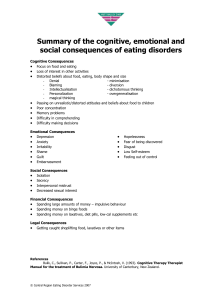
CBT FOR EATING DISORDERS
advertisement

TRANSDIAGNOSTIC CBT FOR EATING DISORDERS “CBT-E” Christopher G Fairburn www.psychiatry.ox.ac.uk/credo WHY LEARN ABOUT CBT-E? • Latest version of the leading evidence-based treatment for eating disorders • Theory-driven • Suitable for a wide range of patients – “transdiagnostic” in its scope – designed for “complex patients” • Highly acceptable to patients • Detailed treatment guide • Shown to be reasonably potent in an inclusive patient sample GUIDE TO CBT-E Fairburn CG. Cognitive Behavior Therapy and Eating Disorders. Guilford Press, New York, 2008 Go to www.psychiatry.ox.ac.uk/credo – obtain further information about CBT-E – obtain the materials needed to practise CBT-E – obtain copies of EDE-16.0D, EDE-Q6.0 and CIA 3.0 EATING DISORDERS Anorexia nervosa Bulimia nervosa Eating disorder NOS AN ED-NOS Comparable in severity to BN Three subgroups: • subthreshold cases of AN and BN • “mixed states” • binge eating disorder BN Leading treatment is guided CB self-help BED No empirically supported treatment AN CBT leading empiricallysupported treatment: ED-NOS Just one treatment study BN • but only 40% to 50% of those who complete CBT-BN make a full and lasting recovery TWO PROBLEMS 1. No evidence-based treatment for – – AN ED-NOS 2. CBT-BN not sufficiently potent “ENHANCED” CBT (CBT-E) CBT-E is designed to address both these problems. Hence ..... 1. It is transdiagnostic in its scope 2. It is designed to be more potent than CBT-BN THE “TRANSDIAGNOSTIC” VIEW What is most striking about AN, BN and ED-NOS is: – 1. How much they have in common, not what distinguishes them ... they share the same distinctive psychopathology – 2. The phenomenon of diagnostic migration THE “TRANSDIAGNOSTIC” VIEW CBT-E is designed to address these mechanisms ..... ...... it is a treatment for eating disorder psychopathology, not a treatment for a DSM-IV diagnosis MAKING TREATMENT MORE POTENT ... CBT-E is designed to be better than CBT-BN at ... • Preparing patients for treatment • Individualising treatment (“bespoke”) • Engaging and retaining patients • Achieving early change • Addressing the over-evaluation of shape and weight and its expressions (e.g., body checking and avoidance, feeling fat, etc) • (Towards the end of treatment) helping patients identify and manipulate their eating disorder “mindset” to minimise the risk of relapse • (In the “broad form” of CBT-E) addressing certain difficulties that obstruct change in subsets of patients; namely, mood intolerance, clinical perfectionism, core low self-esteem, or marked interpersonal difficulties (Fairburn, 2008) VARIOUS VERSIONS OF CBT-E Two forms • Focused: Core default version of the treatment • Broad: Includes additional modules to address broader “external” maintaining mechanisms: mood intolerance, clinical perfectionism, low self-esteem and major interpersonal problems Two intensities • 20-session version for patients with a BMI >17.5 • 40-session version for patients with a BMI <17.5 Versions for different patient groups • Adult outpatient version (Fairburn et al, 2008) • Younger patients’ version (Cooper and Stewart, 2008) • Intensive versions (inpatient, day patient and intensive outpatient versions), and a group version (Dalle Grave, Bohn, Hawker and Fairburn, 2008) PREPARING PATIENTS FOR CBT-E • Provide a description of the treatment and address patients’ concerns. A suitable handout available from www.psychiatry.ox.ac.uk/credo • Advise patients that it is important to make the best possible use of treatment • Give detailed consideration as to when it would be best for CBT-E to start. “False starts” should be avoided if at all possible • Address potential barriers to change in advance: • clinical depression • significant substance abuse • major distracting life problems and competing commitments DEPRESSION Clinical observations 1. Antidepressant medication is remarkably effective in patients with “primary depressive features” – – – – – – – – decreased drive thoughts about death and dying heightened social withdrawal personal neglect marked hopelessness suicidal thoughts and acts tearfulness pathological guilt DEPRESSION Clinical observations (cont) 2. Such patients may have other characteristics of note – – – 