormality has been resolved and the recommendation is to return to routine screening intervals the client should be removed from WWHP rolls and referred t the local Title V (Maternal and Child Health Service Block Grant) or Title X (Arizona Family Planning) program. Women 21-64 years of age may be screened for cervical cancer. 4.0 SCOPE OF WORK: 4.1 SERVICE REQUIREMENTS: 4.1.1 SCREENING SERVICES: The Contractor shall provide the following breast and cervical cancer screening services: Breast - annual clinical breast examination (CBE) and screening mammography; Cervical - pelvic examination and Pap smear. All services shall be completed in accordance with the WWHP Clinical Guidelines (Exhibit 3). 4.1.2 DIAGNOSTIC SERVICES: The Contractor shall provide the following diagnostic services, as appropriate, using the recommendations provided in the WWHP Clinical Guidelines, for women with abnormal screening results: diagnostic mammography; breast ultrasound, fine needle aspiration biopsy, excisional biopsy, surgical consultation, colposcopy, colposcopy-directed biopsy, endocervical curettage (ECC), endometrial biopsy (EMB), cold knife conization (CKC), and diagnostic LEEP. If the Contractor does not have the capacity to perform diagnostic services, the Contractor shall maintain a contract with another provider who will provide the necessary diagnostic services. 4.1.3 The Contractor shall submit a request to the MCWWHP case manager for authorization prior to obtaining a surgical consultation or performing advanced diagnostic procedures, including breast biopsy, endometrial biopsy, cold knife conization CKC) or LEEP.The contractor may perform diagnostic mammogram, breast ultrasound, colposcopy, ECC, or cervical biopsy without prior authorization from the MCWWHP case manager. 4.1.4 TREATMENT SERVICES: The Contractor shall provide treatment services, such as radiation, chemotherapy, lumpectomy, mastectomy, or LEEP, in accordance with the Contractor’s capacity to do so. 4.1.5 Treatment is covered for eligible legal citizens of the United States and qualified aliens by the Breast and Cervical Cancer Treatment Program (BCCTP), through the Arizona Page 4 of 73 SERIAL #: PH RFP 12-023 4.1.6 4.1.7 4.1.8 4.1.9 4.1.10 4.1.11 4.1.12 4.1.13 4.1.14 4.1.15 Health Care Cost Containment System (AHCCCS). For clients diagnosed with abnormalities of the breast or cervix, who are not eligible for BCCTP, contractors are responsible for entering into a sliding fee scale agreement based on the woman’s income and ability to pay or making appropriate referrals to other providers willing to donate or enter into a sliding scale agreement with clients. The Contractor must be an AHCCCS registered provider. In the event that a woman’s diagnostic work-up is positive for cancer or pre-cancerous cervical lesions, and the client has been approved for BCCTP through AHCCCS, AHCCCS will cover the cost of treatment and diagnostic procedures and can pay AHCCCS registered providers directly for services rendered. The Contractor shall use an effective system to schedule client appointments in a timely manner and notify them about test results and when follow-up appointments are necessary. The Contractor shall provide client test results to MCWWHP case managers in a timely manner and collaborate with them to provide appropriate and timely follow-up to clients with abnormal screening results. To assure quality and meet CDC requirements, the Contractor shall comply with the following: 4.1.8.1 The time from screening to diagnosis, or a recommendation to return to routine screening, shall be 60 or less calendar days. If this time frame is not met, services will not be reimbursed. 4.1.8.2 The time from diagnosis to treatment start for breast cancer and invasive cervical cancer shall be 60 or less calendar days. The time from diagnosis to treatment start for cervical lesions requiring treatment shall be 90 or less calendar days. If this time frame is not met, services will not be reimbursed. The Contractor shall submit to the WWHP manager complete, accurate, and legible copies of all data requirements and program forms within 30 days from the completion of the screening and/or diagnostic follow-up and/or treatment procedure/exam. The Contractor shall respond to all requests for missing or incomplete data within 48 hours after the request has been made. The contract amount is not a guaranteed amount. Each Contractor will be given a funding amount at the beginning of the fiscal year which is their actual budgeted amount. Contractors are responsible for tracking expenditures from their funding amount on an ongoing basis. Contractors may request an increase to their funding amount anytime throughout the year prior to reaching their funding limit, by emailing a request to the MCWWHP program manager. Requests will be reviewed and may be approved if funds are available. Contractors will not be reimbursed for services that exceed their funding amount. The Contractor shall attend required MCDPH WWHP meetings. The Contractor shall maintain an ongoing tracking of “in-kind match.” “In-kind match” is defined as non-federally funded, materials, services, and time that directly support WWHP activities. “In-kind match” is NOT TO INCLUDE treatment services. Completed “in-kind match” contribution information needs to be submitted quarterly in October (for July-September), January (for October-December), April (for January-March) and August (for the April-June). Contractors must be willing to accept compensation for each enrollee on a fee for service basis, based on Medicare Part B allowable costs. Women enrolled in WWHP shall not be charged for covered services. Reimbursement rates are formulated annually by the CDC (Exhibit 4). An updated schedule of maximum reimbursement rates will be provided to the Contractor after the rates are received by MCDPH from the CDC in April. If a woman needs a diagnostic or treatment service that is not a covered service under this program, the Contractor will provide services applying the AHCCCS rate. The Contractor shall submit to annual audits of provider performance and implement plans to ensure that quality standards are followed for mammography and cytology procedures, as well as for program policy and procedures. Quality standards shall include: 4.1.15.1 The Contractor will obtain and maintain the following current documents: license(s) or certification(s), and liability insurance. This information may be requested as expiration dates occur. Page 5 of 73 SERIAL #: PH RFP 12-023 4.1.16 4.1.17 4.2 4.1.15.2 Personnel: If Physicians are providing services under this contract they shall be either an M.D. or D.O. and be currently licensed under the provisions of the Arizona Revised Statutes, Title 32, Chapter 13 or 17. Midlevel personnel providing services shall be registered, licensed or board certified in Arizona in their respective fields, as applicable under the provisions of the Arizona Revised Statues, Title 32, Chapter 15 (nurse practitioners) or Chapter 25 (physician’s assistants). 4.1.15.3 Facility: (1) All mammography facilities used by the contractor and its subcontractors shall be certified by the Food and Drug Administration in compliance with the Mammography Quality Standards Acts of 1992, maintain annual American College of Radiology (ACR) accreditation, and be inspected annually by the Arizona Radiation Regulatory Agency in accordance with Arizona State Statute. To be approved for payment by the Office/WWHP, all reports must be submitted using the language of the ACR lexicon, also known as BI-RADS™. (2) All laboratory facilities used by the contractor and its subcontractors shall adhere to the standards of the Clinical Laboratory Improvement Act (CLIA) (1988), and maintain the appropriate CLIA certification. To be approved for payment by the MCWWHP, all Pap test reports must be submitted using the Bethesda System (TBS) of reporting. The Contractor shall respond within 48 hours to communications concerning quality assurance issues. Special consideration will be given to facilities with a history of outreach and service delivery to the target population and women’s health care programs. Preference will be given to those providers targeting uninsured or underinsured women, women at or below 250% of the Federal Poverty Level, those who do not qualify for other programs, those who are 40 years of age or older, and to facilities that are located to best provide geographic coverage to Maricopa County. Preference will also be given to facilities that have bilingual (English/Spanish or English/Asian language) staff persons. COMPENSATION/FEES: Compensation shall be on a fee for service basis as determined by Medicare’s allowable compensation costs for annual breast and cervical screening services (Exhibit 4). No minimum number of clients is guaranteed. Payment will occur after all required data and program forms are submitted and approved within the required 30 day timeframe. The following is a list of typical services: 4.2.1 Clinical breast examination 4.2.2 Pelvic examination 4.2.3 Unilateral Mammogram 4.2.4 Bilateral Mammogram 4.2.5 Breast ultrasound 4.2.6 Aspiration of cysts of breast 4.2.7 Biopsy of breast, needle core (surgical procedure only) and pathology 4.2.8 Incisional biopsy of breast and pathology 4.2.9 Excisional breast biopsy 4.2.10 Fine Needle Aspiration with/without preparation of smears and pathology 4.2.11 Pap smear, reported in Bethesda 4.2.12 Colposcopy without biopsy 4.2.13 Colposcopy with biopsy and/or endocervical curettage surgical procedure only and Pathology 4.2.14 Endocervical Curettage (ECC) 4.2.15 Endometrial biopsy (EMB) 4.2.16 Cold Knife Conization (CKC) 4.2.17 Diagnostic LEEP (loop electrode excision procedure) 4.2.18 Consultation visit – 20 minutes face to face with patient 4.2.19 Appropriate referral for treatment, as needed, to providers willing to donate or enter into a sliding scale agreement with clients. Page 6 of 73 SERIAL #: PH RFP 12-023 4.3 INVOICES AND PAYMENTS: 4.3.1 The Contractor shall submit completed minimum data elements (MDE)s along with supporting documentation such as lab reports, progress/diagnostic work-up notes, and/or pathology reports within 30 days following services. Reimbursement will be denied for services billed after 45 days of the date of service. 4.3.2 The Contractor is solely responsible for its own corporate medical direction, promotion, advertising, revenue disbursement, information systems, oversight, personnel/human resources, administrative services, and any and all tasks, duties, and expenses related to or associated with their corporate operation. 4.3.3 The Contractor shall be responsible for any and all taxes, permit, or authorizations that may be required by laws of the federal, state, or local government. 4.3.4 The Respondent shall submit two (2) legible copies of their detailed invoice before payment(s) can be made. At a minimum, the invoice must provide the following information: 4.4 Company name, address and contact County bill-to name and contact information Contract Serial Number County purchase order number Invoice number and date Payment terms Date of service or delivery Quantity Contract Item number(s) Description of Purchase (services) Pricing per unit of service Extended price Total Amount Due 4.3.5 Problems regarding billing or invoicing shall be directed to the using agency as listed on the Purchase Order 4.3.6 Payment shall be made to the Contractor by Accounts Payable through the Maricopa County Vendor Express Payment Program. This is an Electronic Funds Transfer (EFT) process. After Contract Award the Contractor shall complete the Vendor Registration Form located on the County Department of Finance Vendor Registration Web Site (http://www.maricopa.gov/finance/vendors). 4.3.7 EFT payments to the routing and account numbers designated by the Contractor will include the details on the specific invoices that the payment covers. The Contractor is required to discuss remittance delivery capabilities with their designated financial institution for access to those details. TAX: (SERVICES) No tax shall be levied against labor. It is the responsibility of the Contractor to determine any and all taxes and include the same in proposal price. 4.5 STRATEGIC ALLIANCE for VOLUME EXPENDITURES ($AVE): The County is a member of the $AVE cooperative purchasing group. $AVE includes the State of Arizona, many Phoenix metropolitan area municipalities, and many K-12 unified school districts. Under the $AVE Cooperative Purchasing Agreement, and with the concurrence of the successful Respondent under this solicitation, a member of $AVE may access a contract resulting from a solicitation issued by the County. If you do not want to grant such access to a member of $AVE, please so state in your proposal. In the absence of a statement to the contrary, the County will Page 7 of 73 SERIAL #: PH RFP 12-023 assume that you do wish to grant access to any contract that may result from this Request for Proposal. 