Resources for the physical musculoskeletal exam
advertisement

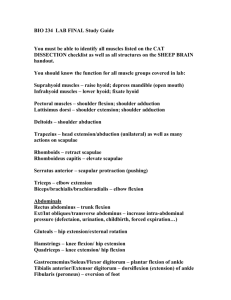
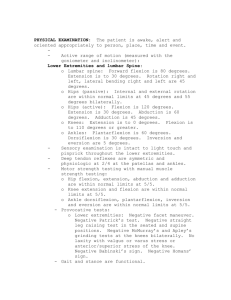
Resident MSK Exam Handout Last updated 1-4-2015 Brian Liem, MD and Leah Concannon, MD Sports and Spine University of Washington Good references: Excellent Texts: Musculoskeletal Physical Examination. An evidenced-based approach. Gerald Malanga and Scott Nadler. -Good book for describing tests -Good for giving sensitivity, specificity and inter-rater reliability of each test. Essentials of Musculoskeletal Care (3rd or 4th edition). Griffin. -Good outline of basic msk exams for each body part. PASSOR Physical Exam Guidelines Online Videos Any of the YouTube videos from Dr. Mark Hutchinson (University of Illinois) He has good physical exam tutorials especially for the knee and shoulder. Shoulder: https://www.youtube.com/watch?v=p60X8fADTeg&list=PLBD0682ECAFB37D24 Knee: https://www.youtube.com/watch?v=Rtp4oz0_3YY&list=PLBD0682ECAFB37D24&index= 8 Hip/Groin: https://www.youtube.com/watch?v=VuHsa4kxT0s&list=PLBD0682ECAFB37D24&index2 Other resources/articles Shoulder: The Role of the Scapula in Athletic Shoulder Function. Ben Kibler Am J Sports Med 1998. Screening of the athlete’s shoulder for impingement symptoms: a clinical reasoning algorithm for early detection of shoulder pathology. AM Cools and D Cambier. BJSM. 2008. General Comments about physical exam: 1. Try to do your exam the same way each time to be systematic. 2. Keep a differential in mind while performing the exam. The goal of the exam is arrive at a diagnosis and to cross conditions off the differential. 3. Patient positioning: Try to perform your exam in such a way that minimizes patient movement. Patients who have to get on and off of the examination table several times will become annoyed, especially those in pain. Remembering this tip can be difficult to do when you are first learning the examination because often you will forget to perform certain maneuvers and will want to return to the maneuver. 4. Not only are you trying to figure out what is wrong with the patient, but often your exam helps you to show the patient that there are biomechanical things that can be worked on in physical therapy (ie: the “sell”). 5. When evaluating a patient, remember the kinetic chain and evaluate other aspects of the body besides the joint/body part that hurts. For example, in an overhead throwing athlete with shoulder pain, look at the hip girdle strength because 50% of power comes from the hips and if this is weak, they put more pressure on shoulder to get the power and this puts more load on the shoulder structures. 6. Compare asymptomatic side to symptomatic side. 7. When evaluating the lumbar spine, also examine the hip since there is a hip-spine connection 8. When evaluating the cervical spine, also examine the shoulder since there is overlap in the pain referral patterns and involved structures. 9. All of these physical exam maneuvers have their limitations. No single examination maneuver is 100% specific or sensitive. Using several examine maneuvers in combination increases your sensitivity and specificity. C-spine Sitting Manual Muscle Testing (MMT) Tips on MMT: have the patient “Hang” their arm on yours -brace their shoulder when testing biceps so that flexion isn’t coming from the deltoid -mechanical disadvantage-- triceps testing. -5th digit finger abduction with your own 5th finger (otherwise you’ll always win) Sensation -C5-T1 dermatomes Reflexes -Use the NINDS 0-5 point scale - 2 = normal - 4 = clonus -Biceps (C5) -Brachioradialis (C6) -Triceps (C7)--- have the patient “Hang” their arm on yours Hoffman’s-Disputed meaning but most say it is an upper motor neuron sign, but may not always be pathologic. -What is a positive sign? -Thumb flex only? Or Thumb and Index finger? Palpation -Occiput -C2-C3 facets -Most common facet joints associated with “cervicogenic HA” -C7 spinous process (most prominent bony prominence in neck) Spurling’s Goal: Reproduce their typical radiating arm or neck symptoms -Can be used for radiculitis/radiculopathy -Can be used to assess for facet mediated pain Lhermitte’s (Dural tension) Goal: Reproduce their typical radiating arm or neck symptoms Standing Inspection: Posture Evaluate from side -Earlobe should align with acromion - Evaluate for rounded shoulders/head forward posture (Desk worker’s posture) -Puts strain on upper traps -Protracts shoulders so stretches rhomboids and trap muscles—muscles that are constantly stretched are weak. Cervical spine ROM Evaluate from behind or in front of patient -Flexion, Extension, Lateral rotation, Side Bending (Ear to shoulder) -Look for restrictions in motion and reproduction of typical pain. “Joel Press” “Elbows in