THE COMPLEMENT SYSTEM THE COMPLEMENT SYSTEM The
advertisement

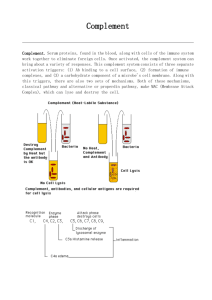
THE COMPLEMENT SYSTEM THE COMPLEMENT SYSTEM • The complement system is a set of plasma proteins that act in a cascade to attack and kill extracellular pathogens. • Approximately 30 components: – – – – activating molecules regulator factors complement receptors membrane proteins wich inhibit the lysis of host cells • Most of the complement proteins and glycoproteins are produced in the liver in an inactive form (zymogen). Activation is induced by proteolitic cleavage. AMPLIFICATION OF THE COMPLEMENT CASCADE inactive precursors limited proteolysis enzyme activating surface Activating surface needed! ACTIVATION OF THE COMPLEMENT SYSTEM COMPLEMENT SYSTEM CLASSICAL PATHWAY MB-LECTIN PATHWAY ALTERNATIVE PATHWAY COMPLEMENT ACTIVATION RECRUITMENT OF INFLAMMATORY CELLS OPSONIZATION OF PATHOGENS FACILITATING PHAGOCYTOSIS DIRECT KILLING OF PATHOGENS ACTIVATION VIA THE CLASSICAL PATHWAY THE C1 COMPLEX Collagen „legs” Gobular „heads” C1 is always present in serum but it can operate on an activating surface in normal case Low affinity binding to the Fc region of antibody conformational change activation Multiple interaction with immune complexes Different isotypes of antibodies activate the complement system differently The classical pathway: Fixation of complement, generation of C3b by the classical C3 convertase ACTIVATION VIA THE MANNAN-BINDING LECTIN PATHWAY GLYCOSYLATION OF PROTEINS IS DIFFERENT IN VARIOUS SPECIES Prokariotic cells Eukariotic cells Mannose Glucoseamine Mannose Galactose Neuraminic acid (sialic acid) MANNAN-BINDING LEKTIN ACTIVATES THE COMPLEMENT SYSTEM MASP = MBL associated serin protease ACTIVATION VIA THE ALTERNATIVE PATHWAY Alternative pathway is instantly inactivated on eukariotic cell surfaces (in the presence of sialic acid molecules) C3b can derive from classical or the lectin pathway too THE CENTRAL COMPONENT OF THE COMPLEMENT SYSTEM Complement fixation Strong covalent binding (3 900 000 000 000 000 molecules/ml) C5-CONVERTASE (C4bC2bC3b) C3-convertase + C3b= C5-convertase The classical and alternative C3-convertase is different in structure but common in function MEMBRANE ATTACK COMPLEX (MAC) MAC in the cell membrane live and bacteria dead COMPLEMENT ACTIVATION SUMMARY COMPLEMENT SYSTEM CLASSICAL PATHWAY Antigen-antibody complex C1q, C1r, C1s Serin protease C4, C2 C4a* MB-LECTIN PATHWAY ALTERNATIVE PATHWAY Mannose Pathogen surface MBL MASP-1/MASP-2 C3 B, D Serin protease C4, C2 C3 CONVERTASE C3a, C5a C3b Inflammatory peptid mediators Phagocyte recruitment Opsonization Binding to phagocyte CR Immune complex removal Terminal C5b – C9 MAC Pathogen/cell lysis The role of complement system in in vivo Alternative, lectin & classical pathway lysis MAC C3 C3a C3b C3b C3b C3b C3b C4a C5a inflammation opsonization phagocytosis Local inflammatory responses can be induced by the small complement fragments C3a, C4a, and especially C5a OPSONIZATION C3b bacterium complement receptor macrophage Complement receptors Name Ligand Expression CR1 C3b>C4b, iC3b rbc, Mo/MF, Gr, B activated T, follicular DC C3d, C3dg, iC3b EBV, IFNa, CD23 B, act. T, foll. DC iC3b> C3dg, C3d ICAM-1, LPS, fibrinogen Mo/MF, Gr, NK Mo/MF, Gr, NK CD11c/CD18 iC3b, C3dg, C3d fibrinogen C3aR C3a M, B, Gr, Mo/MF, platelet, SMC, neuron C5aR C5a,, des-Arg-C5a M, B, Mo/MF, platelet, SMC, neuron C1qR C1q collagen part B, NGr, Mo/MF, EC C1qRp C1q phagocyte CD35 CR2 CD21, CD21L CR3 CD11b/CD18 CR4 ACTIVATION VIA THE CLASSICAL PATHWAY REGULATION OF THE COMPLEMENT SYSTEM Regulatory proteins on human cells protect them from complement-mediated attack CD59 prevents assembly of terminal complement components into a membrane pore Regulation of complement system Factor I a-2macrogl C1Inh DAF C4bp CR1 MCP LECTIN PATHWAY HRF C-pept.ase N CD59 Properdin S-protein DAF positive feedback Fact-H CR1 MCP Factor I membrane protein soluble