6c Immunity
advertisement

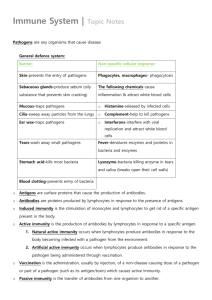
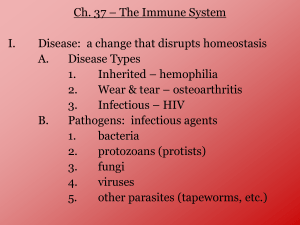
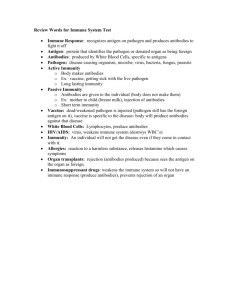
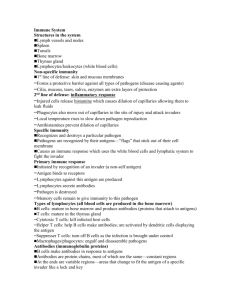
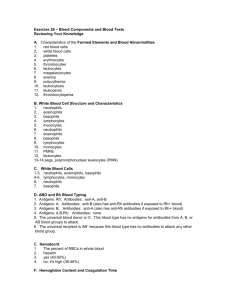
Immunity Pathogen “Path” = disease “ogen” = generating A pathogen is something that causes disease. A biological pathogen is a bacterium, virus, fungi, yeast, protozoa, worms, etc. A non-biological pathogen can be a toxic chemical, asbestos, etc. Usually, the term “pathogen” refers to a biological pathogen. Sizes of Pathogens Bacteria are so small that hundreds of them can fit inside one white blood cell. However, bacteria usually do not invade body cells. They live between the cells of the body, using up nutrients in the area, and they cause harm by secreting toxins. Viruses are so small that thousands of them can fit inside the NUCLEUS of one white blood cell. They always try to invade body cells because they need a piece of our DNA or RNA in order to replicate. When a body cell has been invaded by a virus, the entire cell must be killed by a white blood cell. Antigen An antigen is anything that causes an immune response, which isn't necessarily a biological pathogen (disease-causing organism). A non-biological antigen can be pollen, dust, grass, or anything that a person is allergic to. Pollen can be an antigen to a person with allergies, but it is not an antigen to a person without allergies, because no immune response was launched. LEUKOCYTES (White blood cells) all fight infection BASOPHILS – MAST CELL EOSINOPHILS NEUTROPHILS MONOCYTES – MACROPHAGES LYMPHOCYTES – B CELLS – T CELLS BASOPHILS Basophils – only about 0.5% of all leukocytes – Granules secrete histamines (vasodilation; more WBCs can get to the infection site) – Antihistamines interfere with the function of basophils. – Mast Cell: a basophil that leaves the blood vessel and enters the tissues. Eosinophils Eosinophils – compose 1-4% of all WBCs – Play roles in: Ending allergic reactions, parasitic infections During these conditions they increase in numbers: eosinophilia (too many is ___philia too few is ___penia) Neutrophils Neutrophils – most numerous WBC First to respond to infection – Phagocytize and destroy bacteria – Also destroy bacterial toxins in body fluids – Nucleus – has two to six lobes Neutrophils Neutrophils are the white blood cells that contribute to immunity mainly by engulfing BACTERIA and foreign bodies (thorns, dirt, etc) in a process called phagocytosis. They release the contents of their lysosomes onto the invader, dissolving it. When a bacterium has a capsule, it makes it hard to phagocytize, so the neutrophil requires opsonization by antibodies. Opsonization Some bacteria have evolved a slippery capsule around them as a defense against phagocytosis. The neutrophil cannot engulf this type of bacteria. Neither can a macrophage. When an antibody attaches to this type of bacteria, the neutrophil can now grab onto the antibody like a handle, enabling it to phagocytize the bacteria. This process of facilitation of phagocytosis is called opsonization. When an invading bacteria has the antibody attached to its cell membrane, the entire structure is now called an antigen-antibody complex. If a bacterium does not have a capsule, the neutrophil can destroy it without opsonization. The antibody can also destroy the bacterium by itself by popping the cell membrane. But when a capsule is present, the neutrophil and antibody work best together. Neutrophils are also the ones that primarily destroy the dissolved toxins that bacteria secrete into body fluids. Monocytes Comprise about 5% of all WBC’s. Like neutrophils, they phagocytize (eat) bacteria, old cells, and foreign bodies. They have more types of lysosome enzymes than neutrophils so they are better at killing difficult pathogens. They also use antibodies for opsonization. When they leave the bloodstream and enter the tissues, they are called MACROPHAGES. WBC’s leave the blood vessel to enter the tissues What’s the Difference between Neutrophils and Monocytes/Macrophages? There are 10x more neutrophils in the bloodstream than monocytes/Macrophages. Consider neutrophils to be the most numerous white blood cell. However, there are more macrophages in the tissues of the body. They are everywhere! Neutrophils live only a few days. Monocytes/Macrophages live a few months. Lymphocytes live for years. Monocytes/Macrophages are larger and slower than