5.0 SPECIAL TERMS & CONDITIONS: 5.1 CONTRACT TERM: This Request for Proposal is for awarding a service contract to cover a three (3) year term. 5.2 OPTION TO RENEW CONTRACT: The County may, at its option and with the approval of the Contractor, renew the term of this Contract up to a maximum of two (2) additional years, or other specified length options, (or at the County’s sole discretion, extend the contract on a month to month basis for a maximum of six (6) months after expiration). The Contractor shall be notified in writing by the Materials Management Department of the County’s intention to extend the contract term at least thirty (30) calendar days prior to the expiration of the original contract term. 5.3 5.4 INDEMNIFICATION: 5.3.1 To the fullest extent permitted by law, Contractor shall defend, indemnify, and hold harmless County, its agents, representatives, officers, directors, officials, and employees from and against all claims, damages, losses and expenses, including, but not limited to, attorney fees, court costs, expert witness fees, and the cost of appellate proceedings, relating to, arising out of, or alleged to have resulted from the negligent acts, errors, omissions, mistakes or malfeasance relating to the performance of this Contract. Contractor’s duty to defend, indemnify and hold harmless County, its agents, representatives, officers, directors, officials, and employees shall arise in connection with any claim, damage, loss or expense that is caused by any negligent acts, errors, omissions or mistakes in the performance of this Contract by the Contractor, as well as any person or entity for whose acts, errors, omissions, mistakes or malfeasance Contractor may be legally liable. 5.3.2 The amount and type of insurance coverage requirements set forth herein will in no way be construed as limiting the scope of the indemnity in this paragraph. 5.3.3 The scope of this indemnification does not extend to the sole negligence of County. INSURANCE REQUIREMENTS: 5.4.1 Contractor, at Contactor’s own expense, shall purchase and maintain the herein stipulated minimum insurance from a company or companies duly licensed by the State of Arizona and possessing a current A.M. Best, Inc. rating of A-, VII or higher. In lieu of State of Arizona licensing, the stipulated insurance may be purchased from a company or companies, which are authorized to do business in the State of Arizona, provided that said insurance companies meet the approval of County. The form of any insurance policies and forms must be acceptable to County. 5.4.2 All insurance required herein shall be maintained in full force and effect until all work or service required to be performed under the terms of the Contract is satisfactorily completed and formally accepted. Failure to do so may, at the sole discretion of County, constitute a material breach of this Contract. 5.4.3 Contractor’s insurance shall be primary insurance as respects County, and any insurance or self-insurance maintained by County shall not contribute to it. Page 8 of 73 SERIAL #: PH RFP 12-023 5.4.4 Any failure to comply with the claim reporting provisions of the insurance policies or any breach of an insurance policy warranty shall not affect the County’s right to coverage afforded under the insurance policies. 5.4.5 The insurance policies may provide coverage that contains deductibles or self-insured retentions. Such deductible and/or self-insured retentions shall not be applicable with respect to the coverage provided to County under such policies. Contactor shall be solely responsible for the deductible and/or self-insured retention and County, at its option, may require Contractor to secure payment of such deductibles or self-insured retentions by a surety bond or an irrevocable and unconditional letter of credit. 5.4.6 County reserves the right to request and to receive, within 10 working days, certified copies of any or all of the herein required insurance certificates. County shall not be obligated to review policies and/or endorsements or to advise Contractor of any deficiencies in such policies and endorsements, and such receipt shall not relieve Contractor from, or be deemed a waiver of County’s right to insist on strict fulfillment of Contractor’s obligations under this Contract. 5.4.7 The insurance policies required by this Contract, except Workers’ Compensation, and Errors and Omissions, shall name County, its agents, representatives, officers, directors, officials and employees as Additional Insureds. 5.4.8 The policies required hereunder, except Workers’ Compensation, and Errors and Omissions, shall contain a waiver of transfer of rights of recovery (subrogation) against County, its agents, representatives, officers, directors, officials and employees for any claims arising out of Contractor’s work or service. 5.4.9 Commercial General Liability. Commercial General Liability insurance and, if necessary, Commercial Umbrella insurance with a limit of not less than $1,000,000 for each occurrence, $2,000,000 Products/Completed Operations Aggregate, and $2,000,000 General Aggregate Limit. The policy shall include coverage for bodily injury, broad form property damage, personal injury, products and completed operations and blanket contractual coverage, and shall not contain any provision which would serve to limit third party action over claims. There shall be no endorsement or modification of the CGL limiting the scope of coverage for liability arising from explosion, collapse, or underground property damage. 5.4.10 Automobile Liability. Commercial/Business Automobile Liability insurance and, if necessary, Commercial Umbrella insurance with a combined single limit for bodily injury and property damage of not less than $1,000,000 each occurrence with respect to any of the Contractor’s owned, hired, and non-owned vehicles assigned to or used in performance of the Contractor’s work or services under this Contract. 5.4.11 Workers’ Compensation. 5.4.11.1 Workers’ Compensation insurance to cover obligations imposed by federal and state statutes having jurisdiction of Contractor’s employees engaged in the performance of the work or services under this Contract; and Employer’s Liability insurance of not less than $100,000 for each accident, $100,000 disease for each employee, and $500,000 disease policy limit. 5.4.11.2 Contractor waives all rights against County and its agents, officers, directors and employees for recovery of damages to the extent these damages are covered by the Workers’ Compensation and Employer’s Liability or commercial umbrella liability insurance obtained by Contractor pursuant to this Contract. Page 9 of 73 SERIAL #: PH RFP 12-023 5.4.12 Errors and Omissions Insurance. Errors and Omissions insurance and, if necessary, Commercial Umbrella insurance, which will insure and provide coverage for errors or omissions of the Contractor, with limits of no less than $1,000,000 for each claim. 5.4.13 Certificates of Insurance. 5.4.13.1 Prior to commencing work or services under this Contract, Contractor shall have insurance in effect as required by the Contract in the form provided by the County, issued by Contractor’s insurer(s), as evidence that policies providing the required coverage, conditions and limits required by this Contract are in full force and effect. Such certificates shall be made available to the County upon 48 hours notice. BY SIGNING THE AGREEMENT PAGE THE CONTRACTOR AGREES TO THIS REQUIREMENT AND FAILURE TO MEET THIS REQUIREMENT WILL RESULT IN CANCELLATION OF CONTRACT. 5.4.13.1.1 In the event any insurance policy (ies) required by this contract is (are) written on a “claims made” basis, coverage shall extend for two years past completion and acceptance of Contractor’s work or services and as evidenced by annual Certificates of Insurance. 5.4.13.1.2 If a policy does expire during the life of the Contract, a renewal certificate must be sent to County fifteen (15) days prior to the expiration date. 5.4.14 Cancellation and Expiration Notice. Insurance required herein shall not be permitted to expire, be canceled, or materially changed without thirty (30) days prior written notice to the County. 5.5 LICENSURE/CERTIFICATION 5.5.1 5.5.2 5.5.3 5.6 Contractor shall comply with all applicable provisions of law and other rules and regulations of any and all governmental, accrediting and/or regulatory authorities relating to the licensure and regulation of health care providers and physicians. Upon request, Contractor agrees to allow County, to the extent permitted by law, access to credentials of Qualified Physicians and Qualified Providers who are providing services to Department under the terms and conditions of this Contract. Contractor expressly agrees that it shall comply with all rules, regulations, orders, standards and interpretations promulgated pursuant to the Occupational Safety and Health Act of 1970 (and to the Occupational and Safety Health Act of the State of Arizona), including but not limited to training, provision of personal protective equipment, provision of postexposure prophylaxis, adherence to appropriate lock out/tag out procedures, and providing all notices, material safety data sheets, labels, etc. required by the right-to-know-standard. ACCESS TO AND RETENTION OF RECORDS FOR THE PURPOSE OF AUDIT AND/OR OTHER REVIEW: 5.6.1 In accordance with section MCI 367 of the Maricopa County Procurement Code the Contractor agrees to retain all books, records, accounts, statements, reports, files, and other records and back-up documentation relevant to this Contract for six (6) years after final payment or until after the resolution of any audit questions which could be more than six (6) years, whichever is latest. The County, Federal or State auditors and any other persons duly authorized by the Department shall have full access to, and the right to examine, copy, and make use of, any and all said materials. Page 10 of 73 SERIAL #: PH RFP 12-023 5.6.2 5.7 5.8 If the Contractor’s books, records , accounts, statements, reports, files, and other records and back-up documentation relevant to this Contract are not sufficient to support and document that requested services were provided, the Contractor shall reimburse Maricopa County for the services not so adequately supported and documented. SUBCONTRACTING: 5.7.1 The Contractor may not assign a Contract or Subcontract to another party for performance of the terms and conditions hereof without the written consent of the County. All correspondence authorizing subcontracting must reference the Bid Serial Number and identify the job project. 5.7.2 The Subcontractor’s rate for the job shall not exceed that of the Prime Contractor’s rate, as bid in the pricing section, unless the Prime Contractor is willing to absorb any higher rates. The Subcontractor’s invoice shall be invoiced directly to the Prime Contractor, who in turn shall pass-through the costs to the County, without mark-up. A copy of the Subcontractor’s invoice must accompany the Prime Contractor’s invoice. SCHEDULE OF EVENTS: Request for Proposals Issued: January 27, 2012 Deadline for written questions is February 13, 2012. Questions will not be responded to after the deadline has elapsed. All questions and answers shall be posted to www.bidsync.com under the Q&A’s tab for the solicitation and must be received by 2:00 PM Arizona time. Proposals Opening Date: February 24, 2012 Deadline for submission of proposals is 2:00 P.M., Arizona Time, on FEBRUARY 24, 2012. All proposals must be received before 2:00 P.M., Arizona Time, on the above date at the Maricopa County Department of Public Health, 4041 N. Central Avenue, #1400, Phoenix, AZ 85012. Proposed review of Proposals and short list decision: February 24 – March 2, 2012 Proposed selection and negotiation: March 2 – March 9, 2012 Proposed Best & Final (if required) March 9 – March 16, 2012 Proposed award of Contract: April 11, 2012 All responses to this Request for Proposal become the property of Maricopa County and (other than pricing) will be held confidential, to the extent permissible by law. The County will not be held accountable if material from proposal responses is obtained without the written consent of the Respondent by parties other than the County. 5.9 INQUIRIES AND NOTICES: All inquiries concerning information herein shall be addressed to: Maricopa County Department of Public Health Attn: Cheryl Rentscheler 4041 N. Central Avenue, #1400 Phoenix, AZ 85012 Administrative telephone inquiries shall be addressed to: Cheryl Rentscheler, Procurement Officer, 602.506.6886 Page 11 of 73 SERIAL #: PH RFP 12-023 (cherylrentscheler@mail.maricopa.gov) Inquiries may be submitted by telephone but must be followed up in writing. communication is binding on Maricopa County. 5.10 No oral INSTRUCTIONS FOR PREPARING AND SUBMITTING PROPOSALS: Respondents shall provide their proposals in accordance with Section 5.13 as follows: 5.10.1 One (1) original hardcopy of all proposal documents. 5.10.2 One (1) CD or flash drive providing all proposal documents in their original version (Word, Excel, etc.) as well as all proposal documents in PDF format. 5.10.3 Five (5) CD’s or flash drives providing the entire proposal in PDF format only. 5.10.4 Respondents shall address proposals identified with return address, serial number and title in the following manner: Maricopa County Department of Public Health Attn: Cheryl Rentscheler 4041 N. Central Avenue, #1400 Phoenix, AZ 85012 SERIAL #: PH RFP 12-023, BREAST AND CERVICAL CANCER EARLY DETECTION SCREENING, DIAGNOSTIC, & TREATMENT SERVICES 5.10.5 5.11 Proposals shall be signed by an owner, partner or corporate official who has been authorized to make such commitments. All prices shall be held firm for a period of one hundred fifty (150) days after the RFP closing date. EXCEPTIONS TO THE SOLICITATION: The Respondent shall identify and list all exceptions taken to all sections of PH RFP 12-023 and list these exceptions referencing the section (paragraph) where the exception exists and identify the exceptions and the proposed wording for the Respondent’s exception under the heading, “Exception to the PROPOSAL Solicitation, SERIAL #: PH RFP 12-023.” Exceptions that surface elsewhere and that do not also appear under the heading, “Exceptions to the PROPOSAL Solicitation, SERIAL #: PH RFP 12-023,” shall be considered invalid and void and of no contractual significance. The County reserves the right to reject, determine the proposal non-responsive, enter into negotiation on any of the Respondent exceptions, or accept them outright. 