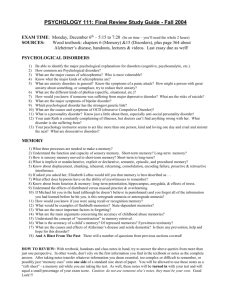
Substance Dependence - People Server at UNCW
advertisement
Abnormal Psychology WEB Anxiety as a Normal and an Abnormal Response • Some amount of anxiety is “normal” and is associated with optimal levels of functioning. • Only when anxiety begins to interfere with social or occupational functioning is it considered “abnormal.” The Bell Curve Phobic Disorders • 1. 2. 3. Phobias Specific phobias Social phobia Agoraphobia Specific Phobias Social Phobia • General characteristics Fear of being in social situations in which one will be embarrassed or humiliated Panic Disorder With and Without Agoraphobia • • • • Panic disorder Panic versus anxiety Agoraphobia Agoraphobia without panic Panic and the Brain Panic Disorder: The Cognitive Theory of Panic Treating Anxiety Disorders • Medications • Behavioral and cognitive-behavioral treatments Generalized Anxiety Disorder • General characteristics • Prevalence and age of onset • Comorbidity with other disorders Generalized Anxiety Disorder: Biological Causal Factors • Genetic factors • A functional deficiency of GABA • Neurobiological differences between anxiety and panic Obsessive-Compulsive Disorder • Obsessions- repetitive unwanted ideas that the person recognizes are irrational • Compulsions- repetitive, often ritualized behavior whose behavior serves to diminish anxiety caused by obsessions Post-Traumatic Stress Disorder • Critical Component – Symptoms occurs AFTER a traumatic stressor Symptoms Categories • Intrusive – – – – – distressing recollections dreams flashbacks psychological trigger reactions physiological trigger reactions Symptoms Categories • Avoidance – – – – – – – avoid thoughts, feelings or discussions avoid activities, places memory blocks anhedonia (without pleasure) numb alexithymia (emotions unknown) feeling of doom Symptom Categories • Hyperarousal Symptoms – – – – – sleep disturbance anger problems concentration startle response “on guard” hypervigilence Mood Disorders • Major Depressive Disorder • Bipolar I and Bipolar II • Cyclothymia – Hypomania • Dysthymia • Schizoaffective disorder Categories of Personality Disorders • Cluster A – Paranoid – Schizoid – Schizotypal Personality Disorders • • • • Paranoid personality disorder Schizoid personality disorder Schizotypal personality disorder Histrionic personality disorder Categories of Personality Disorders • Cluster B – – – – Histrionic Narcissistic Antisocial Borderline Categories of Personality Disorders • Cluster C – Avoidant – Dependent – Obsessive-compulsive The Clinical Picture in Schizophrenia • Positive symptoms – Delusions: fixed firm beliefs with no basis in reality • Most common are grandiose, persecutory and referential – Hallucinations: disturbances in perception • Can occur in any of the five senses – Most common are auditory and visual The Clinical Picture in Schizophrenia • Formal Thought Disorder (a positive symptom) – Disturbances in speech that reflect underlying problems in cognition or thinking • Most common forms are tangentiality and circumstantiality • Less common are neologisms, word salad and clang associations The Clinical Picture in Schizophrenia • Negative symptoms (Nancy Andreasen) – – – – – Avolition Anhedonia Alogia Flat Affect Asociality The Classic Subtypes of Schizophrenia • • • • Undifferentiated type Catatonic type Disorganized type Paranoid type Graph of HS drug use Substance-Related Disorders Methods of taking substances: 7 sec 20 sec 4 min 30 min inhaling IV snort oral or Intramuscular injection When is addiction addiction? • What is substance use? • What is substance abuse? • What is substance dependence? Where is the line??????? DSM-IV Criteria Substance Abuse leads to impairment or distress one of these within 1 yr: failure to full fill role obligations physically hazardous legal problems persistent social problems Substance Dependence leads to impairment or distress 3 of the following: tolerance withdrawal delirium tremens (DTs) take more than intended persistent desire fail to control use lots of time spent obtaining, using, or recovering from use in place of activities continuing despite physical or psychological problems Solomon’s Opponent Process Theory of Addiction • Basic Premise- People take, abuse and become dependent on drugs because of the effect of these drugs • The Clements Corollary- noone ever becomes addicted to thorazine – A State- the initial pleasant effect – B State-unpleasant effects occurring as a result of drug withdrawal The Clinical Picture of Alcohol Abuse and Dependence • Alcohol’s effects on the brain • Physical effects of chronic alcohol use • Psychosocial effects of abuse and dependence Alcohol (ETOH) Short-term effects: absorbed from the stomach into the blood metabolized by the liver (1 oz/hr) it is a drug acts within brain to: stimulate GABA receptors reduces tension dopamine/serotonin levels pleasurable aspects of intoxication inhibits glutamate receptors diminishes cognitive abilities Long-term effects: reduced food intake ETOH: no nutrient value impairs food digestion results in vitamin deficiency B-complex can lead to brain damage/amnesia kills brain cells leads to loss of gray matter from the temporal lobes Korsakoff’s Syndrome suppresses the immune system Alcohol (ETOH) A “drink”: 1 oz. Spirits = 1 glass wine = 1 beer DWI (Driving while intoxicated) takes approximately 2-4 drinks over one hour lighter weight, empty stomach will require less legal blood alcohol limit (.10%) DUI (Driving under the influence) The CAGE Alcohol Addiction: Treatment Admitting the problem a prerequisite for therapy (video clip) Inpatient Hospital treatment expensive & does not lead to better results may be necessary for safe detoxification Aversion therapy Antabuse - drug that creates nausea uses operant conditioning principles Controlled drinking training Self-Help groups Alcoholics Anonymous