pockets” maneuver Can perform to determine if there is improvement in cervical ROM while in this position. If there is improvement in ROM, this may help demonstrate to the patient that their upper traps too tight and lower traps and interscapular muscles weak Supine (usually done after shoulder standing) Neck/Cervical Distraction -Place cervical spine in slight flexion and pull up at the occiput -If improves radicular arm symptoms or axial neck symptoms may be a candidate for trial of traction in PT and/or ordering pneumatic traction device. Shoulder Standing Inspection -Assess SC and AC joints for asymmetry, clavicle for prior fracture -If one AC joint is more prominent could be sign of degenerative changes -Assess for atrophy of deltoid, biceps, supraspinatous and infraspinatous. -Atrophy can be from disuse or from denervation of peripheral nerve -Scapular positon at rest Palpation: -Subacromial space, bicipital groove, AC joint, SC Joint, spine scapula (level of T3), supraspinatous (level of T2), Inferior border scapula (level of T7) and infraspinatous fossa -Tip for finding AC joint: Find spine of scapula. Find clavicle. Track both of them laterally where they meet and this is the AC joint. ROM (Note: this is ROM for the Glenohumeral Joint) -Front: Active ROM Flexion (180 deg), Extension (60 deg), Abduction (180 deg), External Rotation (Elbows at the side, 60 degrees) Note: Watch for elevation of scapula (“hiking of shoulder”) as compensation for loss of active GH joint abduction and forward flexion. They are using upper trap and levator scapulae, hence why patients with shoulder pain often feel neck pain. -Back: Active ROM Internal rotation (Apley Scatch Test) -Assess hoow high can they reach up with thumb -Remember inferior angle of scapula is T7 -Patient’s with Rotator cuff disease often reach only to the lower lumbar region. Passive ROM Internal and External Rotation with shoulder in 90 deg abduction Note: You can also test passive ROM in supine position which has the advantage of stabilizing scapula against the exam table so that you only isolate GH joint range of motion. Adhesive capsulitis ROM: There is global loss of ROM with adhesive capsulitis (Frozen Shoulder) but the most prominent loss is in External Rotation Shoulder Strength testing : -Teres minor and infraspinatous -External rotation with elbow at the side -Subscap and pec major -Internal rotation Test with elbow at the side -Subscapularis specific testing - Lift off test (isolates better). Otherwise you may get pec major. -Bear Hug test (better for those who cannot reach behind)—hand on opposite shoulder. Examiner attempts to pull hand off of shoulder (inferior to superior directed force). -Supraspinatous -Empty Can (Jobe) testing -Key for positioning is adducting positioning at 30 deg which places SST in most optimal plane for testing. -Positive Test suggests supraspinatous tendinopathy vs. tear. Scapular Exam (from back) -Scapular Winging 3 sources of winging: 1) Serratus anterior dysfunction—classic medial winging 2) Rhomboid dysfunction 3) Trap dysfunction -General arm abduction arc (esp when lowering arm) to see if scapula upwardly rotates -Lateral scapular slide test (3 Kiber motions—Dr. Kibler is an Ortho Surgeon ) -Arms at side -Hands on Hips -Arms abducted to 90 deg -Scapular pinch -Normally can hold for 15-20 seconds, but weak muscles hold < 15 seconds -Scapular Assistance Test Goal: see if pain improved with assistance. Tells you that scapula does not upwardly rotate well because of weak serratus. Key fact: For every 2 deg of arm abduction, the scapula rotates up by 1 deg. Special tests (seated or standing position) Impingement (External and Internal) -Neer’s (Key is to stabilze scapula) -Hawkin’s -Yocum’s Glenoid Labral tear -O’Brien’s (adduct to 10-15 deg) -Mayo Shear---simulate thrower’s abduction and ER -Kim Biceps--- biceps is connected to labrum so when you stress the biceps tendon at lengthened position, pulls on labrum -Crank test (like Mayo shear) -Jobe Relocation (similar to relocation test for instability but you are looking for pain relief) AC joint (sprain, DJD) -Cross Arm adduction (Apley scarf test) -O’Brien’s also tests for this Biceps tendon -Speed’s -Yergason’s --- based on fact that biceps is strongest forearm supinator Instability -Sulcus sign—more for multidirectional instability -Load and shift Thoracic Outlet -Roos -Adson’s Supine Note: You can also test passive IR and ER in this position. The advantage of this position is that you can stabilize the scapula against the bed and isolate just the glenohumeral joint motion. Instability (Anterior mainly) -Apprehension test—putting arm in an ER and abducted position which is position of anterior dislocation, then gradually rotating until maximal