5.12 5.13 GENERAL CONTENT: 5.12.1 The Proposal should be specific and complete in every detail. It should be practical and provide a straightforward, concise delineation of capabilities to satisfactorily perform the Contract being sought. 5.12.2 The Respondent should not necessarily limit the proposal to the performance of the services in accordance with this Request for Proposal but should outline any additional services and their costs if the Respondent deems them necessary to accomplish the program. FORMAT AND CONTENT: Page 12 of 73 SERIAL #: PH RFP 12-023 To aid in the evaluation, it is desired that all proposals follow the same general format. The proposal hardcopy must be submitted in binders and have sections tabbed as below: (Responses are limited to 20 pages, single sided, 10 point font type). 5.14 5.13.1 Table of Contents 5.13.2 Letter of Transmittal 5.13.3 Qualifications and Experience – This section shall describe the respondent’s ability and experience related to the programs and services proposed. All project personnel, as applicable, shall be listed including a description of assignments and responsibilities, a resume of professional experience, an estimate of the time each would devote to this program, and other pertinent information. Copies of licenses, accreditation certification, evidence of status as an AHCCCS registered provider, and other pertinent documents shall also be included. Include prior history or capability of providing breast and cervical cancer screening, and diagnostic services, especially those provider institutions with established women’s health and outreach programs. 5.13.4 Services to Be Provided - This section should contain a statement of all of the services proposed, Identify the breast and cervical cancer screening services you intend to provide as well as which diagnostic services you intend to provide. If you will be contracting diagnostic services through another provider, identify the provider and the services they will provide. Specify the number of women for annual and diagnostic services your organization is able and willing to handle on a weekly/annual basis. If applicable, also identify the treatment services that you have the capacity to provide. If you do not have the capacity to provide treatment services, please identify the provider or agency to whom you will refer women for treatment. 5.13.5 Approach – This section shall contain an outline of the general approach you shall utilize. Fully explain your established ability or plan to reach the target population of whom 75% are 50 years of age or older. Include detailed plans for tracking and retaining enrollees over a 12-month period so as to have them return for an annual exam to include all the above mentioned services. Describe strategies for scheduling client appointments in a timely manner. Explain plan for providing test results to WWHP case managers in a timely manner. Describe process for ensuring timely follow-up of women with abnormal results to ensure that CDC timeframe requirements for screening to diagnosis and diagnosis to treatment are met. Describe plan for submitting completed program forms, and results within 30 days after screening and diagnostic procedures/exams. 5.13.6 Proposal exceptions 5.13.7 Attachment A (Pricing) 5.13.8 Attachment B (Agreement Page) 5.13.9 Attachment C (References) EVALUATION OF PROPOSAL – SELECTION FACTORS: A Proposal Evaluation Committee shall be appointed, chaired by the Procurement Officer to evaluate each Proposal. At the County’s option, Respondents may be invited to make presentations to the Evaluation Committee. Best and Final Offers and/or Negotiations may be conducted, as needed, with the highest rated Respondent(s). Proposals will be evaluated on the following criteria which are listed descending order of importance: 5.14.1 5.14.2 Qualifications and Experience Approach Page 13 of 73 SERIAL #: PH RFP 12-023 5.14.3 Services to be provided – preference will be given to providers in the following zip codes: 85021, 85032, 85050, 85254, 85260, 85331, 85335, 85370, 85374, 85379 and surrounding areas. Preference will also be given to providers who are able to perform treatment services or have a well-established network for treatment referrals. 5.15 CERTIFICATION REGARDING DEBARMENT AND SUSPENSION: 5.15.1 The undersigned (authorized official signing for the Contractor) certifies to the best of his or her knowledge and belief, that the Contractor, defined as the primary participant in accordance with 45 CFR Part 76, and its principals: 5.15.1.1 are not presently debarred, suspended, proposed for debarment, declared ineligible, or voluntarily excluded from covered transactions by any Federal Department or agency; 5.15.1.2 have not within 3-year period preceding this Contract been convicted of or had a civil judgment rendered against them for commission of fraud or a criminal offense in connection with obtaining, attempting to obtain, or performing a public (Federal, State or local) transaction or contract under a public transaction; violation of Federal or State antitrust statues or commission of embezzlement, theft, forgery, bribery, falsification or destruction of records, making false statements, or receiving stolen property; 5.15.1.3 are not presently indicted or otherwise criminally or civilly charged by a government entity (Federal, State or local) with commission of any of the offenses enumerated in paragraph (2) of this certification; and 5.15.1.4 have not within a 3-year period preceding this Contract had one or more public transaction (Federal, State or local) terminated for cause of default. 5.15.2 Should the Contractor not be able to provide this certification, an explanation as to why should be attached to the Contact. 5.15.3 The Contractor agrees to include, without modification, this clause in all lower tier covered transactions (i.e. transactions with subcontractors) and in all solicitations for lower tier covered transactions related to this Contract. 5.16 VERIFICATION REGARDING COMPLIANCE WITH ARIZONA REVISED STATUTES §414401 AND FEDERAL IMMIGRATION LAWS AND REGULATIONS: 5.16.1 By entering into the Contract, the Contractor warrants compliance with the Immigration and Nationality Act (INA using e-verify) and all other federal immigration laws and regulations related to the immigration status of its employees and A.R.S. §23-214(A). The contractor shall obtain statements from its subcontractors certifying compliance and shall furnish the statements to the Procurement Officer upon request. These warranties shall remain in effect through the term of the Contract. The Contractor and its subcontractors shall also maintain Employment Eligibility Verification forms (I-9) as required by the Immigration Reform and Control Act of 1986, as amended from time to time, for all employees performing work under the Contract and verify employee compliance using the E-verify system and shall keep a record of the verification for the duration of the employee’s employment or at least three years, whichever is longer. I-9 forms are available for download at USCIS.GOV. 5.16.2 The County retains the legal right to inspect contractor and subcontractor employee documents performing work under this Contract to verify compliance with paragraph 5.16.1 of this Section. Contractor and subcontractor shall be given reasonable notice of the County’s intent to inspect and shall make the documents available at the time and date specified. Should the County suspect or find that the Contractor or any of its subcontractors are not in compliance, the County will consider this a material breach of the contract and may pursue any and all remedies allowed by law, including, but not limited to: suspension of work, termination of the Contract for default, and suspension and/or debarment of the Contractor. All costs necessary to verify compliance are the responsibility of the Contractor. 5.17 VERIFICATION REGARDING COMPLIANCE WITH ARIZONA REVISED STATUTES §§35-391.06 AND 35-393.06 BUSINESS RELATIONS WITH SUDAN AND IRAN: Page 14 of 73 SERIAL #: PH RFP 12-023 5.17.1 5.17.2 By entering into the Contract, the Contractor certifies it does not have scrutinized business operations in Sudan or Iran. The contractor shall obtain statements from its subcontractors certifying compliance and shall furnish the statements to the Procurement Officer upon request. These warranties shall remain in effect through the term of the Contract. The County may request verification of compliance for any contractor or subcontractor performing work under the Contract. Should the County suspect or find that the Contractor or any of its subcontractors are not in compliance, the County may pursue any and all remedies allowed by law, including, but not limited to: suspension of work, termination of the Contract for default, and suspension and/or debarment of the Contractor. All costs necessary to verify compliance are the responsibility of the Contractor. 5.18 CONTRACTOR LICENSE REQUIREMENT: 5.18.1 The Respondent shall procure all permits, insurance, licenses and pay the charges and fees necessary and incidental to the lawful conduct of his/her business, and as necessary complete any required certification requirements, required by any and all governmental or non-governmental entities as mandated to maintain compliance with and in good standing for all permits and/or licenses. The Respondent shall keep fully informed of existing and future trade or industry requirements, Federal, State and Local laws, ordinances, and regulations which in any manner affect the fulfillment of a Contract and shall comply with the same. Contractor shall immediately notify both Materials Management and the using agency of any and all changes concerning permits, insurance or licenses. 5.18.2 Respondents furnishing finished products, materials or articles of merchandise that will require installation or attachment as part of the Contract, shall possess any licenses required. A Respondent is not relieved of its obligation to posses the required licenses by subcontracting of the labor portion of the Contract. Respondents are advised to contact the Arizona Registrar of Contractors, Chief of Licensing, at (602) 542-1502 to ascertain licensing requirements for a particular contract. Respondents shall identify which license(s), if any, the Registrar of Contractors requires for performance of the Contract. 5.19 INFLUENCE: As prescribed in MC1-1202 of the Maricopa County Procurement Code, any effort to influence an employee or agent to breach the Maricopa County Ethical Code of Conduct or any ethical conduct, may be grounds for Disbarment or Suspension under MC1-902. An attempt to influence includes, but is not limited to: 5.19.1 5.19.2 A Person offering or providing a gratuity, gift, tip, present, donation, money, entertainment or educational passes or tickets, or any type valuable contribution or subsidy, That is offered or given with the intent to influence a decision, obtain a contract, garner favorable treatment, or gain favorable consideration of any kind. If a Person attempts to influence any employee or agent of Maricopa County, the Chief Procurement Officer, or his designee, reserves the right to seek any remedy provided by the Maricopa County Procurement Code, any remedy in equity or in the law, or any remedy provided by this contract. 5.20 POST AWARD MEETING: The successful Respondent(s) may be required to attend a post-award meeting with the Using Agency to discuss the terms and conditions of the Contract. This meeting will be coordinated by the Procurement Officer of the Contract. NOTE 1: RESPONDENTS ARE STRONGLY ENCOURAGED TO REVIEW MARICOPA COUNTY’S PROCUREMENT ADMINISTRATIVE INFORMATION AND SAMPLE CONTRACT DOCUMENT PRIOR TO SUBMITTING A PROPOSAL. FOR THIS INFORMATION, GO TO: http://www.maricopa.gov/Materials Page 15 of 73 SERIAL #: PH RFP 12-023 NOTE 2: RESPONDENTS ARE REQUIRED TO USE ATTACHED FORMS TO SUBMIT THEIR PROPOSAL. Page 16 of 73 SERIAL #: PH RFP 12-023 ATTACHMENT A PRICING SHEET BIDDER NAME: F.I.D./VENDOR #: BIDDER ADDRESS: P.O. ADDRESS: BIDDER PHONE #: BIDDER FAX #: COMPANY WEB SITE: COMPANY CONTACT (REP): E-MAIL ADDRESS (REP): PAYMENT TERMS: BIDDER IS REQUIRED TO SELECT ONE OF THE FOLLOWING: TERMS WILL BE CONSIDERED IN DETERMINING LOW BID. FAILURE TO CHOOSE A TERM WILL RESULT IN A DEFAULT TO NET 30. BIDDER MUST INITIAL THE SELECTION BELOW. NET 10 ____________________ NET 15 ____________________ NET 20 ____________________ NET 30 ____________________ NET 45 ____________________ NET 60 ____________________ NET 90 ____________________ 2% 10 DAYS NET 30 ____________________ 1% 10 DAYS NET 30 ____________________ 2% 30 DAYS NET 31 ____________________ 1% 30 DAYS NET 31 ____________________ 5% 30 DAYS NET 31 ____________________ COMPENSATION/FEES: Procedures as described in Section 4.2 (As defined herein) RATE As determined by Medicare’s allowable costs (Exhibit 4) Respondent's signature below indicates understanding and agreement to perform the services outlined in the Request for Proposal indicated above for the total amounts listed above. Signature (REQUIRED) Date Page 17 of 73 SERIAL #: PH RFP 12-023 ATTACHMENT B AGREEMENT Respondent hereby certifies that Respondent has read, understands, and agrees that acceptance by Maricopa County of the Respondent’s Offer will create a binding Contract. Respondent agrees to fully comply with all terms and conditions as set forth in the Maricopa County Procurement Code, and amendments thereto, together with the specifications and other documentary forms herewith made a part of this specific procurement. BY SIGNING THIS