BCCCNP Orientation Overview - Michigan Cancer Consortium
advertisement

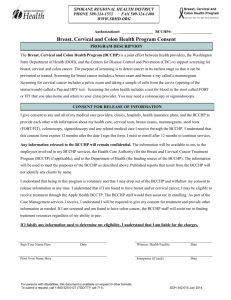
BCCCNP ORIENTATION OVERVIEW E.J. Siegl, Program Director/Nurse Consultant Ann Garvin, Nurse Consultant BCCCNP Program Management 1. Assure eligible women receive needed breast and/or cervical cancer caseload/navigation-only services. 2. Agency achievement of all Minimum Program Requirements for both caseload and navigation services. BCCCNP Caseload Services • Assist uninsured/underinsured clients (< 250% FPL) in obtaining appropriate screening and diagnostic services through the program in a timely manner • Monitor delivery and documentation of clinical services according to CDC Clinical Performance Indicators of Timeliness and Completeness • Monitor appropriate reimbursement of BCCCNP approved services for program clients BCCCNP Navigation Services • Assist insured clients(< 250% FPL) in identifying and addressing individual barriers that may impede their access to receiving screening, diagnostic, and/or treatment services through the healthcare system. BCCCNP Coordinator Responsibilities Program Management • Adherence to Minimum Program Requirements (includes program policies/procedures) • Caseload Monitoring – bi-monthly report • Client Outreach/Recruitment for program services • Provider Outreach/Relationship Building • Fiscal management Program Management MPR Review • Accreditation review every 3 years: off-site review • Requested documents sent to MDHHS reviewer Caseload Monitoring • Bi-monthly report posted on DCH File Transfer • Coordination reimbursement: $175/enrolled woman • To count in caseload: at least 1 service paid by program • FY 16 caseload requirements: must achieve 97% of caseload Program Management: Client Outreach/Recruitment 1. Challenge to agencies: Identifying women eligible for both caseload and navigation-only services 2. Annual Outreach/Recruitment Plan • Should include strategies to target eligible women • Use of MIYO patient education resources Program Management: Provider Outreach/Relationship Building 1. Work with health care providers, and other organizations (I.e. FQHC’s, Mammography Facilities) to identify eligible women that can be referred to BCCCNP 2. Link with community providers (CHWs) 3. Market the program’s services for all women (insured and uninsured) 4. Maintain frequent contact with providers Program Management Caseload Financial Requirements Monitor reimbursement for BCCCNP approved services 1. Assure BCCCNP is compliant with the “funds of last resort” requirement in the federal law. 2. Work with providers to assure reimbursement amount for each BCCCNP approved service is accepted as payment in full. 3. Program Financial resources - Unit Cost Reimbursement Rate Schedule - Financial Reports (Pended, Paid), Provider and Facility Form BCCCNP Coordinator Responsibilities Overseeing Caseload Services • Monitoring clinical service delivery according to BCCCNP Medical Protocol and CDC clinical performance indicators • Monitoring reimbursement of approved BCCCNP clinical services • Assuring accurate documentation of all program data BCCCNP Coordinator Responsibilities Overseeing Caseload Services • Monitoring clinical service delivery according to BCCCNP Medical Protocol and CDC clinical performance indicators • Monitoring reimbursement of approved BCCCNP clinical services • Assuring accurate documentation of all program data BCCCNP Caseload Service Components Clinical Care Delivery Caseload Services Documentation of Program Data Reimbursement of Clinical Services Caseload Services: Clinical Service Delivery Monitoring clinical services: • Abnormal breast or cervical screening results according to BCCCNP Medical Protocol and CDC clinical performance indicators • Eligibility to receive cancer treatment according to BCCCNP Medicaid Treatment Act Protocol BCCCNP Funding based on achievement of CDC’s clinical performance indicators of timeliness and completeness. BCCCNP Medical Protocol 1. Provision of clinical care for average risk women 2. Follow-up abnormal breast/cervical screening results according to CDC clinical indicators of timeliness and completeness 3. Guidelines for reimbursement of BCCCNP screening and diagnostic Services CDC Clinical Indicators Timeliness of Care (Immediate follow-up only) • 75% abnormal BREAST cases require final diagnosis within 60 days • 75% abnormal CERVICAL cases require final diagnosis within 90 days • 80% of all breast and cervical cancer diagnoses