3. premorbid depression a late-onset eating disorder intensification of depressive features in the absence of change in the eating disorder Higher than usual antidepressant doses are often required – – fluoxetine (40mg to 100mg) few side effects DEPRESSION Clinical observations (cont) 4. Resolution of the depressive features facilitates subsequent treatment Resolution of the depressive features may, or may not, result in a change in the eating disorder 5. – – 6. in AN, dietary restraint may intensify in BN, urge to binge may decrease Follow-up suggests that some patients are prone to recurrent depressive episodes – these may trigger recurrences of the eating disorder OVERVIEW OF CBT-E Stage One • “Start well” (establish the foundations of treatment; achieve early change) Stage Two • Review progress; identify emerging barriers to change; design Stage Three Stage Three • Address the main maintaining mechanisms Stage Four • “End well” (maintain the changes obtained; minimise the risk of relapse) STAGE ONE - STARTING WELL 1. 2. 3. 4. 5. 6. 7. 8. 9. Engage the patient in treatment and change Assess the nature and severity of the psychopathology present Jointly create a personalised formulation Explain what treatment will involve Establish real-time self-monitoring Initiate in-session collaborative weighing Provide psychoeducation Establish a pattern of regular eating See significant others THE FORMULATION Personalised visual representation of the processes that appear to be maintaining the eating disorder Rationale • • • • • Begins to distance patients from their problem (decentering) Starts the process of helping patients step back from their eating disorder and try to understand it Can be highly engaging Conveys the notion that eating disorders are a self-maintaining system Informs treatment BULIMIA NERVOSA Over-evaluation of shape and weight and their control c d a Strict dieting; non-compensatory weight-control behavior b Events and associated mood change e Binge eating f Compensatory vomiting/laxative misuse Available as a pdf from www.psychiatry.ox.ac.uk/credo ANOREXIA NERVOSA Over-evaluation of shape and weight and their control Strict dieting; non-compensatory weight-control behaviour Low weight with secondary effects • • • • preoccupation with eating social withdrawal heightened obsessionality heightened fullness Available as a pdf from www.psychiatry.ox.ac.uk/credo COMPOSITE TEMPLATE FORMULATION Over-evaluation of shape and weight and their control Strict dieting; noncompensatory weight-control behaviour Events and associated mood change Binge eating Significantly low weight Compensatory vomiting/laxative misuse Available as a pdf from www.psychiatry.ox.ac.uk/credo EXAMPLE OF ED-NOS Feel really bad about my weight and the way I look Diet; exercise a lot Feel unhappy Occasional binges Low weight? Make myself sick Available as a pdf from www.psychiatry.ox.ac.uk/credo BINGE EATING DISORDER Dissatisfaction with shape and weight and their control Intermittent dieting Events and associated mood change Binge eating THE FORMULATION Procedure • • • • • Drawn out, using the patient’s terms and experiences, starting with something that the patient wants to change Transdiagnostic, but derived from a common template Created jointly; handwritten Provisional; modified as the therapist and patient get a better understanding of the problem Both the therapist and patient keep a copy; in each session, it is on the table SELF-MONITORING Rationale • • Helps patients distance themselves from the processes that are maintaining their eating disorder, and thereby begin to recognise and question them Highlights key behaviour, feelings and thoughts, and the context in which they occur – – makes experiences that seems automatic and out of control more amenable to change must be in “real time” SELF-MONITORING Procedure • • • • • • Discuss practicalities and likely difficulties Stress that it must be “prospective” Provide written instructions and a completed example Form should be simple to complete Reviewing the monitoring records is a crucial part of each session Pay close attention to the process of monitoring in session #1 and respond with perplexity if the patient has not monitored COLLABORATIVE WEIGHING Rationale • Patients with eating disorders