neutrophils, but they can phagocytize larger organisms and more of them. Neutrophils usually just phagocytize bacteria until they die. Macrophages phagocytize and then take pieces of the dead bacteria and present them to lymphocytes so a larger immune response can occur. Differences in Function There are two types of phagocytes: Neutrophils and macrophages. – Neutrophils and macrophages both mainly function by phagocytizing bacteria (not viruses). Lymphocytes are mostly needed to kill off body cells infected by viruses. Differences in Function Neutrophils just phagocytize bacteria and secrete chemicals to recruit more white blood cells to the site. Unlike neutrophils, macrophages have surface receptors; these "recognize" the surface of the pathogen’s cell membrane. Macrophages phagocytize the bacteria, pop their lysosomes onto it, and dissolve it, except for some pieces of the bacteria’s cell membrane. The macrophage places these pieces of bacteria on its own cell membrane, and finds a lymphocyte to present it to. Differences in Function Macrophages present these pieces to T cell lymphocytes and to B cells lymphocytes. The lymphocyte feels the shape of the bacteria pieces on top of the macrophage, (this is called “antigen presentation”) and the lymphocyte can then launch an attack on the rest of the bacteria still alive in the body. In this way, the macrophage recruits even more lymphocytes to join the war. So, what is a lymphocyte? Lymphocytes 20–45% of WBCs – The most important cells of the immune system – There are two types of lymphocytes; one type is effective in fighting infectious organisms like body cells infected with viruses – Both types of lymphocytes act against a specific foreign molecule (antigen) Lymphocytes Two main classes of lymphocyte – – B cells – Originate in the bone marrow, mature into plasma cells. A mature plasma cell fights infection by producing antibodies T cells – Originate in the thymus gland. They attack foreign cells directly (including organ transplants!). They can also kill viruses. Lymphocytes B cells – mature into plasma cells Plasma cells secrete antibodies; the plasma cell’s antibodies are what kills the attacking cell. Antibodies attack in two ways: – – They attach to bacteria and pop the cell membrane They attach to encapsulated bacteria to help neutrophils and macrophages to phagocytize them. Disorder of B-cell Lymphocytes Mononucleosis: Epstein Barr virus attacks B lymphocytes. It is characterized by inflammation of lymph vessels (lymphangitis). – Lymphangitis: lymph vessel inflammation; usually from infection. Infected lymphocytes have a characteristic scalloped edge where they touch RBC’s Function of a B Lymphocyte Figure 17.6b T-cell Lymphocytes T cells – coordinate the immune response by recruiting other white blood cells. They can directly destroy bacteria by popping their cell membrane. T cells can also directly destroy foreign cells by popping the cell membrane. They do not need to phagocytize the invading cell. They do not need the assistance of antibodies. T-cells can therefore kill a body cell that has become infected with viruses. T-Cell T-cell Lymphocytes T cells are the cells that attack organ transplants! Immunosuppression drugs are designed to inhibit the action of T cells. T cells are attacked by the HIV (AIDS) virus. The thymus gland secrets certain hormones which can cause T cells to become immunocompetent (makes the cells mature and start to work) T Cells There are several types of T cells. The main types are Cytotoxic (Killer) T cells – Go out and directly kill bacteria or infected host cells Helper T cells – Release chemicals called “cytokines” to call in more white blood cells of all types to join in the war. They also present the macrophage’s antigen to a B cell, which causes it to produce antibodies against that particular bacteria. The B cell is now called a plasma cell Suppressor T cells – Stop the immune process when it is over, and also "tell" some plasma cells to "remember" how to destroy that specific pathogen. Those plasma B-cells are then called Memory B-Cells. They can react to the same pathogen faster, the next time it invades because Memory B-cells already have the proper antibodies stored up for that pathogen. Killer TCell Virus-Infected Cell Function of a T- Lymphocyte Figure 17.6a Summary A pathogen somehow gets past the body's physical and chemical barriers and the inflammation response. The pathogen is engulfed by a macrophage (or neutrophil). The macrophage releases the contents of its lysosomes onto the bacterium and dissolves most of it. There are still some pieces of the bacterium’s cell membrane left. The macrophage then forces the surface proteins of the bacterium (antigens) to it's own cell surface. Helper T-Cells touch these surface antigens, make a copy of their shape, and present them to B-cells to make antibodies against them. Summary These Helper T-Cells begin to multiply and have two main roles. The first is to activate B-Cells and "tell" them how to neutralize the pathogen by presenting the pieces of the bacterium cell membrane so the B-cells can turn into plasma cells which make the antibodies. – The B-Cells (now called Plasma cells because they have been activated) begin to multiply and produce the antibodies to neutralize this specific pathogen. The second role of Helper T-Cells is to activate the Killer T-Cells by secreting cytokines. Killer T-Cells can either destroy the pathogen itself (bacteria), or destroy the entire body cell which is infected (viruses). When the immune response is over, Suppressor T-Cells stop the process and also "tell" some B-Cells (plasma cells) to "remember" how to destroy that specific pathogen. Those B-cells (plasma cells) now become Memory B-Cells. Antibodies Antibodies (also known as immunoglobulins, abbreviated Ig) are proteins made by plasma cells. They are used to identify and neutralize foreign objects, such as bacteria and viruses. They are typically made of basic structural units—each with two large heavy chains and two small light chains—to form a unit shaped like the letter “Y” A Typical Antibody The tips of the “Y” have receptors that are specific for a particular antigen. The stem of the “Y” can be grasped by a phagocyte. Antibodies The small region at the tip of the protein is extremely variable, allowing millions of antibodies with slightly different tip structures, or antigen binding sites, to exist. This region is known as the hypervariable region. Each of these variants can bind to a different target, known as an antigen. This huge diversity of antibodies allows the immune system to recognize an equally wide diversity of antigens. Antibodies Some of these “Y” shaped units exist by themselves (monomers) Some are in pairs (dimers) Some are in a cluster of five (pentamers) There are five different antibody types , which perform different roles, and help direct the appropriate immune response for each different type of foreign object they encounter. #1 #2 #3 Precipitation/agglutination 38 Types of Antibodies IgD – initiation of immune response IgE – stimulates allergic reactions, good for worm infections IgG – highest concentration in blood, highest amounts in most secondary responses, crosses the placenta IgA – secretory Ig, found in secretions, highest concentration in body IgM – produced first, best at C’ activation J-Protein is what attaches the antibody segments Capsule Pops the cell Virus Opsonization Bacteria Bacteria Antibodies Plasma Cell Pops the cell Cytokines Phagocytosis STOP Presentation Neutrophil Macrophage (Monocyte in bloodstream) B-Cell Helper T-Cell Killer T-Cell Lymphocytes Suppressor T-Cell IMMUNITY Most people are sick more often as children than as adults in their 20s through 30s because we build up many varieties of memory lymphocytes during childhood, providing immunity from more and more antigens during adulthood. Myasthenia gravis Myasthenia gravis (MG): autoimmune disease where antibodies destroy or block receptors for acetylcholine, a neurotransmitter. Causes muscle paralysis. First attacks small muscles especially those that keep eyes open; will spread to diaphragm death. To stave off effects, do thymectomy. Aspirin One baby aspirin a day can help prevent blood clots. It blocks the ability of an enzyme called COX (cyclo-oxidase) to cleave arachidonic acid into a molecule called a prostaglandin. Prostaglandins are needed for inflammatory reactions and for making clotting factors. COX inhibitors, such as aspirin, block pain from inflammation, but they also INCREASE blood clotting time. Fig. 9-1 Hematopoiesis 44 Life span, from longest-lived to shortest-lived: Lymphocytes Erythrocytes Platelets Neutrophils Terms Excess neutrophils: neutrophilia Few neutrophils: neutropenia Excess platelets: thrombocytophilia Few platelets: thrombocytopenia WBC Count White blood cell (WBC) count is a count of the actual number of white blood cells per volume