should begin treatment within 60 days of the final diagnosis Completeness of care: • 90% of abnormal breast or cervical cases requiring follow-up have at least ONE follow-up diagnostic procedure and a final diagnosis documented • 100% of cases with a breast or cervical cancer diagnosis have a treatment disposition documented within 100 days of the diagnosis Abnormal Results Requiring Immediate Follow-up CBE Results Abnormality - R/O Breast Cancer” (includes the following results: • Dominant mass • Nipple discharge-no palpable mass • Asymmetric thickening/ nodularity • Skin changes (Peau d’orange, erythema, nipple excoriation, scaling, eczema, skin ulcers) Mammogram • ACR 0 – Assessment Incomplete-additional imaging required Pap test • ASC-US with POSITIVE HPV – • ACR 4 - Suspicious Abnormality • ACR 5 - Highly Suggestive of Malignancy • ASC-H • LSIL • HSIL • AGC • Squamous cell carcinoma • Adenocarcinoma Documenting Clinical Services 1. Client Enrollment Form 2. Screening/Follow-up Forms 3. BCCCNP Informed Consent 4. Medicaid Application Form 5. Michigan Quit Line Fax Referral Form http://www.michigancancer.org/BCCCP (Follow this tree: LCA Information/Forms) Clinical Forms 1. Client Enrollment Form 2. Screening Form 3. Breast Follow-up Form 4. Cervical Follow-up Form • NOT A MANDATE TO USE FORMS • However, ALL information on forms must be collected and documented in MBCIS Clinical Services: BCCCNP Informed Consent Key Points to Discuss with Women • Program eligibility for uninsured/underinsured women. • Potential consequences for the client if insurance status is not accurately reported. • Description of breast and cervical cancer screening/ diagnostic tests available through the program • Statement that not all screening and diagnostic services are reimbursed by the program • Assistance to obtain cancer treatment if the woman is diagnosed through the program. • Statement that the contents of the form are in effect one year from date signed. FY15: Case Management • Monthly, list received w/ abnormal screening data. • Data gaps are in comments on form: Abnormal Exams - Incomplete Clinical Information FY 15 • Once data are complete – approved for CM. Form: Approved for Case Management Report FY 15 • Posted on DCH File Transfer • Use date and code found on form, and bill – only through FY15 • Current Reimbursement: $95.00 • Process will continue under different reimbursement and different title “Case Management” – in FY16, will be under Diagnostic Navigation • CBE: “Abnormality, rule/out cancer” need diagnostic mammogram and/or ultrasound or surgical consult to establish final dx. NO EXCEPTIONS. • Women with a significantly abnormal breast/cervical screening must continue to receive indicated follow-up diagnostic testing • Must have testing • Must have a final diagnosis (cancer/not cancer) • If cancer, must have a treatment disposition Diagnostic Navigation Process • Monthly, list received w/ abnormal screening data. • Data gaps are in comments on form: Abnormal Exams - Incomplete Clinical Information FY16 • Posted on DCH File Transfer • Process needs to continue as before; once care is complete in MBCIS, name will come off of form: Abnormal Exams - Incomplete Clinical Information FY16 Our work with Title X agencies (cervical) • In brief: women who are patients of Title X agencies (HD • • • • • FP clinics/Planned Parenthood) Have abnormal Pap needing colposcopy (MUST follow ASCCP Guidelines for women <age 25) Income ≤250% FPL, uninsured or underinsured BCCCNP pays for follow-up dx testing If treatment indicated (≥CIN2 final dx), put on BCCCNP Medicaid Treatment Act to pay for treatment Contact Ann Garvin (garvina@michigan.gov or 517-3359087) for diagnostic LEEP or Cone and EMB New in FY15 (breast) • Women <age 40 with abnormal CBE indicating a possible breast cancer diagnosis • Income ≤250% FPL, uninsured or underinsured • Agency refers to BCCCNP to schedule ultrasound (and, if indicated by results, surgical consult and/or mammogram) • Contact Ann Garvin to discuss management if any questions • If treatment indicated (DCIS, LCIS or Invasive Breast Cancer diagnosis), put on BCCCNP Medicaid Treatment Act to pay for treatment BCCCNP Medicaid Treatment Act • Client Eligibility • Client Enrollment (via Caseload Services or Navigation-Only Services) • Duration of Coverage for Cervical Treatment • CIN 2 (2-3 months), CIN 3 (6-7 months) (Guide for documenting Treatment Start Date) • Yearly Re-Determination • Hearing/Appeals BCCCNP Coordinator