PAGE THE SUBMITTING RESPONDENT CERTIFIES THAT RESPONDENT HAS REVIEWED THE ADMINISTRATIVE INFORMATION AND DRAFT RFP CONTRACT’S TERMS AND CONDITIONS LOCATED AT http://www.maricopa.gov/materials. AND AGREE TO BE CONTRACTUALLY BOUND TO THEM. [] Small Business Enterprise (SBE) RESPONDENT (FIRM) SUBMITTING PROPOSAL FEDERAL TAX ID NUMBER PRINTED NAME AND TITLE AUTHORIZED SIGNATURE ADDRESS TELEPHONE DUNS # / CITY WEB SITE STATE ZIP FAX # DATE EMAIL ADDRESS Page 18 of 73 SERIAL #: PH RFP 12-023 ATTACHMENT C RESPONDENT’S REFERENCES RESPONDENT SUBMITTING PROPOSAL: 1. COMPANY NAME: ADDRESS: CONTACT PERSON: TELEPHONE: 2. E-MAIL ADDRESS: COMPANY NAME: ADDRESS: CONTACT PERSON: TELEPHONE: 3. E-MAIL ADDRESS: COMPANY NAME: ADDRESS: CONTACT PERSON: TELEPHONE: 4. E-MAIL ADDRESS: COMPANY NAME: ADDRESS: CONTACT PERSON: TELEPHONE: 5. E-MAIL ADDRESS: COMPANY NAME: ADDRESS: CONTACT PERSON: TELEPHONE: E-MAIL ADDRESS: Page 19 of 73 EXHIBIT 1 VENDOR REGISTRATION PROCEDURES BidSync.com Registration is FREE and REQUIRED for all vendors. Register On-line at https://www.bidsync.com/Links/links-learn Upon completion of your on-line registration, you are responsible for updating any changes to your information. Please retain your Login ID and Password for future use. For assistance, please contact BidSync Vendor Support Department via phone or email, during regular business hours: 1800-990-9339 or agencysupport@BidSync.com Page 20 of 73 SERIAL #: PH RFP 12-023 EXHIBIT 2 SAMPLE TRANSMITTAL LETTER (To be typed on the letterhead of Offeror) Maricopa County Department of Public Health 4041 N. Central Avenue, #1400 Phoenix, AZ 85012 Re: Serial #: PH RFP 12-023, BREAST AND CERVICAL CANCER EARLY DETECTION SCREENING, DIAGNOSTIC, & TREATMENT SERVICES To Cheryl Rentscheler: (NAME OF COMPANY) (Herein referred to as the "RESPONDENT"), hereby submits its response to your Request for Proposal dated , and agrees to perform as proposed in their proposal, if awarded the contract. The Respondent shall thereupon be contractually obligated to carry out its responsibilities respecting the services proposed. Kindly advise us in writing on or before if you should desire to accept this proposal. Very truly yours, _______________________________ NAME (please print) _______________________________ SIGNATURE _______________________________ TITLE (please print) Page 21 of 73 SERIAL #: PH RFP 12-023 EXHIBIT 3 Breast & Cervical Clinical Guidelines Page 22 of 73 SERIAL #: PH RFP 12-023 The Well Woman Healthcheck Program wishes to extend its gratitude and appreciation to the past and current Well Woman Healthcheck Medical Advisory Board members for their work on the initial version, revision and expansion of this guide. Notes about the Well Woman Healthcheck Breast and Cervical Clinical Guidelines This symbol precedes Well Woman Healthcheck policy, which may not necessarily be representative of standard breast and cervical screening guidelines for the general population. Page 23 of 73 SECTION ONE - BREAST HEALTH Screening is the process to assist in the detection of unsuspected disease in asymptomatic patients. Seventy-five percent of women with newly diagnosed breast cancer have no identifiable risk. The methods used for early detection of breast cancer by health providers are clinical breast examination (CBE) and routine screening mammography. The purpose of mammography screening is to improve breast cancer survival rates by detecting breast cancer before it is palpable. Screening mammography combined with CBE has been found to significantly decrease breast cancer mortality for women 50 years of age and older. The American Cancer Society and the National Cancer Institute recommend screening mammography every year for women 40 years of age and older. Controversy still exists within the medical community concerning the frequency of mammography examination and the ages for which to start and stop routine mammography screening. Women younger than 40 years of age should have an annual clinical breast examination, but they should not undergo routine screening mammography, unless of course they have risk factors for early-onset breast carcinoma and/or are symptomatic. Symptoms suggestive of breast cancer include: Painless lump or mass Spontaneous, unilateral, serous or serosanguinous nipple discharge Spontaneous, unilateral, bloody nipple discharge Dermatitis of nipple/areola Change in contour of breast Dimpling of the breast skin Nipple retraction (this does not include women with a history of inverted nipples) Fixation of a mass to the chest wall or adjacent tissue Edema and erythema of breast skin Axillary adenopathy Important points to remember about breast cancer screening: Normal results on a screening examination do not necessarily indicate absence of disease. No screening test is 100% accurate; therefore, some cases of the disease may be unavoidably missed. Normal results of a screening exam should never rule out the later development of disease, which is why ongoing regular screening is so strongly recommended. The detection of an abnormality does not mean the abnormality is cancerous. Only about 20 percent of the women with abnormal screening results will, after further evaluation, be diagnosed with breast cancer. PATIENT EDUCATION Written materials regarding clinical breast examination (CBE), breast-self examination (BSE) and mammography should be provided to the patient to reinforce staff recommendations. Materials should include information in regard to: BSE techniques and normal findings; indications for calling provider about signs or symptoms of breast cancer; importance of age-appropriate screening; an explanation of breast screening and diagnostic procedures; and the limitations of screening exams. Page 24 of 73 Instruct clients on the day of their mammography appointment to: Wear pants or a skirt because she will have to undress from the waist up. Instruct her to avoid the use of deodorants, powders or other topical agents on the breasts or in the underarm areas, because they may cause artifacts on the mammogram. Breast-self Examination (BSE) The benefit of breast-self examination (BSE) in the early detection of breast cancer has not been proven. Breast-self examination should be taught to patients but not overemphasized. If a patient values the role of breast self examination in breast cancer screening and is comfortable with its use, the practice should be reinforced and encouraged. A woman who finds a mass or abnormality during BSE should be seen promptly for appropriate clinical evaluation. RISK ASSESSMENT AND CLINICAL BREAST EXAMINATION (CBE) A comprehensive breast examination includes: risk assessment, patient history, and a thorough examination. Risk assessment: age; family history of breast cancer (mother, sisters, daughters) including the age they developed breast cancer, bilateral or unilateral involvement; family men who had breast cancer; and family who had ovarian cancer. Specific history: previous biopsies and the pathology discovered; diagnosis of previous breast, endometrial, ovarian, or colon cancer; parity, age at first child; age at menarche and menopause; hormone or contraceptive use; the possibility of current pregnancy; and potential radiation exposure as a child. Symptom assessment: lumps, pain, nipple discharge, changes in shape, difference between breasts, cyclic tenderness, and skin changes. The CBE should occur prior to the patient's mammography appointment to determine the need for routine screening or diagnostic imaging. Clinical Breast Examination: The examination should be conducted in a setting allowing for minimal distraction and adequate patient privacy. Examination gowns should be adjusted to minimize the unnecessary exposure of the patient being examined. A complete clinical breast examination should take 5-10 minutes. The CBE should occur: A.) With the Patient Sitting: Inspect the breasts for asymmetry, abnormal superficial vascular patterns, dimpling, nipple retraction, and peau d'orange. Palpation of axillary and supraclavicular/infraclavicular nodes. Note size, location mobility, and consistency of nodes palpated. Page 25 of 73 Page 26 of 73 A discrete palpable mass should be documented in the examiners notes with specific notation of the following elements: Location (upper outer quadrant; 1 cm. from the nipple) Mobility (fixed, mobile) Approximate size (1/2 cm. 1 cm.) Consistency and tenderness (lump, rubbery, soft, smooth) Bloody or serous nipple discharge Nipple or areolar scaliness Skin dimpling and retraction (puckering, dimpling, thickening) MAMMOGRAPHY Screening Mammography - (CPT Code 76092) Is a bilateral procedure performed to detect unsuspected cancer in asymptomatic women, it is limited to two images, craniocaudal and mediolateral oblique views. Diagnostic Mammography: Unilateral- (CPT Code 76090) May also be referred to as "additional" or "supplementary" mammographic views, such as magnification for calcification and/or a coned compression view. A diagnostic mammogram requires direct physician supervision and interpretive skills. It is used to further investigate suspicious masses found on physical examination. A unilateral exam is limited to the symptomatic breast. Diagnostic Mammography; Bilateral- (CPT Code 76091) May also be referred to as "additional" or "supplementary" mammographic views, such as magnification for calcification and/or a coned compression view. A diagnostic mammogram requires direct physician supervision and interpretive skills. It is used to further investigate suspicious masses found on physical examination. A bilateral exam focuses on both breasts. Seventy-five percent of the women receiving mammography services in the Well Woman Healthcheck Program must be 50 years of age and older. Twenty-five percent of the women receiving mammography services through the Well Woman Healthcheck Program may be younger women. All Well Woman Healthcheck Program patients must have a CBE within six-weeks prior to their scheduled screening mammography appointment. A routine screening mammography consists of mediolateral oblique and craniocaudal projections of both breasts. Any women with a positive clinical breast examination should be referred for a diagnostic mammogram. The CBE results should be well documented and forwarded to the referral mammography facility. Scheduling mammography services during a patient's menstrual cycle should be avoided due to increased breast tenderness. Women with breast implants should be referred to a radiologist with experience in performing mammography on these women. If the client has had a previous mammogram, request that her films be sent from last mammogram to the referral mammography facility. Page 27 of 73 Mammography Facilities Effective October 1, 1994, all mammography facilities must be certified by the Food and Drug Administration (FDA) as providing quality mammography. Certification requirements included in the Mammography Quality Standards Act (MQSA) discuss personnel, equipment, radiation exposure, quality assurance programs, and record keeping and reporting issues. A list of certified mammography facilities can be obtained online from: www.fda.gov/cdrh/mammography/certified.html WWHP MAMMOGRAPHY SCREENING GUIDELINES I. Women less than 40 Years of Age Women less than 40 years of age must have a clinical breast examination to confirm symptoms prior to receiving breast follow-up services through the Well Woman Healthcheck Program. If the CBE confirms suspicious findings then: Women 35 years of age or older may be referred for diagnostic mammography; Women less than 35 years of age should not be referred for mammography, as results often are equivocal. Women less than 35 years of age should be referred for breast ultrasound examination. II. Women 40-49 Years of Age Since women less than 50 years of age may only account for 25% of the yearly mammograms performed, the clinician must evaluate the client's risk to determine the patient's future screening interval: Low risk group -discuss need for every other year (biennial) mammographic screening High-risk group - may benefit from yearly mammographic screening. This group includes those women with: Personal history of breast cancer. (Approximately 10% will have a second primary breast cancer during her lifetime) Family history of breast cancer, first-degree relative with premenopausal breast cancer. (Risk increased 3-4 times.) Mother, daughter, or sister with a history of premenopausal bilateral breast cancer. (Risk increased 8-10 times.) Biopsy-proven moderate or severe atypical epithelial hyperplasia. (Risk increased 3-5 times.) Personal history of lobular ductal carcinoma-in-situ. (Risk increased 8-10 times.) Nulliparity or age 30 or older at first live birth. (Risk increased 1-1.5 times.) III. Women 50 Years of Age and Older Annual CBE and bilateral screening mammography Page 28 of 73 Well Woman Healthcheck Program's Mammography Screening Policy Matrix 75% of WWHP mammograms must be provided to women 50 years of age or older. 