of blood. Both increases and decreases can be significant. White blood cell differential looks at the types of white blood cells present. There are five different types of white blood cells, each with its own function in protecting us from infection. The differential classifies a person's white blood cells into each type: neutrophils (also known as segs, PMNs, granulocytes, grans), lymphocytes, monocytes, eosinophils, and basophils. BLOOD TYPING: The ABO SYSTEM Blood typing is the technique for determining which specific protein type is present on RBCs. Only certain types of blood transfusions are safe because the outer membranes of the red blood cells carry certain types of proteins that another person’s body will think is a foreign body and reject it. BLOOD TYPING These proteins are called antigens (something that causes an allergic reaction). There are two types of blood antigens: Type A and Type B. A person with Type A antigens on their blood cells have Type A blood. A person with Type B antigens have Type B blood. A person with both types has type AB blood. A person with neither antigen has type O blood. BLOOD TYPING If a person with type A blood gets a transfusion of type B antigens (from Type B or Type AB, the donated blood will clump in masses (coagulation), and the person will die. The same is true for a type B person getting type A or AB blood. Type O- blood is called the universal donor, because there are no antigens, so that blood can be donated to anyone. Type AB+ blood is considered the universal acceptor, because they can use any other type of blood. This blood type is fairly rare. The rarest blood type is AB negative. RH FACTOR There is another term that follows the blood type. The term is “positive” or “negative”. This refers to the presence of another type of protein, called the Rh factor. A person with type B blood and has the Rh factor is called B positive. A person with type B blood and no Rh factor is called B negative. RH FACTOR The reason this is so important is that if an Rh- mother has an Rh+ fetus in her womb (from an Rh+ father), her antibodies will attack the red blood cells of the fetus because her body detects the Rh protein on the baby’s red blood cells and thinks they are foreign objects. This is called Hemolytic Disease of the Newborn (HDN). HDN This can be prevented if the doctor knows the mother is Rh- and the father is Rh+, because that means the baby has a 50% chance of being Rh+ like the father. Therefore, anytime a mother is Rh-, even if the mother says the father is Rh-, you can’t be sure who the father is, so they will proceed as though the baby may be Rh +. They will give her an injection of a medicine (Rhogam) that will prevent her immune system from attacking the baby. Rhogam Rhogam is given at 18 weeks into the pregnancy and again within 72 hours after giving birth. It is usually given within 2 hours after giving birth since you can’t trust the patient to return after they leave the hospital. The first baby is not at risk; during the first birth (or miscarriage), the placenta tears away and that’s when the baby’s blood cells get into the mother’s bloodstream. She then forms antibodies against the Rh factor, which are ready to attack the second fetus. The baby does not make the Rh factor until about 18 weeks into the pregnancy. IMMUNE SYSTEM INFLAMMATORY REACTION: When you get stuck by a thorn or have an infected cut, the body goes through a series of events called an inflammatory reaction. Four outward signs: – – – – Redness (erythema or rubor) Heat (calor) Swelling (edema) Pain (dolor) INFLAMMATORY REACTION Redness is caused from the blood vessels dilating to allow more blood flow to the area. Within the blood are platelets to clot the blood, proteins to repair the damage, and macrophages, which are white blood cells that eat up the foreign body, bacteria, or the dead cells. Heat is caused because of the extra amount of warm blood flow to the area. Swelling is caused from the plasma that leaks out of the swollen blood vessels. Pain is caused from the pressure of the extra fluid pressing on nerves in the area. ADAPTIVE IMMUNITY Two types of Adaptive Immunity – ACTIVE immunity Naturally Acquired Artificially Acquired You can also think of it this way – PASSIVE immunity Naturally Acquired Artificially Acquired Active Immunity Naturally Acquired – The body is naturally exposed to an infectious agent and launches an immune reaction Artificially Acquired – The