Psychopathology & treatment
advertisement

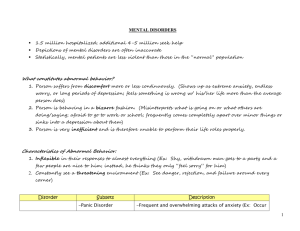
1 GENERAL PSYCHOLOGY LECTURE 13 PSYCHOPATHOLOGY &TREATMENT Visiting Assistant PROFESSOR YEE-SAN TEOH Department of Psychology National Taiwan University Unless noted, the course materials are licensed under Creative Commons AttributionNonCommercial-ShareAlike 3.0 Taiwan (CC BY-NC-SA 3.0) PSYCHOPATHOLOGY & TREATMENT Defining Mental Disorders • Mental disorders are currently diagnosed using the diagnostic manual of the American Psychiatric Association. • Diagnostic & Statistical Manual of Mental Disorders (DSM-IV-TR). Mental Disorders (DSM-IV-TR) • Behavioral or psychological syndrome or pattern that occurs in a person that is associated with present: Distress (e.g. painful symptom), or Disability – impairment in one or more important areas of functioning, or Significantly increased risk of harm (suffering, death, pain, disability, or an important loss of freedom) Mental Disorders (DSM-IV-TR) • The syndrome or pattern must: Not be merely an expectable and culturally sanctioned response to a particular event. Currently be considered a manifestation of the behavioral, psychological, or biological dysfunction in the individual. Prevalence of Mental Disorders • Point prevalence – how many people in a given population have a given disorder at a particular point in time. • Lifetime prevalence – how many people in a certain population will have the disorder at any point in their lives. i. 46% of the U.S. population will experience at least one mental disorder during their lifetimes. ii. Anxiety disorders are the most common disorders (lifetime prevalence rate of 29%). ASSESSING MENTAL DISORDERS Clinical Assessment Clinical interviews Self-report measures Projective tests Lab tests (e.g. neuroimaging, blood) Clinical Interview • Clinician asks patient to describe her problems/concerns. • Close attention is paid to the patient’s report, looking for consistencies and discrepancies in: (i) Symptoms: what is reported by the patient about his physical or mental condition (e.g. hearing voices) (ii) Signs: what is observed by the clinician about a patient’s physical or mental condition (e.g. inattention) Self-Report Measures • Asking participants questions, e.g. questionnaire. Beck Depression Inventory (BDI) • Targets people’s feelings of depression. Projective Tests • Unstructured personality tests • Use relatively ambiguous stimuli to elicit responses that are unguarded and authentic. • E.g. Unconscious wishes & conflicts that cannot be revealed via direct testing. Thematic Apperception Test (TAT) • Person is shown a set of pictures and asked to make up a story about each. • Responses are seen as revealing implicit or otherwise hidden motives. The DSM-IV-TR • Sets out specific criteria - particular duration for the symptoms or a certain frequency for each disorder. • Contains 5 dimensions of functioning. • Includes disorders that seem to appear only in some cultures, e.g. i. Dhat (India): term used to refer to severe anxiety abt the discharge of semen. ii. Ghost sickness (Native Americans): preoccupation with death 5 Axes of DSM-IV-TR I • Clinical syndromes, e.g. depression, eating disorders, drug dependence II • 2 broad sets of difficulties – mental retardation & personality disorder III • General medical conditions that may contribute to a person’s psychological functioning IV V • Social or environmental problems (e.g. family) • Global assessment – how well person is coping with her overall situation. ANXIETY DISORDERS Prevalence & Symptoms • Lifetime prevalence is 29% • More common in women than in men. • Main symptom = feeling of intense anxiety. • Person with anxiety disorder will often take steps (usually disruptive to their lives & unsuccessful) to deal with anxiety Anxiety Disorder I: Phobias • Intense & irrational fear. • Coupled with great efforts to avoid the feared object or situation. • Specific & social phobias. Specific phobias - Characteristics • Intense & irrational fear directed at a particular object – person probably knows it irrational but cannot help it. • Lifetime prevalence of around 13%. • Gender ratio of 2:1 (female:male) • Some fears are more common than others (e.g. snakes vs specific numbers). Specific phobias - Examples Acrophobia (high places) Claustrophobia (enclosed places) Ochlophobia (crowds) Mysophobia (germs) Triskaidekaphobia (number 13) Specific phobias – Avoidance strategies • Developing strategies for avoiding the phobic object. • Phobias often expand in scope so that the person may avoid more and more objects or places. Social Phobia - Characteristics • Also referred to as social anxiety disorder. • Fear of embarrassment or humiliation causes people to avoid situations that might expose them to public scrutiny. • Intensely afraid of being watched and judged by others. • Concerned about negative evaluations as well as positive ones. Social Phobia - Characteristics • Lifetime prevalence of around 13%. • Equal