25% of WWHP mammograms may be provide to women less than 50 years of age. Age CBE Mammography Under 40 Annual CBE 50+ Annual CBE Women under 40 years of age may be eligible for breast screening and diagnostics if an abnormality is confirmed by clinical breast exam. Due to breast density, mammography is of little value in this population of women. Women less than 35 years of age should be directly referred for an ultrasound examination of the breast(s). Annual bilateral mammography screening. Page 29 of 73 Mammography Reporting Lexicon The American College of Radiologists, BI-RADSTM (Breast Imaging Reporting and Data System) reporting system is the required mammography-reporting lexicon under the MQSA regulations. The mammography report should be concise and include: (1) a succinct description of the overall breast composition; (2) a clear description of any significant finding [a] mass [b] calcifications [c] architectural distortion and [d] special cases; and (3) an overall summary impression as follows: BI-RADSTM Category 0 Assessment Incomplete Category 1 Negative Category 2 Benign Finding for which additional imaging evaluation is needed. A recommendation for additional imaging evaluation includes the use of spot compression, magnifications, special mammographic views, ultrasounds, etc. Negative mammogram There is a negative mammogram but the interpreter may wish to describe the finding. Involuting, calcified fibroadenomas, fat containing lesions, such as oil cysts, lipomas, etc., all have characteristic appearances and may be labeled. A finding in this category should have high probability of being benign. It is not expected to change over the followup interval but the radiologist would prefer to establish stability Biopsy should be considered. These Category 4 Suspicious Abnormality are lesions that do not have characteristic morphologies of breast cancer but have a definite probability of being malignant. The radiologist has sufficient concern to urge a biopsy. If possible, the relevant probabilities should be cited so that the patient and her physician can make the decision on the ultimate course of action. Appropriate action should be taken, Category 5 Highly Suggestive of Malignancy these lesions have a high probability of being cancer. TM For more information in regard to BI-RADS please visit the American College of Radiologists’ web site at: www.acr.org Category 3 Probably Benign FOLLOW-UP ROUTINE For normal Screening Examination (both CBE and Mammogram) Page 30 of 73 Normal CBE = a finding of "normal" or "benign" Normal Mammogram = a BI-RADTM 1 or BI-RADTM 2 mammography finding. Notify the patient of examination findings, including the need for regular ongoing screening examinations and the procedure for reminding the patient when her next screening examination is due. For Abnormal Screening Examination (either CBE or Mammogram) An abnormal clinical breast examination or screening mammogram should generate follow-up diagnostic referrals. Notify the patient of an abnormal result and the implications within 5 days of receipt of abnormal findings, include: need for further testing, a choice (if available) of appropriate referrals for definitive diagnostic procedures, and an explanation that it is her responsibility to obtain follow-up care in a timely manner before the need for treatment can be established. Abnormal CBE An abnormal CBE should be followed by a diagnostic mammogram. If the diagnostic mammogram is negative, a referral to a surgeon or physician with expertise in breast problems is required. A normal mammogram does not rule out cancer if a woman has a mass on CBE. Abnormal Mammogram An abnormal screening mammogram should be followed with additional mammographic views or ultrasound as recommended by the radiologist. Page 31 of 73 MANAGEMENT OF COMMON BREAST PROBLEMS Prepared by the Commission on Cancer and the American College of Surgeons and the Society of Surgical Oncology for the Centers for Disease Control and Prevention (1995). Thorough communication with patients about the follow-up options, their risks, and all test results, as well as written documentation of these discussions, is very important to the provision of quality care. Cyst Solid Ultrasound or cyst aspiration is useful to differentiate between solid and cystic mass. If the mass does not disappear with fine needle aspiration, or if the fluid is bloody, send the fluid specimen for cytological study and refer the patient to a surgeon. Fluid can otherwise be discarded. Nonpalpable simple cysts confirmed by ultrasound do not need aspiration except for pain relief. Cysts having suspicious characteristics need to be biopsied. Reexamine breast in 6 weeks for recurrence. If cyst recurs, refer to a surgeon. Otherwise, follow routinely. A patient with a suspicious mass should have a bilateral diagnostic mammogram to screen both breasts for nonpalpable cancers. A normal mammogram does not eliminate need for further evaluation of a clinically suspicious mass. However, if a mass is clinically benign on breast examination, and this is confirmed by cytologic examination and mammography, the patient may be followed by a surgeon every 3 months until biopsy or resolution of problem. Women younger than 30 years most likely have cyst or fibroadenoma. Ultrasound or fine needle aspiration may be used to confirm. Refer patients to a surgeon for a solid, dominant, persistent mass because biopsy is almost always indicated. If mass persists after 3 months and can be distinguished from remainder of breast tissue, refer to a surgeon. Vague Nodularitv If significant doubt exists about the nature of a mass, consider mammogram or ultrasound first and then fine needle aspiration for cytologic examination. If mass appears benign, slightly lobulated breast tissue, or poorly defined thickening not matched in opposite breast - recheck bimonthly or quarterly. Mammographic Abnormality For American College of Radiology (ACR) BI-RADTM categories 4 (suspicious abnormality; biopsy should be considered) and BI-RADTM category 5 (highly suggestive of malignancy), refer to a surgeon. For ACR BI-RADTM category 3 (probably benign; short follow-up interval suggested), patient may be followed with sequential imaging at an interval suggested by the radiologist. Clearly communicate to women the need for clinical and imaging follow-up. Page 32 of 73 For ACR BI-RADTM category 0 (assessment is incomplete; additional imaging evaluation needed), obtain recommended imaging studies to better characterize the abnormality. Breast Pain Perform clinical breast examination and mammography, if age appropriate. If examination and mammography are negative, fibrocystic change is most likely. Reassure patient, offer a trial of a non-narcotic analgesic, and recommend use of a well-supporting brassiere. If conservative measures do not relieve pain symptoms, referral to a surgeon is indicated. Skin/Nipple Change and Nipple Discharge Women with skin breakdown on the nipple or areola should be referred to a surgeon. Patient with palpable mass and nipple discharge should be referred to a surgeon If discharge suggestive of neoplasm (spontaneous; unilateral; confined to single duct; occurring in older patient; clear, bloody, serous, or serosanguinous) send patient for mammography and surgical consult. Nipple discharge -particularly if bilateral or multiductal; milky, green, gray, or black discharge is not suggestive of cancer. If milky discharge is profuse, medical work-up for galactorrhea may be indicated. The Worried Patient with a Negative Work-up Refer patient to a surgeon for a second opinion. Difficult Breast Examinations May refer to a surgeon if the woman has had mammoplasty or augmentation implantation, if breasts are very large or multinodular, or if several biopsies have severely scarred the breasts. High-Risk Patients Consult a breast cancer specialist for a woman with history of breast cancer; strong first-degree family history; history of atypia; or multiple biopsies Such women may need special follow-up regimens. SPECIAL CONSIDERATIONS Pregnant or Lactating Women with Breast Masses Physical diagnosis of breast cancer may be extremely difficult in these situations, it is important to refer these patients to a surgeon. Approximately 1 in 2,000 pregnant or lactating women have breast cancer. Page 33 of 73 BENIGN BREAST CONDITIONS Fibrocystic disease - Characterized by nodules or cysts in ducts, may be bilateral or unilateral. May be localized or spread throughout. The patient often presents with pain and tenderness. Varies with monthly hormonal cycle. Fibroadenoma - Characterized as a firm, round, mobile, non-tender mass. Intraductal Papilloma - Overgrowth of benign cells lining the ducts. Frequently there is an absence of a palpable mass. The patient may present with serous, serosanguinous or bloody nipple discharge. Page 34 of 73 SERIAL #: PH RFP 12-023 Page 35 of 73 SERIAL #: PH RFP 12-023 Page 36 of 73 SERIAL #: PH RFP 12-023 BREAST ALGORITHMS Algorithm 1. Assessment of Risk Algorithm 2. New Palpable Mass Algorithm 3. Abnormal Screening mammogram with Normal CBE Algorithm 4. Spontaneous Unilateral Nipple Discharge Algorithm 5. Breast Skin Changes/Nipple Retraction Algorithm 6. Breast Pain in Non-Lactating Women Algorithm 7. Management of Breast Biopsy Results Page 37 of 73 SERIAL #: PH RFP 12-023 Page 38 of 73 SERIAL #: PH RFP 12-023 Page 39 of 73 SERIAL #: PH RFP 12-023 Page 40 of 73 SERIAL #: PH RFP 12-023 Page 41 of 73 SERIAL #: PH RFP 12-023 Page 42 of 73 SERIAL #: PH RFP 12-023 Page 43 of 73 SERIAL #: PH RFP 12-023 Page 44 of 73 SERIAL #: PH RFP 12-023 Page 45 of 73 SERIAL #: PH RFP 12-023 Page 46 of 73 SERIAL #: PH RFP 12-023 BREAST REFERENCES American Cancer Society. Clinical Breast Examination, Proficiency Criteria and Guidelines, pp. 1-20, 1998. American College of Radiology. Breast Imaging Lexicon, Reporting System. Available online at: http://home.earthlink.net/~rowberg/birads/reporting.htm Accessed 03/02/2000 California Department of Public Health, cancer Detection Section. Breast Cancer Diagnostic Algorithms for Primary Care Providers. June, 2011. Available online at: http://qap.sdsu.edu. Centers for Disease Control and Prevention. Evaluation of Common Breast Problems: A Primer for Primary Care Providers. Pamphlet, pp. 1-13, 1995. Centers for Disease Control and Prevention. Follow-up of Abnormal CBE and Mammographic Findings, Manual. 1999. Page 47 of 73 SERIAL #: PH RFP 12-023 SECTION TWO - CERVICAL CANCER SCREENING A cervical Pap test is a cytodiagnostic test primarily for the detection of cervical cancer and precancerous lesions. Squamous cell carcinoma comprises 90%, and adenocarcinoma comprises approximately 10% of cervical cancers (NCI, 2002). Although the Pap test can sometimes detect endometrial, vaginal and other cancers, its use as a screening test is intended for the early detection of cervical dysplasia and cancer (USPHTF, 1996). It should be noted that a single negative cytodiagnosis, and on occasion multiple negative cytodiagnoses, does not rule out gynecologic neoplasia. The Pap test false negative rate can be as high as 50% in cases of invasive cervical cancer (NCI, 2002). The early diagnosis and treatment of cervical cancer precursors or cervical carcinoma- in-situ (CIS) may delay or prevent the progression of invasive disease. Treatment at the localized stage may include any of the following clinical procedures: loop electrosurgical excision (LEEP), conization (cold knife cone biopsy), cryosurgery, laser surgery, and when necessary hysterectomy. Longitudinal studies have shown that in untreated patients with in situ cancer, 30-70% will develop invasive carcinoma over a period of 10 -12 years. However, in about 10% of patients, lesions can progress from in situ to invasive in a period of less than one year (NCI, 2002). Cervical cancer accounts for 6% of all malignancies in women Annually, there are an estimated 16,000 cases of invasive cancer of the cervix and 5,000 deaths in the United States. 40-50% of the women who will die from invasive cervical cancer are over age 65. 90% of these cases can, and should be detected early through the use of Pap test. Source: The National Cancer Institute, 2002 Symptoms Women with cervical cancer precursor lesions or CIS are often asymptomatic. Symptoms of late stage disease may include light bleeding or spotting, separate from a woman's menstrual cycle, painful intercourse, or postcoital bleeding. PATIENT EDUCATION Women should be instructed to ... Schedule an appointment approximately two weeks (10-18 days) after the first day of her last menstrual period. Not douche 48 hours prior to the test. Not use tampons, birth control foams, jellies or other vaginal creams or vaginal medications for 48 hours prior to the test. Refrain from intercourse 48 hours prior to the test. Source: American Society of Cytopathology RISK ASSESSMENT Women with an increased risk for cervical cancer include: Women who initiated sexual intercourse prior to age 16; Women with five or more sex partners in a lifetime; Women with a history of Human Immunodeficiency Syndrome (HIV); Human Papilloma Virus (HPV) or other sexually transmitted diseases; Page 48 of 73 SERIAL #: PH RFP 12-023 Women exposed to cigarette smoke; Women with prenatal exposure to diethylstilbestrol (DES)- maternal use of DES to prevent miscarriage, used from 1940 -1970; Women who have not had a Pap test within the previous five years; and Women with a history of cervical cancer or dysplasia. The Human Papillomaviruses (HPV) Research suggests that the most important risk factor for the development of cervical cancer is the presence of the human Papilloma viruses (HPV). There are over 80 distinct types of HPV identified, approximately 30 of which infect the human genital tract. HPV types 16 and 18 are most often associated with invasive disease (NCI, 2002). As HPV is sexually transmitted, barrier methods of contraception have been shown to lower the incidence of cervical neoplasia (NCI, 2002). Some of the high risk types that are included in commercial HPV tests included types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, & 68. Smoking Smokers have a 50% higher risk of developing cervical cancer (ASC, 2000). Smoking elevates the risk of cervical cancer by exposing women who smoke and those who inhale second-hand smoke to cancer-causing chemicals that damage the DNA in cells of the cervix. A woman's risk increases relative to the number of cigarettes smoked per day and the number of years she has smoked. Essentially there are two invasive cervical cancer prevention strategies: 1- Primary Prevention: prevent cervical cancer precursors. Precursors can be prevented by decreasing exposure to HPV by delaying sexual intercourse and limiting the number of sexual partners. Abstaining from smoking is another way to decrease the risk of cervical cancer precursor lesions. 