person is injected with a weakened (attenuated) or killed organism, as found in a vaccination Naturally Acquired Active Immunity This is when the body is exposed to an infectious agent and the body has to work to produce antibodies which specifically attack that infectious agent. The white blood cells secrete these antibodies which will continue to circulate sometimes for years, ready to attack that type of bacteria and cause them to pop like a balloon before the body can become sick. Naturally Acquired Active Immunity – You catch a cold and eventually get better. You can never get the same cold virus twice because you will have become immune to it. Your next cold is from a different virus. There are hundreds of thousands of cold viruses; that’s why there is no cure for the common cold. – Another example is when an unvaccinated child is exposed to the measles at school and gets the disease, but never gets the disease again. However, there are some diseases that you don’t want to get, even once, such as polio, diphtheria, tetanus, and influenza, because the first exposure could kill or disable you. For these diseases, we have vaccines which are made of those organisms which have been altered (attenuated) so that the body recognizes them as foreign, but they can’t cause disease. That way, if the person is exposed to the real organism later, the antibodies are already there to kill it off without the body getting sick. Artificially Acquired Active Immunity An example is when a child is vaccinated against measles as a baby, so when he gets to school and is exposed to the disease, he doesn’t get sick. Passive Immunity Naturally Acquired – Example is the passing of antibodies from mother to infant in breast milk Artificially Acquired – Example is when a person receives an infusion of antibodies from someone else. Active vs. Passive Immunity Active immunity is long-lived, and may last for years or even a life time. Passive immunity is short lived, and may last only for a few months. NOTE: A vaccination is not the same as receiving an anti-toxin or anti-venom injection. More on that in Micro class. ALLERGIES From a hypersensitivity to substances such as pollen or animal hair that would not ordinarily cause a reaction. There are two types of allergic responses: Immediate Delayed Immediate allergic response Occurs within seconds of contact with the thing causing the allergy. This is the case with anaphylactic allergies, where someone who is allergic to seafood or peanuts can actually die within minutes because the allergic reaction is so severe the throat swells shut and they can’t breathe. They need an injection immediately of epinephrine that will stop the reaction. Delayed allergic response Delayed allergic response is when the body’s first exposure to the substance will not cause a reaction, but all exposures afterward will trigger the response. An example is poison ivy. You won’t itch the first time you touch it. Common allergens 71 Chemical mediators of allergies Preformed – histamine - ↑ vascular permeability; smooth muscle contraction – proteases – mucous secretion, generation of complement split products Newly formed (30-60seconds) – leukotrienes - ↑ vascular permeability; contraction of pulmonary smooth muscles – platelet activating factor – platelet aggregation; contraction of pulmonary smooth muscles – prostaglanin D2 – vasodilation; contraction of smooth muscles – cytokines – chemotactic and inflammatory 72 Symptoms of allergy dependent upon site of allergen exposure wheal-and-flare reaction – Pruritis (itching), erythema – skin bronchoconstriction mucous secretion vasodilation (shock) 73 74 Localized anaphylaxis (atopy) reaction limited to the site of allergen exposure pruritis (itchy) and urticaria (hives) allergic rhinitis (hay fever) asthma (atopic asthma) atopic dermatitis (eczema) food allergies 75 Allergic asthma stimulation of ‘allergy attack’ – airborne allergens – pollen, dust, insect parts – blood borne allergens – viral antigens – degranulation of mast cells due to IgE cross-linking lower respiratory tract symptoms – – – – airway edema mucous secretion inflammation = airway obstruction and damage asthmatics are hypersensitive to allergens ~5% of U.S. population symptoms can range from somewhat mild to lifethreatening (<5% severe asthma) 76 AUTOIMMUNE DISEASE A hereditary problem where the body thinks its own tissues are foreign bodies, and it constantly tries to kill off its own tissues.