ER. Examiner’s other hand applies pressure to posterior shoulder in an anterior posterior direction. -Relocation test--- looking for relief of instability feeling (not of pain) Prone -Superman to test periscapular muscle strength—normally can hold for 15 seconds. Elbow: Seated -Inspection -Swelling over olecranon to suggest olecranon bursitis -Active ROM -Look for restrictions in flexion/extension and supination and pronation: If there is, think of a loose body or some bony material restricting motion. -Palpation -3 main bony prominence s(medial epicondyle, lateral epicondyle and olecranon) -Proximal dorsal forearm along extensor muscle bulk -Palpation radiocapitellar joint--- often a site of OA 2/2 repetitive trauma -Distal triceps insertion over olecranon -Valgus and varus stress testing—put in 25 deg of flexion to unlock olecranon from olecranon fossa. Valgus: Mainly looking at UCL (aka MCL) Varus: Mainly looking at RCL (aka LCL) Specific Conditions -Lateral epicondylitis/losis testing -Resisted wrist extension and middle finger extension with elbow extended -Passive wrist FLEXION (puts the wrist extensors on stretch) -Medial epicondylitis/losis testing -Resisted pronation and wrist flexion for - Ulnar neuropathy -Tinel’s at elbow -Can reproduce tingling in 4th and 5th digits or tenderness at the groove Finger and wrist Seated Anatomy tips: - Memorize the 6 dorsal (extensor) compartments Anatomic snuff box is bordered by the 1st and 3rd dorsal compartments -Remember FDS vs. FDP are both finger flexors but flex the PIP and DIP joints respectively because of their insertions -Know the borders of the anatomic snuff box -Know the course of the median and ulnar nerves and sensory innervations Ie: Skin of Thenar eminence is innervated by palmar cutaneous branch. Inspection -Atrophy of thenar eminence (suggests carpal tunnel syndrome) -Atrophy hypothenar eminence (suggests ulnar neuropathy—wrist or elbow) -Finger deformities (ie: Joint in a flexion position) Specific conditions: -Carpal Tunnel Tests (Median nerve -Phalen’s (hold for 30 sec) and Tinel’s -Resisted Thumb abduction -Ulnar neuropathy -Froment’s for ulnar neuropathy (use a piece of paper between both thumbs) -Radial sided wrist pain -DeQuervain’s tenosynovitis -Finkelstein’s -Carpal Metacarpal Osteoarthritis -CMC grind test -Scaphoid fracture -Tenderness in anatomic snuff box -Ulnar sided wrist pain TFCC tear -TFCC compression Extersor carpi ulnaris (ECU) tendinopathy -Resisted wrist extension with wrist in slight ulnar deviation Hook of Hamatee Fx -Palpation over the hamate -Dorsal Wrist pain -Scapholunate dissociation -Watson’s test Low back Standing Inspection -Gait -Trendelenberg -Antalgic -Walk on toes and heels (functionally tests L4-L5 and S1) -Posture from side - do they have increase hip flexion which may be sign of tight hip flexor? - do they have increased lumbar lordosis that puts pressure of facets and pars? -Posture from back -do they shift to one side (shift is away from the side of neural compression) -Increased paravertebral musculature on one side to suggest scoliosis curve on that size -Single leg squat to evaluate for functional hip abductor strength Palpation -Lumbo-sacral palpation - PSIS: Level of S2 -Iliac crest: level of L4 -Lumbar ROM -Flexion -Do they bend at the lumbar spine or at the hips? -Extension -Facet loading -Schober test if possibility of inflammatory component Seated -MMT -Sensory testing (Dermatomes L2-S1) -Reflex testing Don’t forget medial hamstring (L5) -Seated Slump -“Sitting in a cop car” Supine -Straight leg raise -Hip examination Prone Note: You may choose to do palpation in this position as often patients are more relaxed and less guarded. -Reverse straight leg (upper lumbar segments)/Femoral nerve stretch Hip Standing -Everything you did for Low back Palpation -Palpation trochanter in standing (sway or “put out a cigarette”) -Palpation Iliac crest (higher than you think; marks level of L4) -ASIS (feel like hooks)—this is origin of Sartorius muscle. Seated Resisted hip flexion – reproduction of pain may be consistent with hip flexor issue Supine -Look of leg length discrepancies (functional and true)—measure from ASIS to medial malleoli -Passive IR and ER ROM -Scour maneuver--- if positive, points to intra-articular source of pain. -FADIR (Flexion adduction internal rotation)—impingement (FAI or labral tear) -FABER (Flexion abduction external rotation) -Groin pain = Intra-articular -Buttock pain = classically thought to be SI joint -Resisted Straight Leg Raise—for intra-articular pain -Hip distraction with IR if you suspect they have an intra-articular pathology like OA -Pain may improve as compared to IR without distraction. -Posterior compression for SI joint pain -Modified Thomas test