2- Secondary Prevention: routine Pap test screening. Pap test screening helps to identify cervical cancer precursor lesions at the earliest, most treatable stage. The risk of developing invasive cervical cancer is 3 to 10 times greater in women who have not been screened (NCI, 2002). The risk also increases with longer duration following the last normal Pap test. Screening every 2 to 3 years, however, has not been found to increase likelihood the risk of finding invasive cervical cancer above the risk expected with annual screening (NCI, 2002). WWHP’s CERVICAL CANCER SCREENING POLICY PAP TEST SCREENING FREQUENCY In 1988, a consensus recommendation was developed by the American College of Obstetricians and Gynecologists (ACOG), the American Nurses Association, the American Cancer Society, the National Cancer Institute, the American Medical Association, the American Academy of Family Physicians, and the American Medical Women's Association. The recommendation suggested that all women who are or who have been sexually active, or women who have reached 18 years of age should have an annual cervical Pap test and pelvic examination. It was further recommended that after a woman had three or more consecutive satisfactory annual examinations, the Pap test could be performed less frequently at the discretion of her physician. The U.S. Preventive Services Task Force (1996) recommended that the time between Pap tests should be 1-3 years, depending on the presence of risk factors for cervical cancer. The risk of an abnormality occurring within 3-5 years after three consecutive negative annual smears is minimal in low-risk patients. Pap test screening of high-risk women should be scheduled annually; however, the physician may feel that screening more frequently is necessary. DEFINITIONS: Consecutive - refers to the Pap test results within the specified time period of five years (60-months). For example, if a woman who has been enrolled in the program for 5-years presents for a Pap test in 2001 and she has had three "consecutive" normal Pap test results in 1997, 1999, and 2000 she would not be eligible for Pap test screening until 2003. Page 49 of 73 SERIAL #: PH RFP 12-023 Documented - all Pap tests to calculate screening interval must be done while enrolled in the WWHP and documented in the WWHP CaST database. Normal Pap test result - includes a result of Negative for Intraepithelial lesion or Malignancy. Screening Interval - the time between screening Pap tests. Seventy-five percent of the women who have had three documented and consecutive normal Pap test results over a five-year period (60 months) should NOT have a Pap test when they return for cervical cancer screening the fourth year. The screening interval for these women should increase to a Pap test once every three years. Twenty-five percent of women screened by the WWHP may continue to have annual Pap tests if they meet the high-risk criteria defined by the WWHP Medical Advisory Board. Women with an Abnormal Pap Test Result Women who have had a history of prior dysplasia may be screened annually or more frequently as determined by their clinician. Pap testing should not exceed four Pap tests within a 12-month period. Often clinicians will request repeat Pap tests at a screening interval of 3, 4, 6, or 9 months. Once the abnormal Pap test results resolve and there are three documented normal Pap test results over a period of three years, the screening interval should be increased to once every three years. If later a woman has an abnormal Pap test, she would resume more frequent screening, as determined by her clinician. Cervical Cancer Risk Criteria Twenty-five percent of the women screened for cervical cancer may continue with annual screening, at the discretion of their clinician. Providers wishing to continue annual re-screening, in the presence of three consecutive normal Pap test results, must document in the comment section of the WWHP screening form the client's cervical cancer risk or other rationale for continued annual Pap test screening. To be eligible for annual Pap test screening women must meet the following criteria: Abnormalities were found within the last three years; OR There is presence of anyone of the following: o Five or more sexual partners in a lifetime o History of a sexually transmitted disease o History of HIV/lmmunosuppression o Absence of any Pap smears within the previous seven years o Prenatal exposure to DES (diethylstilbestrol) SCREENING POST HYSTERECTOMY Although vaginal smears are often done for follow-up of women who have had a hysterectomy for malignancy, a retrospective study suggests little or no benefit of routine vaginal screening for women who have had a hysterectomy for reasons other than cervical neoplasia. Investigators found a low prevalence of vaginal dysplasia (0.1%) and a high false positive rate of vaginal smears from women who have had a hysterectomy for benign disease (NCI, 2002). Approximately 35 percent of women 50 years of age or older have had a hysterectomy. The majority of women who have had a hysterectomy do not have a cervix and are not at risk for developing cervical cancer. If a woman gives a history of a hysterectomy for cervical neoplasia, she should be followed with an annual Pap test for three years following the hysterectomy. If all three consecutive Pap tests are within normal limits, her screening interval should be increased to Pap tests every three years, rather than annually. A woman should not have a Pap test, through the WWHP, if she has had a hysterectomy for fibroids or reasons other than cervical dysplasia. A small percentage of women have had a supracervical hysterectomy and have an intact cervix. The presence of a cervix is easily determined on physical examination. These women are at risk of developing cervical cancer. Therefore, they require continued Pap smears based on the current cervical screening policy. Page 50 of 73 SERIAL #: PH RFP 12-023 WWHP Cervical Cancer Screening Policy for Women Post Hysterectomy WWHP Reimbursable Procedures Pelvic Exam Pap test Women who have had a hysterectomy for cervical neoplasia Yes Yes Women who have had a supracervical hysterectomy (cervix intact). Yes Yes Women who have had a hysterectomy for reasons other than cancer or cervical dysplasia; but are unsure if their cervix is intact. Women who have had a hysterectomy for reasons other than cervical neoplasia, and do not have a cervix. Yes Yes, if they have a cervix or history of cancer ---------------------------No, if they do not have a cervix No No COMPLETING THE CYTOLOGY LABORATORY REQUISITION FORM At a minimum, the following information should be accurately completed on the cytology requisition form: the patient's first and last names, her age and/or date of birth, the source of the specimen and the date it was collected. The name, address and telephone number of the requesting clinician should also be included to ensure prompt reporting. To assist the cytology technicians and cytopathologists with a thorough interpretation of the Pap test specimen, the cytology requisition form should also include information with regard to the patient's clinical history. Information such as the date of the patient's last menstrual period (LMP), parity, postmenopausal, estrogen or other hormone therapy, use of an intrauterine device (IUD), diethylstilbestrol exposure, chemotherapy, radiation therapy, previous gynecologic surgeries/treatments, history of cancer, previous abnormal cytology results, and any clinical findings observed at the time of examination, such as an infection or visible lesion. ADEQUACY/QUALITY OF PAP TEST SPECIMEN The Pap test, when correctly obtained from a woman with a cervix, should contain endocervical components from the squamocolumnar junction and material from the ectocervix. Studies have shown that the use of an endocervical brush can increase the yield of endocervical cells by seven-fold (ACOG Technical Bulletin, August 1993). It is strongly recommended that an endocervical brush be used to collect the endocervical specimen, in addition to the use of a plastic cervical spatula. The use of a wooden spatula and/or cotton tipped swab are strongly discouraged as they both retain cellular materials (ASC, 2000). The presence of the endocervical component (endocervical cells and/or squamous metaplastic cells and/or cervical mucus with endocervical cells) in the Pap test indicates that the transformation or squamocolumnar junction zone has been sampled. The endocervical component should be present in the Pap test collected from most premenopausal patients with a cervix. It is not uncommon for the endocervical component to be absent in Pap tests from pregnant, post-hysterectomy, and post-menopausal women, as well as those women who have cervical conization and LEEP procedures. If endocervical cells are absent, and if the patient has a poor screening history, it is suggested that the Pap test be repeated in 3-6 months. If the patient has routinely been screened with a history of normal Pap tests, the patient should be instructed to return at the appropriate routine screening interval. Page 51 of 73 SERIAL #: PH RFP 12-023 REPORTING OF PAP TEST RESULTS The Bethesda System The National Cancer Institute convened the first workshops on the Bethesda System in 1988 and 1991 to clarify the confusion of multiple cytological reporting systems. The goals were to provide better communication between the cytopathologists and the referring providers and to facilitate cytologic and histologic correlation in cervical and vaginal samples. The classification that was developed is called The Bethesda System (TBS) for reporting the Cervical/Vaginal Cytological Diagnoses. The National Cancer Institute convened a third workshop, Bethesda 2001, held April 30 -May 2, 2001, to review issues regarding terminology and reporting of cervical cytology. Nine forum group sessions covered topics including: specimen adequacy, non-neoplastic changes, atypical squamous cells of undetermined significance (ASCUS), atypical glandular cells of undetermined significance (AGUS), ancillary testing (HPV DNA testing, etc.), endometrial cells, squamous intraepithelial lesion (SIL), automated computer review, and recommendations. The groups revised the Bethesda System of reporting to include the following reporting system, now referred to as the Bethesda System 2001. The Bethesda System 2001 includes the following features (detailed in Figure 1). A description of specimen type, an evaluation of specimen adequacy, an interpretation/result of the specimen, the method of review, and all ancillary testing performed on the specimen and the result(s) of the ancillary testing. Page 52 of 73 SERIAL #: PH RFP 12-023 Figure 1 SPECIMEN TYPE SPECIMEN ADEQUACY Satisfactory for Evaluation Unsatisfactory for Evaluation (reason specified) GENERAL CATEGORIZATION Negative for Intraepithelial Lesion or Malignancy Epithelial Cell Abnormality (“Squamous” or “Glandular” specified) AUTOMATED REVIEW ANCILLARY TESTING BETHESDA SYSTEM 2001 Conventional Pap test, Liquid-based or other technology Specimen rejected/not processed (reason specified) Specimen processed and examined, but unsatisfactory for evaluation of epithelial abnormality because of (reason specified) INTERPRETATION/RESULT ORGANISMS Trichomonas vaginalis Fungal organisms morphologically consistent with Candida spp. Shift in flora suggestive of bacterial vaginosis Bacteria morphologically consistent with Acitnomyces spp. Cellular changes consistent with Herpes simplex virus OTHER NON-NEOPLASTIC FINDINGS Reactive cellular changes associated with: inflammation; radiation; or intrauterine contraceptive device (IUD) Glandular cells status post hysterectomy Atrophy OTHER Endometrial cells in women 40 years of age SQUAMOUS CELL Atypical Squamous cells Of undetermined significance (ASC-US) Cannot exclude HSIL (ASC-H) Low Grade Squamous intraepithelial lesion (LSIL) Encompassing: HPV/mild dysplasia/CIN I High Grade Squamous intraepithelial lesion (HGSIL) Encompassing: moderate and severe dysplasia, CIN 2 and 3, CIS Squamous cell carcinoma GLANDULAR CELL Atypical Endocervical cells (NOS or specified comments) Endometrial cells (NOS or specified comments) Glandular cells (NOS or specified comments) Atypical Endocervical cells, favor neoplastic Glandular cells, favor neoplastic Endocervical Adenocarcinoma in situ Adenocarcinoma Endocervical Endometrial Extrauterine Not otherwise specified (NOS) OTHER Other Malignant Neoplasms If examined by an automated device, the device should be specified If an ancillary test is performed, a brief description of the test methods and a report, results should be included Page 53 of 73 SERIAL #: PH RFP 12-023 FOLLOW-UP and MANAGEMENT OF PAP TEST FINDINGS NEGATIVE FOR INTRAEPITHELIAL LESION OR MALIGNANCY Notify the patient of the Pap test results, and instruct the patient in the importance of returning for her next screening Pap test at the determined interval(s), or if she becomes symptomatic with any gynecological problems. NEGATIVE FOR INTRAEPITHELIAL LESION OR MALIGNANCY, WITH: I. Organisms: Trichomonas vaginalis Fungal organisms morphologically consistent with Candida spp. Shift in flora suggestive of bacterial vaginosis Bacteria morphologically consistent with Actinomyces spp. Cellular