Tips for Teaching Nursing Diagnosis and the Use of NANDA
advertisement

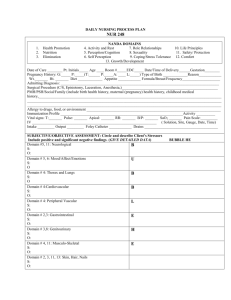
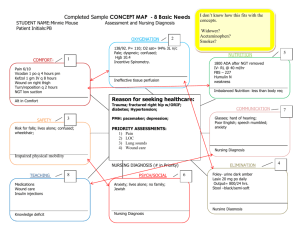
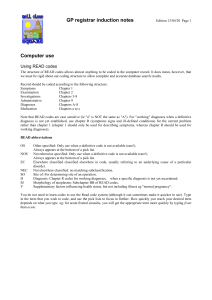
Tips for Teaching Nursing Diagnosis and the Use of NANDA International Terminology Nursing Diagnosis: Definition • The NANDA-I definition of a nursing diagnosis was adapted from a national, Delphi study by Dr. Joyce Shoemaker (1984) – Nursing diagnosis is a clinical judgment about individual, family, or community responses to actual or potential health problems/life processes. Nursing diagnoses provide the basis for selection of nursing interventions to achieve outcomes for which the nurse is accountable (NANDA, 1997). The Diagnoses • 206 NANDA-approved nursing diagnoses will be present in the Definitions & Classifications book for 2009 - 2011 • Level of Evidence (LOE) Criteria Established for All New and Revised Diagnoses – Entry into the Taxonomy requires various levels of clinical evidence Clinical Decision Making • Health care professionals face complex decisions daily regarding patient care— and must do so with decreased resources – What is the area of concern that nurses can treat/prevent/monitor? (Diagnosis) – What is an appropriate goal for this patient? (Outcome) – What treatment is most effective? (Intervention) Critical Thinking • Nurses need knowledge of diagnoses, definitions and defining characteristics, especially those common to the populations with which they work and the diagnostic processes that are used to interpret patient data • Skills of analyzing, logical reasoning, and applying standards are thinking processes required for accurate diagnosis in nursing • These skills are developed through: – Discussions of how data should be clustered to generate accurate diagnoses – Relation of data clusters to diagnoses – Comparisons of existing data to expected data based on research findings. Lunney (2009) Diagnosis Requires Assessment • Identifying human responses that are related to medical diagnosis without a complete assessment to determine the presence of defining characteristics – Lack of instruction on clustering assessment data to derive a list of potential diagnoses – Lack of hypothesis testing to determine best diagnoses for each patient Nurses Are Diagnosticians • Diagnosticians interpret data within their fields of expertise in order to provide needed services • A key element of data interpretations is that they are subject to error. – A good diagnostician must realize that there are always risks to the accuracy of data interpretations • Becoming a nurse diagnostician requires development of professional and personal skills and characteristics – Competencies in intellectual, interpersonal, and technical domains – Personal strengths of tolerance for ambiguity and use of reflective practice Teaching Methods • Review proper method to complete patient assessment to determine the presence of defining characteristics – Clustering of defining characteristics is often misunderstood : presence of one defining characteristic does not necessarily require a diagnosis – All nursing interventions do not require a nursing diagnosis • Medication administration for a condition that is not a primary focus of nursing care is related more to a medical diagnosis – Need to test hypotheses – Need to evaluate success of plan of care and reassess continually Diagnostic Process Assessment Cluster cues / defining characteristics Generate list of potential diagnoses Collect additional data to narrow list of potential diagnoses Determine diagnosis/diagnoses to be treated Implement plan of care based on identified diagnoses Evaluate success of plan of care Cue Generation and Nursing Diagnosis • Cues are analyzed in relation to possible diagnoses • Existing cues are matched with the expected cues for the diagnoses being considered • During the evaluation of cues and related diagnoses, nurses may decide that there are not enough data to make a diagnostic decision or that there is enough evidence for one or more likely diagnoses – If there are not enough data to make a diagnosis, then the next step involves a focused search for additional cues – If there is enough supporting evidence, a diagnosis is made and then validated Quality Nursing Care • Accurate Assessment and Diagnosis – Defining characteristics – Related factors – Risk factors • Identify Attainable Patient Outcomes – Efficiency • Utilize Proven Interventions – Effective – Least resource-intensive Quality Nursing Care • Accurate Assessment and Diagnosis – Defining characteristics – Related factors – Risk factors • Identify Attainable Patient Outcomes – Efficiency • Utilize Proven Interventions – Effective – Least resource-intensive Incorrect Diagnostic Process Assessment OR Identify Medical Diagnosis Cluster cues / defining characteristics Generate list of potential diagnoses Collect additional data to narrow list of potential diagnoses Determine nursing diagnosis/diagnoses to be treated Implement plan of care based on identified diagnoses Evaluate success of plan of care Teaching Methods • Requiring students to develop and detail care plans with “every possible diagnosis” creates resistance – Sets up situation that is not realistic • Cannot address every possible diagnosis in a short hospital stay – Becomes a “thing to do” rather than truly understanding and applying diagnostic reasoning and differential diagnosis • Students learn to “just pick a diagnosis” rather than making decisions about the best explanation(s) for patient responses Teaching Methods • Use of case studies can assist students in identifying cues in patient situations that may be defining characteristics of one or more nursing diagnoses • Hypothesis generation and differential diagnosis skills can be developed through case studies, clinical conference discussions and in skills lab scenarios “The List” • Automating the electronic record to populate the plan of care with nursing diagnoses when a particular medical diagnosis is used – Becomes a documentation tool rather than an individualized plan of care to direct nursing interventions to meet important patient outcomes – Puts patients at risk / Negligence • May ignore or miss important diagnoses for patients • Plan of care does not address critical outcomes for patients Reportable Quality Measures: Where is Nursing? • Management of diabetes: – Percent of adults with diabetes who had a foot examination in past year – Percent of adults with diabetes who had an influenza immunization in past year – Percent of adults with diagnosed diabetes with HbA1c level > 9.0% (poor control); < 7.0% (optimal) – Hospital admissions for short-term complications of diabetes per 100,000 population The Role of Nursing in Patient Quality • Percent of adults with diagnosed diabetes with HbA1c < 7.0% (optimal) – Readiness for enhanced family coping – Health-seeking behaviors – Readiness for Enhanced Self Health Management The Role of Nursing in Patient Quality • Management of diabetes: – Hospital admissions for short-term complications of diabetes per 100,000 population • • • • • • Anxiety Ineffective coping Ineffective health maintenance Risk for injury Deficient knowledge Ineffective Self Health Management Diagnostic Difficulties • Significant overlap of cues (Defining Characteristics) to diagnoses • Contextual factors such as culture can change the perspective on diagnosis • Many studies have verified that interpretations of clinical cases have the potential to be less accurate than indicated by the data – (Lunney, 2007).