are unusual in their frequency of weighing – – • frequent weighing encourages concern about inconsequential changes in weight, and thereby maintains dieting avoidance of weighing is as problematic Knowledge of weight is a necessary part of treatment – – – – permits examination of the relationship between eating and weight facilitates change in eating habits necessary for addressing any associated weight problem one aspect of the addressing of the over-evaluation of weight COLLABORATIVE WEIGHING Procedure • No weighing at home (but transfer to at-home weighing late in treatment) but patient and therapist weighing the patient at the beginning of each (weekly) session – – – joint plotting of a weight graph repeated examination of trends over the preceding four readings continual reinforcement of “One can’t interpret a single reading” EDUCATION Rationale • Reduces stigma, corrects myths, informs about important maintaining processes, educates about health risks Procedure • • • • Guided reading Overcoming Binge Eating” (Fairburn, 1995) – all patients (even those who do not binge eat) – chapters 1, 4 and 5 Provide additional information about “starvation” for those who are significantly underweight (available as a pdf from www.psychiatry.ox.ac.uk/credo) Reading set as graded homework with reviews at subsequent session(s) REGULAR EATING Key intervention for all patients (including underweight ones) Rationale • • • • • Foundation upon which other changes in eating are built Gives structure to the patient’s eating habits (and day) Provides meals and snacks which can then be modified Addresses one form of dieting Displaces binge eating Procedure • • • Help patients eat at regular intervals through the day ..... ..... without eating in the gaps ..... what they eat does not matter at this stage SIGNIFICANT OTHERS Rationale • • • See “significant others” if this is likely to facilitate treatment and the patient is willing Usually the significant others are people who influence the patient’s eating Aim is to create the optimal environment for the patient to change Procedure • Typically comprises up to three 30-minute sessions immediately after a routine one; preparation is important STAGE TWO Whilst continuing with the strategies and procedures introduced in Stage One ... 1. Review progress and compliance with treatment 2. Identify emerging barriers to change 3. Review the formulation 4. Decide whether to use the “broad” form of CBT-E – 5. clinical perfectionism, core low self-esteem, major interpersonal problems Design Stage Three STAGE THREE Whilst continuing with the strategies and procedures introduced in Stage One, address the main maintaining mechanisms operating in the individual patient’s case ... 1. Over-evaluation of shape and weight 2. Over-evaluation of control over eating 3. Dietary restraint 4. Dietary restriction 5. Being underweight 6. Event-related changes in eating ADDRESSING THE OVER-EVALUATION OF SHAPE OR WEIGHT The “core psychopathology” of eating disorders is the over-evaluation of shape and weight • self-worth is judged largely or exclusively in terms of shape and weight and the ability to control them • other modes of self-evaluation are marginalised • most other features appear to be secondary to the core psychopathology • dieting • repeated body checking and/or body avoidance • pronounced “feeling fat” ADDRESSING THE OVER-EVALUATION OF SHAPE OR WEIGHT Overview 1. Prepare the patient for change i. Educate about self-evaluation ii. Assess the patient’s scheme for self-evaluation and its expressions iii. Expand the formulation Family Work Shape, weight and eating Other Friends Sport Music Family Work Shape, weight and eating Other ADDRESSING THE OVER-EVALUATION OF SHAPE OR WEIGHT (cont) Expand the formulation Over-evaluation of shape and weight and their control Dietary restraint Shape and weight checking and/or avoidance Preoccupation with thoughts about shape and weight Mislabelling adverse states as “feeling fat” Marginalisation of other areas of life ADDRESSING THE OVER-EVALUATION OF SHAPE OR WEIGHT 2. Address the over-evaluation using two strategies: Develop new domains for self-evaluation Reduce the importance of shape and weight ADDRESSING THE OVER-EVALUATION OF SHAPE OR WEIGHT Develop new domains for