for hip flexor tightness -Active SLR with and without side compression -If easier to perform with side compression from examiner may be indication for for SI joint belt. Sidelying -Hip abductor (glut med and glut min) strength in side lying. Make sure patient doesn’t cheat with hip flexors. Pull out into extension if want more isolation and to make it harder. -Ober’s for tight iliotibial band (ITB) Knee Standing Inspection -Look at knee and ankle alignment. -Valgus or varus alignment? -Varus alignment may put more pressure on medial compartment -Increased Q angle? -Double leg Squat—look to see if their knees dive into valgus and for overpronation at the ankle -Single leg squat -Look for femoral adduction and internal rotation to suggest functional weakness of the hip abductors and external rotators -Look for overpronation at the ankle. -Duck walking--- pain reproduced suggests meniscal or intra-articular pathology -Patellofemoral specific: If you suspect patellofemoral pain syndrome, you may try these maneuvers to see if pain improves while squatting -Support over medial foot arch by examiner to counteract pronation -Squat while squeezing gluteal muscle as if “pinching credit card” in between the buttocks to engage the gluteal muscles -Squat with lateral to medial support over the patella from the examiner to keep the patella from tracking laterally. Seated -Active ROM in flexion/extension -Palpation for crepitus -J Sign (lateral patellar deviation during terminal extension) Supine Key is to have them relax their leg so that they don’t fight you--- a trick is to log roll the leg first Straight leg -Look for loss of extension in a knee—often in OA or intra-articular loose body like a meniscus flap tear -See if you can place your hand underneath the posterior knee -Patellar glide motion -Patellar facet palpation -Bulge sign (for an effusion) -Palpate posterior knee for fullness--- can be sign of Baker’s cyst Knee flexed -End range of flexion to see if reproduces pain---often meniscus or OA has pain -Joint line palpation -Anterior (ACL) and posterior (PCL) drawer Valgus and varus testing -key is to stabilze the femur ACL Testing Lachman’s -Make sure patient is relaxed to get a good sense of laxity (ie: their quad is not contracted) -Should feel firm end point. -Knee flexed to 30 degrees to unlock the tibia from femur “Small Hands” Lachman’s -Place patient’s leg over your femur. Stabilize pateint’s femur with one hand and lift up the tibia with the other. Meniscus Testing McMurray’s: Keep your fingers on the joint line to feel for palpable clunks. Classically to correctly do this pt’s knee is first flexed and slowly brought into extension coupled with the following motions to specifically target medial vs. lateral meniscus: EXTERNAL ROTATION + VALGUS = medial meniscus INTERNAL ROTATION + VARUS = lateral meniscus Apley’s grind--- for meniscus Noble’s for ITB--- pain in “ITB syndrome” is at the femoral condyle (not at the insertion of the ITB at Gerdy’s tubercle). Foot/Ankle Inspection in standing Examine for pronation (combo of ankle DF, subtalar eversion, forefoot abduction) and pes planus -Over-Pronation has been implicated in 1. Patellofemoral pain 2. ITB syndrome 3. Tib posterior tendinopathy Have patient stand on their toes and look to see if there is inversion of the ankles. This may be sign of weak peroneals which often happens in those who sprain their ankles. Palpation Ankle: -Anterior ankle/Talar dome -Medial malleolus -Lateral malleolus -Achilles’ tendon Midportion Insertion -Along peroneal tendons for peroneal tendinopathy (often occurs in patients who walk on uneven surfaces) Foot: -Medial calcaneal tuberosity—plantar fasciitis -Navicular--- site of stress fracture -Base of 5th—site of stress fractures, Jones fracture -1st MTP—site of hallux valgus, turf toe, sesmoiditis, OA (hallux rigidus), gout. -Metatarsal shafts—focal tenderness if suspect stress fracture -Metatarsal heads--- for metatarsalgia -Webspaces--- for morton’s neuroma Ottowa Ankle and Foot Rules for getting an X-ray to r/o Fx 1. Pain in malleolar or foot region 2. Bony tenderness (within 6 cm of distal tip of medial or lateral mallolus or at base of 5 th or naviuclar) Or Inability to bear weight for 4 steps Active and resisted ROM -Dorsiflexion—assess in 2 positions -Knee extended—more gastrocs because in this position the tendons taut as crosses knee joint -Knee flexed---isolates soleus -1st Ray Dorsiflexion--- normal is 70 deg Eversion -Weak in: -Peroneal tendinopathy -L5 radiculopathy -Peroneal neuropathy Lateral ankle sprain -Anterior Drawer -Talar Tilt High ankle sprain -Squeeze test -DF and Eversion stress to open up the ankle mortise Thompson test for Achilles rupture Metatarsal squeeze test for morton’s neuroma