changes consistent with Herpes simplex virus Notify -the patient of her Pap test results and have her return for a culture and/or wet mount, if needed, to identify the causative agent (if not done at time of the initial visit). Counsel the patient and offer a course of treatment for specific type of vaginitis. Verify this action by documenting it in the patient's medical record. Schedule the patient for a clinic visit. o Trichomonas vaginalis may be managed by treatment if the patient is symptomatic. If there are no symptoms, a confirmatory test should be considered. Resume routine screening. o Women presenting with fungal organisms morphologically consistent with Candida spp should be offered therapy, if symptomatic. Resume routine screening. o Shift in flora suggestive of bacterial vaginosis (BV), offer therapy for BV only if symptomatic. Resume routine screening. o Bacteria morphologically consistent with Actinomyces spp. is significant if intrauterine device is in situ. If a patient with an IUD is asymptomatic for pelvic inflammatory disease, then antimicrobial treatment or following the patient with no treatment may be appropriate. The IUD need not be removed in the asymptomatic patient. o Cellular changes consistent with Herpes simplex virus (HSV) are suggestive of HSV shedding. HSV culture or treatment is unnecessary unless indicated for other reasons. Resume routine screening. For guidelines on treatment please refer to the Centers for Disease Control and Prevention, 2002 STD Treatment Guidelines, available online at: http://www.cdc.gov/nchstp/dstd or hardcopies are available by phone at: 1-888- 232-3228 (press 2,5,1,1 to go to STD information), or by Mail: DSTDP, Training & Health Communications Branch, 1600 Clifton Rd., NE Mailstop E-02, Atlanta, GA 30333 NEGATIVE FOR INTRAEPITHELIAL LESION OR MALIGNANCY, WITH: II. Other Non-Neoplastic Findings: Notify the patient of the Pap test report and the need to follow the recommendations of the health care provider. Verify this action by documenting it in the patient's medical record. Schedule the patient for a clinic visit. Reactive cellular changes This finding includes reactive cellular changes associated with inflammation, radiation and the use of an intrauterine contraceptive device (IUD) o Inflammation could be due to gonorrhea, chlamydia, or other pathogens. Consider contacting patient and offer testing for gonorrhea, chlamydia, and/or a wet mount for other pathogens, as indicated. Page 54 of 73 SERIAL #: PH RFP 12-023 o o Women with reactive cellular changes and a history of radiation therapy should be re-screened in one year. Women with reactive cellular changes and have an intrauterine device (IUD) in place should be re-screened in one year. Glandular cells post-hysterectomy This finding is considered benign. Resume routine screening. Atrophy Atrophic changes or atrophy with inflammation (Atrophic Vaginitis) is a potential indication for treatment with estrogen. Treatment options include estrogen vaginal cream (daily) or oral regimens. o Treatment with estrogen is contraindicated if there is a history of breast cancer (estrogen dependent or unknown receptors), endometrial cancer/undiagnosed vaginal bleeding, or a history of deep vein thrombosis. NEGATIVE FOR INTRAEPITHELIAL LESION OR MALIGNANCY, WITH: III. Other: Endometrial Cells in women 40 years of age This may indicate a need to evaluate the endometrium (such as an endometrial biopsy). This may be an indication for this procedure especially if the patient has abnormal bleeding/post menopausal bleeding circumstances that would usually call for an evaluation of the endometrium. If the Pap was unrelated to menses, then an endometrial evaluation might be considered. EPITHELIAL CELL ABNORMALITY Squamous Cells Atypical Squamous Cells: Pap test results interpreted as atypical squamous cells of undetermined significance (ASC-US) have a 5-17% chance of having cervical intraepithelial neoplasia (CIN) 2, 3 confirmed by biopsy, while CIN 2, 3 is identified in 24 - 94% of women with ASC-H (atypical squamous cells, cannot exclude high grade intraepithelial lesions) (JAMA, 2002). Atypical Squamous Cell of Undetermined Significance (ASC-US) Notify the patient and counsel her regarding the seriousness of the Pap test report and the need to follow the recommendations of the health care provider. Verify this action by documenting it in the patient's medical record. Schedule the patient for a clinic visit. The preferred approach to managing women with ASC-US diagnosed by conventional Pap test includes co-collected DNA* testing for oncogenic HPV types (high-risk HPV panel only); OR patients with ASCUS may be followed with repeat Pap testing. If repeat cytology is the method of follow-up, women should have a repeat Pap test within 4-6 months. If the repeat Pap test is negative the patient can resume routine screening. If the HPV DNA is positive for high-risk types of HPV, or if one of the repeat Pap test is positive (ASC-US or more severe) the patient should be referred for colposcopy. Another acceptable approach is immediate colposcopy for the patient with ASC-US. Post-menopausal women with ASC-US, with evidence of atrophy, can be managed by undergoing a 3-6 week course of intravaginal estrogen cream followed by a repeat Pap test one week after the completion of estrogen therapy. If the repeat Pap test is "negative for intraepithelial lesion or malignancy" (NIL) the patient should be referred for a repeat Pap test in 4-6 months. If NIL, the patient can be referred for routine Pap test screening. Women may also be referred for immediate HPV DNA testing, repeat cytology or colposcopy (as noted in the managing women with ASC-US bullet). Women who are immunosuppressed should be referred for immediate colposcopy. This includes women who are HIV positive regardless of CD4 count or therapy. Page 55 of 73 SERIAL #: PH RFP 12-023 Pregnant women should be followed per the guidelines for non-pregnant women with ASC-US (as noted in the managing women with ASC-US bullet). Atypical Squamous Cells Cannot Exclude High Grade Squamous Intraepithelial Lesion (ASC-H) Notify the patient and counsel her regarding the seriousness of the Pap test report and the need to follow the recommendations of the health care provider. Verify this action by documenting it in the patient's medical record. Schedule the patient for a clinic visit. Women should always be referred directly for colposcopic evaluation, with subsequent follow-up determined by the findings at evaluation. *This approach is only cost effective if DNA specimen is obtained at the time of original Pap smear, “reflex testing,” usually with a liquid-based specimen. SQUAMOUS INTRAEPITHELIAL LESIONS Squamous intraepithelial lesion encompasses a spectrum of noninvasive cervical epithelial abnormalities traditionally classified as a flat condyloma, dysplasia/carcinoma in-situ, and CIN. In the Bethesda System 2001, the spectrum is divided into low-grade and high-grade lesions. Low-grade lesions (LSIL) encompass the cellular changes associated with HPV cytopathic effect (koilocytotic atypia) and mild dysplasia/CIN 1. High-grade lesions (HSIL) encompass moderate dysplasia, severe dysplasia, and carcinoma in-situ/CIN 2, 3). Gynecological cytology cases showing diagnostic HSIL in which there is a non-diagnostic cytological evidence of invasion should be diagnoses as HSIL and accompanied by the comments "with features suspicious for invasion." Source: Bethesda 2001 Post-Workshop Recommendations Page 56 of 73 SERIAL #: PH RFP 12-023 Low Grade Squamous Intraepithelial Lesion (LSIL) Approximately 15-30% of women with LSIL on cervical cytology will have CIN 2, 3 identified on a subsequent cervical biopsy (JAMA, 2002). The National Cancer Institutes ASCUS/LSIL Triage Study (AL TS) noted that 83% of the women referred for LSIL evaluation tested positive for high-risk HPV types (JAMA, 2002). Notify the patient and counsel her regarding the seriousness of the Pap test report and the need to follow the recommendations of the health care provider. Verify this action by documenting it in the patient's medical record. Schedule the patient for a clinic visit. The next step in patient management for LSIL is colposcopy. If high-grade dysplasia (CIN) is confirmed on the colposcopy the patient needs treatment. If no dysplasia is found on colposcopy the the patient will need follow-up Paps at 6 and 12 months. If all are NIL then she can resume yearly screening. If ASC-US or greater, then refer again for colposcopy. Postmenopausal women with LSIL with evidence of atrophy should be offered a course of intravaginal estrogen cream treatment for 3-6 weeks; 1 week post- treatment the Pap test should be repeated. If the repeat Pap test is positive (ASC-US or more severe) refer for colposcopy. If the repeat Pap test is negative, repeat the Pap test in 6 months. Alternatively, immediate colposcopy can be offered. OR HPV DNA testing can be offered - - those positive for high-risk HPV types are referred for colposcopy, and those with a negative test being rescreened with a Pap in 12 months. Pregnancy Recommendations. In most cases, pregnant women with LSIL should be referred for colposcopy High Grade Squamous Intraepithelial Lesion (HSIL) Notify the patient and counsel her regarding the seriousness of the Pap test report and the need to follow the recommendations of the health care provider. Verify this action by documenting it in the patient's medical record. Schedule the patient for a clinic visit. HSIL SHOULD ALWAYS BE REFERRED FOR COLPOSCOPY. Schedule the patient for immediate colposcopy. The colposcopy is considered satisfactory if the entire squamo-columnar junction is visualized. Patient management is directed by the result of this examination and the results of histological evaluation obtained by a directed biopsy of the abnormal area defined on colposcopy exam. If CIN 2-3 is identified, definitive treatment is indicated. Treatment may include conization, laser ablation, LEEP and in some cases cryosurgery or hysterectomy. If the colposcopy is satisfactory, and only CIN 1 or no CIN is found. A review of the Pap, colposcopy and histology should be done (with one pathologist reviewing all materials). Treatment should be managed according to a revised diagnosis. If HSIL is upheld on review of the Pap and not confirmed with the colposcopy and biopsy then a LEEP or cone biopsy is recommended. If the colposcopy is considered unsatisfactory and no lesion visualized. The materials should be reviewed as the above bullet and managed accordingly. If the colposcopy is unsatisfactory and CIN is found on histology then the patient should undergo treatment with a LEEP or cone biopsy. Note: The cytobrush should be used to sample the endocervix in the follow-up of women with HSIL. Squamous Cell Carcinoma Notify the patient and counsel her regarding the seriousness of the Pap test report and the need to follow the recommendations of the health care provider. Verify this action by documenting it in the patient's medical record. Schedule the patient for a clinic visit. Promptly refer the patient for evaluation and treatment. Page 57 of 73 SERIAL #: PH RFP 12-023 GLANDULAR CELLS The atypical glandular cell (AGC) category is associated with a substantially greater risk for cervical neoplasia than atypical squamous cells or LSIL categories. Studies have found that 9-54% of women with AGC have biopsied confirmed CIN, 0-8% have biopsy confirmed adenocarcinoma in-situ (AIS), and less than 1- 9% have invasive carcinoma (JAMA, 2002). Atypical (Not Otherwise Specified [NOS] or Specified Comments): Endocervical Cells, Endometrial Cells Atypical Glandular Cells Atypical, Favor Neoplastic: Endocervical Cells or Glandular Cells Endocervical Adenocarcinoma In Situ Adenocarcinoma: Endocervical Endometrial Extra uterine Not Otherwise Specified Other: Malignant Neoplasm Notify the patient and counsel her regarding the seriousness of the Pap test report and the need to follow the recommendations of the health care provider. Verify this action by documenting it in the patient's medical record. Schedule the patient for a clinic visit. All women with atypical glandular or atypical endocervical cells should have colposcopy and endocervical curettage (ECC). Management with repeat Pap testing is NOT acceptable. Women with atypical glandular cells who are over 35, or women younger than 35 with AGC who have abnormal vaginal bleeding, should have an endometrial biopsy (EMB). Women with an atypical glandular cell Pap test, with a negative colposcopy, biopsy, and ECC should be followed with repeat Pap testing every 4-6 months until the woman has had four normal Pap tests. Women with atypical endometrial cells should have an endometrial biopsy (EMB). Women with atypical glandular cells that favor neoplasia or adenocarcinoma in-situ should have colposcopy and endocervical curettage (ECC). If disease is not identified through the initial work-up, a cold knife cone biopsy is recommended. (Please note: The WWHP cannot reimburse for cone- biopsy). Women diagnosed with invasive cancer on biopsy or ECC requires definitive therapy and should be referred to a gynecologic oncologist. FOLLOW-UP and MANAGEMENT OF PELVIC EXAMINATION FINDINGS WWHP's Policy with regard to the Removal of Cervical Polyps Cervical polyps are most often benign lesions and are primarily removed to alleviate symptoms such a post-coital and/or mid-cycle bleeding. Under the reimbursement guidelines of the National Breast and Cervical Cancer Early Detection Program the removal of a cervical polyp (polypectomy) as an independent procedure is not an allowable procedure. However, if a gross cervical lesion, suspicious for cancer, is observed during the client's pelvic examination, this lesion should be biopsied immediately to rule out cancer. In such cases, if the pathology report describes the biopsied lesion as a benign growth, such as a cervical polyp, the program may reimburse providers for the biopsy procedure - as the procedure was performed specifically to rule out malignancy. Page 58 of 73 SERIAL #: PH RFP 12-023 HOW TO CHOOSE A QUALITY CYTOLOGY LAB By Sharon Siweck, CT When seeking to provide cervical screening services it is imperative to have the necessary skills to select a quality laboratory that will provide a consistent and high level of proficiency. This becomes more crucial when the target group being offered Pap test screening falls into a " high risk" category identified by either the lack of recent and consistent cervical screening, or other contributing factors such as a previous abnormal pap test, sexually transmitted disease, multiple partners, early onset of sexual activity, or prenatal exposure to DES. Critical to the selection process of a reputable laboratory are several components: 1. Does the lab have American Society of Cytopathology accreditation? This is considered to be the hallmark certification of a very high quality laboratory. Minimally, the lab must have a CLIA number, and frequently will have College of American Pathologists recognition. 