self-evaluation – encourage patients to identify and engage in (neglected) interests and activities, especially those of a social nature ADDRESSING THE OVER-EVALUATION OF SHAPE OR WEIGHT Overview 1. Prepare for change 2. Address the over-evaluation using two strategies: • Develop marginalised self-evaluative domains • Addressing the expressions of the over-evaluation • body checking and avoidance • “feeling fat” ADDRESSING THE OVER-EVALUATION OF SHAPE OR WEIGHT (cont) Shape checking • Identify the various forms of shape checking • often patients are not aware of them • self-monitoring for 24 hours on two days ADDRESSING THE OVER-EVALUATION OF SHAPE OR WEIGHT (cont) Shape checking • Identify the various forms of shape checking • Categorise them – those best stopped (e.g., measuring dimensions) – those best reduced in frequency and/or modified • Progressively address • Takes many successive sessions (one item on session agenda) • Always address mirror use ADDRESSING THE OVER-EVALUATION OF SHAPE OR WEIGHT (cont) Reflections on mirrors • How do we know what we look like? • Should we believe what we see in the mirror? – things aren’t what they seem – what we “see” in mirrors depends to a large extent upon how we look – scrutiny is prone to result in magnification (c.f., spider phobias) – scrutiny creates and maintains dissatisfaction • “If you look for fatness you will find it” – contrast with incidental reflections (e.g., in shop windows) ADDRESSING THE OVER-EVALUATION OF SHAPE OR WEIGHT (cont) Mirror use • Always assess patients’ mirror use • Educate about mirrors – consider when it is appropriate to look in a mirror • Encourage patients to think first before using a mirror – what are they trying to find out? – can they find this out? – is there a risk that they will get “bad” information? • Discuss how to avoid magnification ADDRESSING THE OVER-EVALUATION OF SHAPE OR WEIGHT (cont) Comparisons with others • Frequent • Conclusions drawn are highly salient • Biased – subjects of the comparison (slim) – method of appraisal (cursory) Strategy • Identify the phenomenon • Educate • Reduce frequency, experiment with bias (subjects & methods) ADDRESSING THE OVER-EVALUATION OF SHAPE OR WEIGHT (cont) Body avoidance • Avoidance is as problematic as repeated checking and scrutiny • Identify the various forms of avoidance (NB: may co-occur with checking) • Educate • Progressively encourage “exposure” (using behavioural experiments) • Include the evaluation of other people’s bodies • Takes many successive sessions (one item on agenda) “Feelings of fatness” Actual weight Time Available as a pdf from www.psychiatry.ox.ac.uk/credo ADDRESSING THE OVER-EVALUATION OF SHAPE OR WEIGHT (cont) “Feeling fat” • • • Phenomenon little studied or written about Fluctuates in intensity Either: – – an expression of an acute increase in body dissatisfaction the result of mislabelling certain physical or emotional states Strategy • Identify in real time the triggers of (intense) feelings of fatness • Examine the nature of the triggers • Help patients ... • • ask “What else am I feeling just now?” whenever they feel fat address the triggers directly ADDRESSING DIETARY RESTRAINT Strict dieting “Restraint” “Restriction” (attempted under-eating) (actual under-eating) ADDRESSING DIETARY RESTRAINT • Remind patients that (for them) dietary restraint is a problem, not a solution – • e.g., highlight any difficulty/inability eating with others (CIA) Identify the main forms of restraint – delayed eating • already addressed – avoidance of specific foods ADDRESSING DIETARY RESTRAINT Food avoidance • • • Identify avoided foods Categorise them Systematically introduce (as behavioural experiments) IDENTIFY AND CHALLENGE DIETARY RULES Identify other dietary rules and rituals: • Not eating more than 600 kcals daily • Not eating before 6.00 pm • Not eating in front of others • Eating less than others present • Not eating food of unknown composition ADDRESSING RESIDUAL BINGES • • Introduction of a pattern of regular eating displaces most binge eating Identify mechanisms responsible for each remaining binge Binge Analysis Breaking a dietary rule • ……………………… Being disinhibited (e.g., alcohol) • ……………………… Under-eating Binge eating • ……………………… Adverse event or mood • ……………………… Lessons to learn: • ……………………... Available as a pdf from www.psychiatry.ox.ac.uk/credo STAGE THREE Completing Stage Three 1. 