Responsibilities Overseeing Navigation Services Establish a network of medical and community providers to assist in: • Identifying insured eligible women (<250% FPL) requiring assistance in obtaining needed breast/cervical cancer services • Identifying resources for resolving barriers that may impede the woman from receiving breast/cervical cancer services Navigation-Only Services 1. Readiness to Learn 2. Form completion: - Intake Assessment - Encounter Summary - MTA Encounter Summary October 1, 2015 Algorithm to Assess Client’s Readiness to Screen NO Client NOT Eligible for Navigation-Only Services 1. Client due for breast/cervical screening? YES NO 2. Client WILLING to receive needed services? DO NOT COMPLETE NAVIGATION FORMS OR ENTER DATA IN MBCIS YES NO FINAL CLIENT ENCOUNTER Complete Navigation Encounter Form Navigation-Only Services Completed **Assistance/Intervention Needed for: · System Barriers, · Financia Barriers, · Psychosocial Barriers, · Communication Barriers FIRST CLIENT ENCOUNTER Complete Navigation Intake Assessment Form 3. Client needs agency help in scheduling services? ** YES YES 4. Client received needed services? NO Data Management Program Data Requirements 1. MBCIS User Agreement/User Access Form- All applications • Documenting Clinical/Non-Clinical Data in MBCIS • Caseload Reports – BI-weekly reports from Mike Carr • DCH File Transfer for confidential patient information ACCESS to Applications – Step 1 • User Agreement Form • MBCIS • Discoverer • Patient Navigation • DCH File Transfer • Cancer Mapper • Fax to 517-335-8752 Single Sign On – Step 2 • SSO Application Portal • https://sso.state.mi.us • Subscribe to Applications MBCIS, Discoverer, DCH File Transfer & Cancer Mapper Access Instructions • For complete, step-by-step instructions, please go to: www.michigancancer.org/BCCCP • LCA Information > Manuals > MBCIS, Discoverer, DCH File Transfer, or Cancer Mapper MBCIS Access Instructions Discoverer Access Instructions DCH File Transfer Access Instructions Cancer Mapper User Guide and Access Instructions Website Utilization www.michigancancer.gov/BCCCP • BCCCNP Caseload Eligibility & Services • How to Become a Provider • Benefits of Becoming a Provider • Patient Navigation • Patient Navigation Protocol • Forms • Rates & Codes • Presentations • LCA Information • Agency Best Practices • Clinical • Clinical Webinars • Early Detection Clinical Protocols • BCCCNP Medical Protocol • BCCCNP Medicaid Treatment Act Website Utilization www.michigancancer.gov/BCCCP • Resources & Materials • Affordable Care Act (ACA) & Healthy Michigan Plan (HMP) • BCCCNP Annual Meetings • MDHHS Cancer Fact Sheets • Patient Education • Webinars • Federal Poverty Guidelines • Miscellaneous • Breast Cancer Awareness License Plate • Breast & Cervical Cancer Screening Brouchure • Patient Information • Breast Density Info • Cervical Cancer Info Website Utilization www.michigancancer.gov/BCCCP • Billing & Reimbursement • Rate Schedules • ICD-10 Codes • Revenue Codes • Place of Service Codes • Hold Codes • Billing & Reimbursement Guide • Billing Guidelines – Paper & Electronic Claim Submission • Procedure Code Reference Chart Website Utilization www.michigancancer.gov/BCCCP • LCA Information > Manuals > • MBCIS • MBCIS Access Instructions • MBCIS Online Training for Clinical Access • MBCIS Basic Data Entry • MBCIS Clinical Data Entry • Cancer Mapper • DCH File Transfer • Discoverer • LCA Information > Forms • • • • • • • • Client Enrollment Form Screening and Follow-Up Forms Informed Consent Medicaid Application MBCIS User Application Form Provider & Facility Form Michigan Tobacco Quit line Fax Referral Form HPV Materials Order Form DISCOVERER • User Name = same as your SSO login for MBCIS • Password – if you have forgotten your password, or need it reset, please contact Tory Doney at 517-335-8854 or DoneyT@michigan.gov. • Database = pbc2 (peanut butter cookies) DISCOVERER DISCOVERER - *NEW* PEND • The MOST IMPORTANT Billing & Reimbursement report that can be run! DISCOVERER - *NEW* PEND DISCOVERER - *NEW* Payments DISCOVERER - *NEW* Payments Questions???? Contact Information: • Ann Garvin (GarvinA@michigan.gov; 517-335-9087) (Clinical, Breast and Cervical Cancer, Case Management, <age 40 Questions) • E.J. Siegl (SieglE@michigan.gov; 517-335-8814) (Program, MTA, QI Questions) • Tory Doney (DoneyT@michigan.gov; 517-335-8854) (Billing and Reimbursement Questions) • Sam Burke (BurkeS5@michigan.gov ; 517-241-6913) (Billing and Reimbursement Questions)