prevalence for men & women. • Typically emerges in childhood or adolescence. • May be accompanied by other anxiety disorders or depression. Social Phobia - Examples • Fears may be limited to one type of situation: - Speaking in front of others - Writing in front of others - Eating in front of others • Fears can also be generalized to many different situations. Social Phobia – Avoidance Strategies • Avoid situations in which they must expose themselves to public scrutiny. E.g. Avoid public speaking or performing because they think others will think they are stupid. • When forced into unwanted situations – may use alcohol or drugs – substance abuse or dependence a real risk. STRESS DISORDERS Stress Disorders • A category of anxiety disorders triggered abruptly by an identifiable or horrific event. • E.g. 911 incident, war, 921 earthquake, Japan Tsunami • E.g. child abuse, witnessing a violent crime, rape, physical assault. Posttraumatic Stress Disorder (PTSD) • Lifetime prevalence of 7%, more likely in women. 5 core components (DSM-IV-TR): 1. Must experience a traumatic event that qualifies as a serious traumatic stressor, possibly one that was either objectively or subjectively related to threats of life or physical integrity. 2-4. Three symptoms clusters of reexperiencing, avoidance/numbing, and hyperarousal. - Person must have at least: i. 1 reexperiencing symptom (e.g. recurrent & distressing memories or thoughts of the event, physiological reactivity to trauma reminders) ii. 3 avoidance symptoms (e.g. efforts to avoid thoughts, feelings, or talking about the traumatic event; avoiding activities, places, people, or situations that serve as trauma reminders) iii. 2 hyperarousal symptoms (e.g. difficulty falling or staying asleep, irritability, temper outbursts) 5. Symptoms cluster must be present for at least a month and must cause functional impairment in social, school, family, health, or another important area of daily living. ROOTS OF ANXIETY DISORDERS Comorbidity • Having one of the anxiety disorders increases the likelihood of having another anxiety disorder as well. • More than ½ the people with one anxiety disorder will at some point also have some other anxiety disorder.. Genetic risk factors • The probability that one member of a twin pair will have an anxiety disorder if the other twin has it is much higher for identical than fraternal twins. • Genes do not directly ‘cause’ the anxiety disorder. • Disorder will emerge only if the person with the genetic vulnerability is exposed to some sort of stressor. Brain Bases • Phobias – brain regions involved in fear learning especially active. • PTSD – less brain activation in prefrontal regions assoc with emotional regulation. Psychological Risk Factors • Psychological maltreatment of a child. • Experiences that condition a person to the phobic object. • Learning through observation of fear demonstrated by someone else. • Development of PTSD is affected by: i. Severity of trauma ii. Level of social support available to person. iii. Person’s genetic pattern (x5 more likely if parent has had it). MOOD DISORDERS Mood Disorders • Also called affective disorders. • Changes in mood (disturbance in positive & negative mood) and motivation. • Emotional and energetic extremes. • 2 Types: a. Depression b. Bipolar disorder Depression • Unipolar – at one extreme – depressed. • Depressed mood and/or loss of pleasure. • Lifetime prevalence of 7-12% for men; 20-25% for women • Higher prevalence in women – repetitively turning emotional difficulties over and over in their minds. Symptoms of Depression Centers on feelings of sadness, hopelessness, & broad apathy about life. Loses interests in eating, hobbies, sex, almost everything. Depressed feelings lasting at least 2 weeks & accompanied by other symptoms, such as insomnia & feelings of worthlessness. Many also experience anxiety Symptoms of Depression 20% of people have psychotic delusions – unshakable beliefs. E.g. hearing voices aboutt punishment. Cognitive Deficits – disrupted attention & working memory. Physical Manifestations – loss of appetite, weight loss, weakness, fatigue, poor bowel functioning, sleep disorders, loss of interest in sex. Age of Onset of Depression • Most commonly begins in adolescence & continues through middle adulthood. • But can emerge in the elderly & children. • Some symptoms of depression in adolescents are expressed in teenage form: - Despair – substance abuse - Apathy aboutt life – number of classes missed - Irritability – aggression & defiance ROOTS OF MOOD DISORDERS Genetic Factors • Concordance rate is roughly 2 times higher in identical twins than in fraternal twins. • Separate inheritance pathways for unipolar & bipolar depression. Brain Bases • 3 neurotransmitters seem critical for mood disorders. Norepinephrine ii. Dopamine iii. Serotonin i. • Many antidepressant medications work by altering the availability of these chemicals at the synapse. • Symptom improvements do not usually