2. Review the origins of the eating problem (“historical review”) Help patients learn to control their eating disorder “mindset” ORIGINS OF THE EATING PROBLEM Historical review Rationale - Normalising - Encourages further distancing and awareness of the eating disorder “mindset” - Facilitates discussion of the “function” of the eating disorder in the past and at present - Enhances understanding of the eating disorder Time period Events and circumstances (that might have sensitized me to my shape, weight and eating) Before onset of eating problem (up to age 16) Mother very anxious about eating throughout my childhood A bit overweight aged 9 Always have been on the tall side and a bit clumsy (have felt too "big") Friend developed anorexia; slightly jealous The 12 months before onset (when I was 16) Moved to new city and house New school Unhappy; no friends The 12 months after onset (when I was 17) Started to cut back on my eating Felt good and in control Fights with my mum Lost weight rapidly for a while Since then (17 to 26) Started purging (18) Binge eating (18/19) Went to college (19) Regained weight (19); out of control; awful Eating problem just as it is now (20 to present) Dropped out of college (23) Psychotherapy and antidepressants (24) Fairburn et al (2008) MINDSETS Introduce the notion of mindsets once patients have alternating psychological states (near the end of treatment) Educate (DVD analogy) • all-embracing cognitive-emotional systems • we all have them • may be dysfunctional • create their own reality (they “filter” experience) • self-perpetuating MINDSETS One can influence mindsets in two ways: i. By addressing their content • using conventional CBT procedures MINDSETS ii. By influencing their “playing” • decreasing the chances it is triggered • • by spotting it coming into place • • real-time awareness of potential triggers; inoculation against them early warning signs (“relapse signatures”) by displacing it • behaving healthily (“doing the right thing”) • plus potent distraction STAGE FOUR - ENDING WELL 1. Maintain the changes obtained • • Identify what problems remain Jointly devise a specific plan for maintaining progress [Template plan available for editing from www.psychiatry.ox.ac.uk/credo] STAGE FOUR - ENDING WELL 2. Minimise the risk of relapse (in the long-term) • • • Ensure that the patient has realistic expectations – Achilles heel (the DVD still exists) – danger of viewing a “lapse” as a “relapse” Identify future “at risk” times – if weight gain; if dieting; if under stress Devise a plan for dealing with setbacks – detect early – deal with them promptly i. ii. address the eating problem; do the right thing address the trigger [Template plan available for editing from www.psychiatry.ox.ac.uk/credo] CBT-E Strategies for patients who are underweight CBT-E 1. Start well. Engage the patient in treatment and the prospect of change • carefully consider when best to start treatment 150 • be engaging, positive, supportive, interested in patient as a person 140 130 BMI 20.0 120 110 100 90 80 0 2 4 6 8 10 12 14 16 18 20 22 24 26 28 30 32 34 36 38 40 Weeks (Fairburn, Cooper, Shafran, Bohn, Hawker, Murphy and Straebler, 2008) CBT-E 1. Start well. Engage the patient in treatment and the prospect of change 2. Educate about the psychobiological effects of under-eating and being underweight, and create a personalised formulation • personalised education (based on handout) • personalised formulation (derived from CBT-E’s transdiagnostic template formulation) 150 140 130 BMI 20.0 120 110 100 90 80 0 2 4 6 8 10 12 14 16 18 20 22 24 26 28 30 32 34 36 38 40 Weeks (Fairburn, Cooper, Shafran, Bohn, Hawker, Murphy and Straebler, 2008) EDUCATION • • 1. Psychological effects of maintaining a very low weight Cognitive effects – – – – • inward-looking preoccupied with food and eating difficulty concentrating inflexible thinking Effects on mood – – – low mood lability of mood irritability EDUCATION • Heightened obsessionality – – – • rigidity of behaviour (e.g., fixed routines) obsessional behaviour (e.g., ritualistic eating) indecisiveness and procrastination Social effects – – – withdrawal loss of interest in the