2. The Arizona Department of Health Services, Office of Laboratory Licensure and Certification can provide information on recent surveys of the laboratory. The last two surveys performed are available under the "Freedom of Information Act" and may be requested in writing to ADHS, OLLC, 3443 N. Central, Suite 810, Phoenix, AZ 85012. There is a per page charge. The Centers for Medicaid and Medicare Services (CMS) additionally conducts "Specialized Reviews of Cytology Laboratories." The intensive and comprehensive nature of these surveys far exceeds all others. Survey findings may be available either through your State of Federal Regional Offices or through the Freedom of Information Act from (CMS). 3. Request from the laboratory a description of the diagnostic classification system they use, it should be the Bethesda System. Ask for a copy of the requisition form and an example of a report. 4. The laboratory should supply a copy of the laboratory's specimen submission and handling procedures. The procedures should detail how specimens will be submitted to the lab and the type of supplies they will provide to providers utilizing their laboratory. 5. Ask if the laboratory has adequate cytotechnologist staffing to accommodate your estimated volume and the estimated turn around time for report receipt. Also determine if the laboratory distributes work out to satellite laboratories or subcontracts with an outside laboratory. This must be identified on the report form. 6. Request a copy of the laboratory's annual statistics that identify: *total case/slide volume of Pap tests *number of cases reported by diagnosis *number of cases with discrepant cyto/histo correlation (if the lab is being utilized for biopsy correlation testing) 7. Identify who the laboratory contact person will be in the event of problems or questions. LABORATORY INDICATORS Atypical Glandular Cells in a typical cytology laboratory should be less than 1%. Atypical Squamous Cells in a typical cytology laboratory should not exceed 5% of total specimens with ASC:SIL ratios not higher than 2:1 to 3:1 in general screening populations. Source: Bethesda 2001 Post-Workshop Recommendations Page 59 of 73 SERIAL #: PH RFP 12-023 Page 60 of 73 SERIAL #: PH RFP 12-023 Page 61 of 73 SERIAL #: PH RFP 12-023 CERVICAL ALGORITHM Algorithm 1. Management of Women with a Histological Diagnosis of Cervical Intraepithelial Neoplasia Grade 1 (CIN1) Preceded by ASC-US, ASC-H, or LSIL Cytology Algorithm 2. Management of Women with a Histological Diagnosis of Cervical Intraepithelial Neoplasia Grade 1 (CIN1) Preceded by HSIL or AGC-NOS Cytology Algorithm 3. Management of Adolescent Women (20 years and younger) with a Histological Diagnosis of Cervical Intraepithelial Neoplasia Grade 1 (CIN1) Algorithm 4. Management of Women with a Histological Diagnosis of Cervical Intraepithelial Neoplasia- (CIN 2,3) Algorithm 5. Management of Adolescent and Young Women with a histological Diagnosis of Cervical Intraepithelial Neoplasia- Grade2,3 (CIN 2,3) Algorithm 6. Management of Women with Adenocarcinoma in-situ (AIS0 Diagnosed from a Diagnostic Excisional Procedure Page 62 of 73 SERIAL #: PH RFP 12-023 Page 63 of 73 SERIAL #: PH RFP 12-023 Page 64 of 73 SERIAL #: PH RFP 12-023 Page 65 of 73 SERIAL #: PH RFP 12-023 Page 66 of 73 SERIAL #: PH RFP 12-023 Page 67 of 73 SERIAL #: PH RFP 12-023 Page 68 of 73 SERIAL #: PH RFP 12-023 CERVICAL REFERENCES American Society of Colposcopy and Cervical Pathology (ASCCP). 2006. Available online: http://www.asccp.org. American Society of Cytopathology (ASC), 2000, ASC Guidelines. Available Online: www.cytopathology.org Solomon D., Davey D., Kurman R., Moriarty A., Oconnor D. (2002). Consensus Statement, The 2001 Bethesda System. JAMA, April 24, 2002- Vol 287, No 16 u.s. Preventative Health Task Force (USPHTF), 1996. Chapter 9. Screening for Cervical Cancer. Available Online: http://odphp.osophs.dhhs.gov/pubs/guidecps/text/CHO9. txt National Cancer Institute (NCI), 2002. Cervical Cancer (PDQ) Prevention, Screening and Treatment. Available Online: www.cancer.gov National Cancer Institute (NCI), 2001. Bethesda System 2001. Post-workshop Recommendations. Available Online: www.bethesda2001 cancer .gov Wright T., Cox JT, Massad S., Twiggs L., Wilkinson E., for the 2001 ASCCP- Sponsored Consensus Conference (2002). 2001 Consensus Guidelines for the Management of Women with Cervical Cytological Abnormalities. JAMA, April 24, 2002- Vol 287, No 16 Page 69 of 73 SERIAL #: PH RFP 12-023 EXHIBIT 4 2011 NBCCEDP Allowable Procedures, Relevant CPT® Codes, and Medicare Reimbursement Rates CPT Code Professional Component (-26) Technical Total Component Amount (-TC) Office Visit New Patient; history, exam, straightforward decisionmaking; 10 minutes New Patient; expanded history, exam, straightforward decision-making; 20 minutes New Patient; detailed history, exam, straightforward decision-making; 30 minutes New Patient: comprehensive history, exam, moderate complexity decision-making; 45 minutes New Patient: comprehensive history, exam, high complexity decision-making; 60 minutes Established Patient; evaluation and management, may not require presence of physician; 5 minutes Established Patient; history, exam, straightforward decision-making; 10 minutes Established Patient; expanded history, exam, straightforward decision-making; 15 minutes 99201 99202 99203 99204 99205 99211 99212 99213 Breast Screening & Diagnostic Screening Mammogram, Bilateral (2 view film study of each breast) Mammography, Diagnostic Follow-up, Unilateral $ 34.71 $ 34.71 77057 77055 Mammography, Diagnostic Follow-up, Bilateral 77056 Stereotactic localization guidance for breast biopsy or needle placement Mammographic guidance for needle placement, breast $ 43.13 $ 79.45 $ 27.64 77031 77032 Radiological examination, surgical specimen 76098 Ultrasound, breast(s), unilateral or bilateral, B-scan and/or real time with image documentation Ultrasonic guidance for needle placement, imaging supervision and interpretation Puncture aspiration of cyst of breast 76645 76942 $ 8.08 $ 26.94 $ 33.36 $ 45.40 $ 50.74 $ 66.11 $ 80.13 $ 27.70 $ 11.00 $ 68.11 $ 161.63 19000 Puncture aspiration of cyst of breast, each additional cyst, used with 19000 Breast biopsy, percutaneous, needle core, not using imaging guidance Breast biopsy, open, incisional 19001 19100 19101 Page 70 of 73 $ 40.59 $ 70.17 $ 101.69 $ 156.49 $ 194.90 $ 19.45 $ 40.93 $ 68.19 NonFacility $ 80.11 $ 85.45 $ 109.24 $ 159.59 $ 55.34 $ 19.08 $ 95.05 $ 194.98 $ 107.10 $ 26.17 $ 139.72 $ 318.56 SERIAL #: PH RFP 12-023 Breast biopsy, percutaneous, needle core, using imaging guidance; for placement of localization clip use CPT 19295 Breast biopsy, percutaneous, automated vacuum assisted or rotating biopsy device, using imaging guidance Excision of cyst, fibroadenoma or other benign or malignant tumor, aberrant breast tissue, duct lesion, nipple or areolar lesion; open; one or more lesions Excision of breast lesion identified by preoperative placement of radiological marker; open; single lesion Preoperative placement of needle localization wire, breast $ 209.71 $ 538.38 19102 19103 $ 461.02 $ 511.82 $ 157.09 $ 66.71 $ 88.82 $ 140.15 $ 134.66 19120 19125 19290 Preoperative placement of needle localization wire, breast; each additional lesion Image guided placement, metallic localization clip, percutaneous, during Fine needle aspiration without imaging guidance 19291 19295 10021 Fine needle aspiration with imaging guidance 10022 Breast Screening & Diagnostic Cytopathology, evaluation of fine needle aspirate; immediate cytohistologic study to determine adequacy of specimen(s) Cytopathology, evaluation of fine needle aspirate; interpretation and report Surgical pathology, gross and microscopic examination CPT Code 88172 88173 88305 Surgical pathology, gross and microscopic examination; requiring microscopic evaluation of surgical margins Screening Mammogram, Digital, Bilateral 88307 G0202* Diagnostic Mammogram, Digital, Bilateral G0204* Diagnostic Mammogram, Digital, Unilateral G0206* Anesthesia for procedures on the integumentary system, anterior trunk, not otherwise specified. Medicare Base Units = 3 (Each additional base unit = $20.84) Professional Component (-26) Technical Component (-TC) NonFacility $ 29.71 $ 67.84 $ 36.15 $ 78.98 $ 34.71 $ 42.80 $ 34.71 $ 20.35 $ 68.11 $ 68.44 $ 144.26 $ 103.51 $ 122.55 $ 96.16 $ 50.06 $ 135.95 $ 104.59 $ 223.24 $ 138.22 $ 165.35 $ 130.87 00400 $ 62.52 88164 $ 14.87 88141 $ 28.56 88142 $ 28.51 Cervical Screening & Diagnostic Cytopathology (conventional Pap test), slides cervical or vaginal reported in Bethesda System, manual screening under physician supervision Cytopathology (conventional Pap test), cervical or vaginal, any reporting system, requiring interpretation by physician Cytopathology (liquid-based Pap test) cervical or vaginal, collected in preservative fluid, automated thin layer preparation; manual screening under physician supervision Page 71 of 73 SERIAL #: PH RFP 12-023 Cytopathology, cervical or vaginal, collected in preservative fluid, automated thin layer preparation; manual screening and rescreening under physician supervision Cytopathology, cervical or vaginal, collected in preservative fluid, automated thin layer preparation; screening by automated system, under physician supervision Cytopathology, cervical or vaginal, collected in preservative fluid, automated thin layer preparation; screening by automated system and manual rescreening, under physician supervision Hybrid Capture II from Digene - HPV Test (High Risk Typing, only) Colposcopy of the cervix 88143 $ 28.51 88174 $ 30.06 $ 37.28 $ 49.39 $ 107.51 $ 152.41 $ 141.64 $ 133.93 $ 288.06 $ 324.21 $ 128.80 $ 100.74 88175 87621 57452 Colposcopy of the cervix, with biopsy and endocervical curettage Colposcopy of the cervix, with biopsy 57454 57455 Colposcopy of the cervix, with endocervical curettage 57456 Endoscopy with loop electrode biopsy(s) of the cervix 57460 Endoscopy with loop electrode conization of the cervix 57461 Biopsy, single or multiple, or local excision of lesion, with or without fulguration (separate procedure) Endocervical curettage (not done as part of a dilation and curettage) Conization of cervix, with or without fulguration, with or without dilation and curettage, with or without repair; cold knife or laser 57500 57505 $ 303.35 $ 261.80 57520 Loop electrode excision procedure LEEP 57522 Cervical Screening & Diagnostic CPT Code Endometrial sampling (biopsy) with or without endocervical sampling (biopsy), without cervical dilation, any method (separate procedure) 58100 Endometrial sampling (biopsy) performed in conjunction with colposcopy (List separately in addition to code for primary procedure) 58110 Surgical pathology, gross and microscopic examination 88305 Pathology consultation during surgery, first tissue block, with frozen section(s), single specimen Pathology consultation during surgery, first tissue block, with frozen section(s), each additional specimen 88331 88332 Professional Component (-26) Technical Component (-TC) NonFacility $ 108.81 $ 36.15 $ 59.11 $ 29.04 $ 68.44 $ 31.37 $ 11.00 Page 72 of 73 $ 47.92 $ 104.59 $ 90.48 $ 40.04 SERIAL #: PH RFP 12-023 ASC Rates with Relevant CPT Codes CPT Code 19000 Facility Price (for Provider) $ 43.64 19100 $ 67.91 $ 211.69 $ 102.16 $ 190.69 $ 391.55 $ 435.34 Drainage of breast lesion Bx breast percut w/o image 19101 Biopsy of breast, open 19102 Bx breast percut w/image 19103 Bx breast percut w/device 19120 Removal of breast lesion 19125 Excision, breast lesion Transportation Services (AHCCCS Rates) HCPS Code Non-emerg. transportation, per mile, volunteer Non-emerg. transportation, per mile, case worker A0080 A0160 Taxicab, base rate, per client Taxicab, rate/ per mile, urban Taxicab, rural base rate, per client Taxicab, rate/ per mile, rural Ambulatory Van, urban base rate per client Ambulatory Van, urban rate/ per mile Ambulatory Van, rural base rate per client Ambulatory Van, rural rate/ per mile Wheelchair Van, urban base rate per client Wheelchair Van, urban rate/ per mile Wheelchair Van, rural base rate per client Wheelchair Van, rural rate/ per mile A0100 S0215 A0100 S0215 A0120 S0215 A0120 S0215 A0130 S0209 A0130 S0209 Facility Fee $ 72.99 $ 169.57 $ 946.62 $ 300.96 $ 580.77 $ 946.62 $ 946.62 Amount 0.48 0.48 1.15 1.42 1.15 1.69 7.36 1.42 8.05 1.69 12.36 1.70 10.31 1.84 Page 73 of 73