appear until a few weeks later. Brain Bases • Brain imaging have shown that… • Severe depression is associated with increased brain activation in a limbic system region. - Inducing sadness in healthy participants leads to increased activation in this brain region. - When depression is successfully treated, brain activity returns to normal levels. Psychological Risk Factors • Identifiable life crisis (marital breakdown, death in family). • Living environment (e.g. bad neighborhood) • Additional stresses associated with low socio-economic status. The Diasthesis-Stress Model Person who has gene variant + no significant stresses in life Low Risk Person who doesn’t have gene variant + many stresses in life Low Risk Person who has gene variant + stressors High Risk The Cognitive Schema • Intensely negative & irrational beliefs: Worthless Future is bleak Whatever happens, its going to get worse The Cognitive Schema Beck • Depressed patients are more negative in their thinking overall and in their thinking about themselves. • Negative beliefs can be detected in someone years before the depression begins. Peterson & Seligman • Depressed persons usually present with a pessimistic explanatory style. Depression in other contexts • Far more common in war-torn countries. • Less commonly diagnosed in Asian countries like China, Taiwan, and Japan than in the West. • People in Asian countries may differ in how they understand, display and perhaps even experience their own symptoms. TREATMENT OF MENTAL DISORDERS Different treatments target different causes Psychological Treatments Biomedical Treatments • Alter psychological and • Alter underlying biological environmental processes. • Changing perception and beliefs. • “Talk therapy” processes directly. • Administering medication or doing neurosurgery. PSYCHOLOGICAL TREATMENTS Cognitive Behavioral Therapy (CBT) Cognitive Therapy (developed by Beck) • Dysfunctional cognitions play a key role in the development of mental disorders. • Depressed people have negative beliefs about themselves, the world and the future, and distorted thought processes. Negative beliefs… World Self It’s a cruel world out there I am unlovable Future Things are only going to get worse Distorted Thought Processes All-or-nothing Overgeneralization • Now that I’ve lost the election, I am worthless • I lost my car keys – that’s just like me, I lose everything Disqualifying the positive • My doing well on the test today was just a fluke Emotional reasoning • I feel it, therefore I know it’s true Cognitive Restructuring - Some form of mental health counseling - Helps client become aware of inaccurate or negative thinking. - Focuses on patterns of thinking that are maladaptive. - Teach strategies for keeping certain thoughts readily available. • Challenging someone’s beliefs or habits of interpreting the world. - Outright efforts of persuasion - Confronting maladaptive beliefs Cognitive-Behavioral Approach • Present-focused. • Concerned with identifying and solving problems the patient wishes to address. • Highly structured sessions. • Patient expected to do homework – practice new skills or new ways of thinking learnt during therapy. • Group therapy is common BIOMEDICAL TREATMENTS Biomedical Treatment • Pharmacological – medications that alter information flow at the synapse; influences thoughts, feelings, behaviors. • Nonpharmacological – direct manipulation of the nervous system via surgery or electrical or magnetic pulses. Pharmacological Example Antidepressants • Medications designed to counteract depression. • Selective serotonin reuptake inhibitors (SSRIs) – e.g. Prozac, Zoloft, Paxil. • Increase serotonin turnover in the brain Pharmacological Example Antidepressants • Beneficial effects emerge only after drug is taken for a month or so. • Side effects include weight gain, nausea, diarrhea, insomnia, loss of sexual desire/response. • Overprescribed, possible risk of addiction. Nonpharmacological Example Electroconvulsive Therapy (ECT) • Used mostly for severe depression. • Brief, moderately intense electric current is passed through the brain to produce a convulsive seizure. • Patients are given short-acting anesthetics & muscle relaxants. • Works well for patients who have not responded well to medications. • Effects are quicker. Nonpharmacological Example Electroconvulsive Therapy (ECT) • May produce memory impairment. • But cognitive side effects are diminished if the ECT is delivered to just one side of the brain during therapy. • Use of ECT is controversial – generally reserved for use only after medication has failed or when there seems to be a serious chance of suicide. Copyrights Page 13 Work License Author/Source National Taiwan University YEE-SAN TEOH 37 National Taiwan University YEE-SAN TEOH 38 National Taiwan University YEE-SAN TEOH 45 National Taiwan University YEE-SAN TEOH 50 National Taiwan University YEE-SAN TEOH 53 National Taiwan University YEE-SAN TEOH 54 National Taiwan University YEE-SAN TEOH