outside world loss of interest in sex EDUCATION • 2. Subjective physical effects of maintaining a very low weight • • • • feeling cold sleeping poorly feeling full after eating little impaired taste (need to use lots of condiments) • • 3. Medical information • Effects on bones, growth, fertility, etc EDUCATION • Implications • 1. Many features that the patient is experiencing are non-specific effects of starvation • feeling cold, sleeping poorly, feeling full • being obsessive and inflexible, difficulty concentrating • being infertile, having weak bones – some are likely to maintain the eating disorder – features of starvation mask the patient’s true personality – reversed by weight regain; weight gain therefore a necessary part of treatment EDUCATION • 2. Other features are not due to starvation • extreme concerns about shape and weight • the need to feel in “control” – some of these features are responsible for the initiation and maintenance of the starvation – treatment must also be directed at these features ANOREXIA NERVOSA Over-evaluation of shape and weight and their control Strict dieting; non-compensatory weight-control behaviour Low weight with secondary effects • • • • preoccupation with eating social withdrawal heightened obsessionality heightened fullness Available as a pdf from www.psychiatry.ox.ac.uk/credo CBT-E 1. Start well. Engage the patient in treatment and the prospect of change 2. Educate about the psychobiological effects of under-eating and being underweight, and create a personalised formulation 3. Establish a pattern of regular eating 4. Discuss pros and cons of change 5. Initiate and then maintain weight regain 150 140 130 BMI 20.0 120 110 100 90 80 0 2 4 6 8 10 12 14 16 18 20 22 24 26 28 30 32 34 36 38 40 Weeks (Fairburn, Cooper, Shafran, Bohn, Hawker, Murphy and Straebler, 2008) How I feel now Reasons to stay as I am It makes me feel in control and special I get attention from others I will not get ‘fat’ I am good at it It makes me feel strong It shows I have will-power It is familiar and feels safe I have an excuse for things I don’t have to have periods I am not hassled by men If I change: - I won’t be able to stop eating - my weight will shoot up - my stomach will stick out - my thighs will get fatter If I change people will think that: - I am weak and greedy - I have given in - I am getting fat Thinking five years ahead ... Reasons to change Reasons to stay as I am Reasons to change I will get rid of my starvation symptoms: - thinking about food and eating all the time - feeling so cold - not sleeping properly - feeling faint I will feel healthier I will be healthier I will be able to think more clearly I will have more time I will be able to think about other things I will be less obsessive, and more flexible and spontaneous My life will have a broader focus I will be happier and have more fun I will be able to go out with others and get on with people better I will discover who I really am It makes me feel in control and special I will not get ‘fat’ It is familiar and feels safe If I change: - I won’t be able to stop eating - my weight will shoot up - my stomach will stick out - my thighs will get fatter If I change people will think that: - I am weak and greedy - I have given in - I am getting fat I want to be a success at work I want a long term relationship I want a family I want to be a positive role model for my children I want to go on holiday and be spontaneous I want to be in good health I don’t want to still have starvation symptoms or any other effects of the ED I want to be in ‘true’ control of my eating I don’t want to waste my life I want to achieve things I don’t want to be chronically ill 170 160 BMI 25.0 (157lbs) 150 Healthy weight 140 Weight (lbs) 130 BMI 20.0 (126lbs) 120 110 100 0 2 4 6 8 10 12 14 16 18 20 22 24 26 28 30 32 34 36 38 40 Weeks CBT-E 1. Start well. Engage the patient in treatment and the prospect of change 2. Educate about the psychobiological effects of under-eating and being underweight, and create a personalised formulation 3. Establish a pattern of regular eating 4. Discuss pros and cons of change 5. Initiate and then maintain weight regain 150 140 130 BMI 20.0 120 110 100 • take the plunge • educate about the physiology of weight regain • let patients try it their way • help patients maintain an energy excess of 500kcals per day • offer the option of high-energy drinks 90 80 0 2 4 6 8 10 12 14 16 18 20 22 24 26 28 30 32 34 36 38 40 Weeks (Fairburn, Cooper, Shafran, Bohn, Hawker, Murphy and Straebler, 2008) CBT-E 1. Start well. Engage the patient in treatment and the prospect of change 2. Educate about the psychobiological effects of under-eating and being underweight, and create a personalised formulation 3. Establish a pattern of regular eating 4. Discuss pros and cons of change 5. Initiate and then maintain weight regain 6. Address other psychopathology at the same time 7. Practise weight maintenance and end well • ensure that progress is maintained • minimise the risk of relapse 150 140 130 BMI 20.0 120 110 100 90 80 0 2 4 6 8 10 12 14 16 18 20 22 24 26 28 30 32 34 36 38 40 Weeks (Fairburn, Cooper, Shafran, Bohn, Hawker, Murphy and Straebler, 2008) Over-evaluation of shape and weight and their control • body checking and avoidance • feeling fat • marginalisation of other areas of life Strict dieting; non-compensatory weight-control behaviour • dietary restraint and restriction • dietary rules • over-exercising Low weight with secondary effects CBT-E Broad version EXTENDED THEORY (Fairburn et al, 2003) • • Certain “external” maintaining mechanisms operate in subgroups of patients and these are barriers to change Four sets of mechanisms appear to be especially important – – – – • • mood intolerance clinical perfectionism core low self-esteem interpersonal difficulties Predicted that the successful addressing of these mechanisms should improve outcome The “broad” form of CBT-E is based on this theory MOOD INTOLERANCE • There is a subgroup of patients with “mood intolerance” – exceptionally sensitive to intense mood states – usually adverse mood states (e.g., anger, anxiety) – unable to accept and deal appropriately with these states MOOD INTOLERANCE (cont) • Respond “dysfunctional mood modulatory behaviour” which reduces awareness of the mood state and neutralises it, but at a personal cost – self-injury (e.g., cutting or burning their skin) – taking psychoactive substances (e.g., alcohol or tranquillisers) – binge eating, vomiting or exercising intensely (which may also become habitual means of mood modulation) MOOD INTOLERANCE (cont) • Not clear whether these patients actually experience unusually intense mood states or are unduly sensitive to them • Cognitive processes contribute (e.g., “I can’t stand feeling like this”) and can amplify the initial mood state MOOD INTOLERANCE (cont) Treatment • Existing CBT treatment procedures are often not sufficient for these patients’ needs • Treatment strategies and procedures have been developed that are relevant to mood intolerance: – elements of dialectical behaviour therapy (Linehan, 1993) – enhancement of metacognitive awareness ADDRESSING MOOD INTOLERANCE 1. Analyse in detail a recent example in session • recreate the exact sequence – – – – – – triggering events any mood change associated cognitions behavioural response immediate effect later appraisal 2. Start to monitor in detail the relevant phenomena • ask the patient to monitor closely the relevant behaviour and its antecedents and consequences ADDRESSING MOOD INTOLERANCE (cont) Adverse event Pressure at work Deterioration in mood Tension Dysfunctional behaviour Binge eating and/or cutting Immediate improvement in mood Release of tension Later negative appraisal “Binge eating like this is hopeless. I have no will-power” ADDRESSING MOOD INTOLERANCE (cont) 3. Prospectively analyse future examples • ask the patient to analyse in real time the occurrence (or incipient occurrence) of future episodes of mood intolerance • requires very careful “in the moment” recording of circumstances, thoughts and feelings • patients find this frustrating • rationale: – slows down and distances the patient from the phenomenon – highlights points in the sequence when alternative courses of action are possible ADDRESSING MOOD INTOLERANCE (cont) 4. Address using the procedures that seem most pertinent • • • • • • range of options available important that patients intervene early one success breeds further successes real-time monitoring has an impact in its own right choose those procedures that seem most applicable do not forget the value of simple interventions (e.g., putting barriers in the way of engaging in DMMB) • do not overload patients (principle of parsimony) CLINICAL PERFECTIONISM Over-evaluation of striving to achieve, and achieving, personally demanding standards despite adverse consequences • Form of psychopathology equivalent to the “core psychopathology” of eating disorders (i.e., it is also a dysfunctional system for self-evaluation) • (Shafran R, Cooper Z, Fairburn CG. Clinical perfectionism: A cognitive-behavioural analysis. Behaviour Research and Therapy 2002; 40: 773-791) CLINICAL PERFECTIONISM (cont) • When clinical perfectionism and an eating disorder co-exist their psychopathology overlaps – perfectionist standards for controlling eating, shape and weight – in addition to perfectionist standards for other valued domains of life (e.g., performance at work, sport, music, etc) Over-evaluation of shape and weight and their control Strict dieting; noncompensatory weight-control behaviour Events and associated mood change Binge eating Compensatory vomiting/laxative misuse Significantly low weight Over-evaluation of achieving and achievement Pursuit of personally demanding standards in valued areas of life e.g., work, sport, friendships, etc Available as a pdf from www.psychiatry.ox.ac.uk/credo CLINICAL PERFECTIONISM (cont) Treatment • Cognitive behavioural analysis of clinical perfectionism has clear implications for treatment – i.e., the CBT-E strategy (for addressing the over-evaluation of eating, shape and weight) may also be applied to clinical perfectionism Over-evaluation of achieving and achievement Rigorous pursuit of personally demanding standards and/or avoidance of tests of performance Preoccupation with thoughts about performance Performancechecking with selective attention to deficiencies in performance Marginalization of other areas of life Re-setting standards if goals are met Available as a pdf from www.psychiatry.ox.ac.uk/credo “CORE” LOW SELF-ESTEEM • Many patients with eating disorders are highly self-critical – due to failure to meet their goals (e.g., perfect control over eating) – generally lessens with successful treatment • Subgroup that has a more global negative view of themselves - “core low self-esteem" – unconditional and pervasive negative view of themselves – part of their permanent identity – leads them to make negative judgements about themselves that are autonomous and independent of performance “CORE” LOW SELF-ESTEEM (cont) • Generally longstanding – antecedent risk factor for developing AN and BN (like perfectionism) • Obstructs change (relatively consistent predictor of poor response to CBT-BN) – creates hopelessness about the capacity to change – encourages particularly determined pursuit of valued goals • Self-perpetuating state – pronounced negative processing biases coupled with over-generalisation – results in patients being prone to see themselves as repeatedly failing, and these failures being viewed as confirmation that they are failures as people CORE LOW SELF-ESTEEM (cont) Treatment • Are many well-described CBT strategies and procedures available (e.g., Fennell, 1998) • Change is greatly facilitated by concurrent change in other areas (i.e., change in the eating disorder; enhanced interpersonal functioning) ADDRESSING CORE LOW SELF-ESTEEM Reading • Fennell MJV (1998). Low self-esteem. In Treating Complex Cases: The Cognitive Behavioural Therapy Approach (eds N Tarrier, A Wells, G Haddock). Wiley, Chichester • Fennell M (1999). Overcoming Low Self-esteem. Robinson, London INTERPERSONAL DIFFICULTIES • Well-recognised that many patients with eating disorders have impaired interpersonal functioning • Their significance has come to the fore with the well-replicated finding that an exclusively interpersonal treatment (IPT) is a relatively effective treatment for BN (Fairburn et al, 1993; Agras et al, 2000) INTERPERSONAL DIFFICULTIES (cont) Treatment • • CBT-E addresses interpersonal functioning (when relevant) with there being three interpersonal goals: • to resolve interpersonal problems • to enhance general interpersonal functioning • to address developmental issues Achieved using an embedded interpersonal module that employs IPT strategies and procedures