molecule MAJOR REGULATING FACTORS OF COMPLEMENT SYSTEM C1Inh: C1-inhibitor (serine-protease inhibitor) Factor I: inhibits both C3 convertases in the presence of co-factors (C4bp – classical pw., factor H – alternative pw., MCP – both) DAF(CD55): Decay Accelerating Factor MCP: Membrane Cofactor Protein MIRL(CD59): Membrane Inhibitor of Reactive Lysis Properdin: stabilize convertases of alternative pathway Deficiencies of complement system – cascade molecules Not the lysis of cells is the most important function of the complement system Deficiencies of regulatory molecules, receptors One of the major function of C1 INHIBITOR C1q binds to IgM on bacterial surface C1q binds to at least two IgG molecules on bacterial surface Binding of C1q to Ig activates C1r, which cleaves and activates the serine protease C1s C1INH dissociates C1r and C1s from the active C1 complex HEREDITARY ANGIONEUROTIC EDEMA (HANE) (HEREDITARY C1INH DEFECT) • 17-year old boy - severe abdominal pain (frequent sharp spasms, vomiting) • appendectomia normal appendix • similar symptoms occured repeatedly earlier in his life with watery diarrhea • family history of prior illness • immunologist’s suspicion: hereditary angioneurotic edema • level of C1INH: 16% of the normal mean • daily doses of Winstrol (steroid) – marked diminution in the frequency and severity of symptoms • intravenous purified C1INH became avaible by the time Main symptoms: • swellings of skin, guts, respiratory tracts • serious acute abdominal pain, vomiting • larynx swelling – suffocation, may cause death Treatment: • iv C1INH, FFP, steroid • kallikrein and bradykinin receptor antagonists Child with symptoms of HANE Pathogenesis of hereditary angioneurotic edema activation of XII factor Inhibition by C1INH in many steps • bradykinin and C2-kinin: enhance the permeability of postcapillar venules activation of kallikrein activation of proactivator by contraction of endothel • holes in the venule walls • edema formation cleveage of kininogen to generate bradykinin, vasoactive peptide • C1 is always active without cleveage of C2a to generate C2-kinin, vasoactive peptide cleveage of C2 to generate C2a cleveage of plasminogen to generate plasmin activation of C1 activating surface because plasmine is always active Q&A HANE 1. Activation of complement system results in the release of histamine and chemokines, which normally produce pain, heat and itching. Why is the edema fluid in HANE free of cellular components, and why does the swelling not itch? Histamine release on complement activation and recruiting of leukocytes is caused by C3a and C5a, both generated by the C3/C5 convertases. In HANE C1 constantly activate C2 and C4 in the plasma but C4b is rapidly inactivated because it does not bind to activating surface; for that reason, and because the concentrations of C2 and C4 are relatively low, no C3/C5 convertase is formed. Edema is caused by C2-kinin and bradykinin. 2. Which complement component levels will be decreased? Why? C2 and C4, because of the continous cleavage by activated C1. Q&A HANE 3. Would you expect the alternative pathway components to be low, normal or elevated? C1 plays no part in the alternative pathway. This pathway is not affected. 4. What about the levels of the terminal components? The unregulated activation of the early components does not lead to the formation of the C3/C5 convertase, so the terminal components are not abnormally activated. 5. Despite the complement deficiency in patients with HANE, they are not unduly susceptible to infection. Why not? The alternative pathway of complement activation is intact and these are compensated for by the potent amplification step from the alternative pathway. 6. How might you decide the background of the laryngeal edema (HANO or anaphylactic reaction)? If the laryngeal edema is anaphylactic, it will respond to epinephrine. If it is due to HANO, it will not, C1INH needed. PAROXYSMAL NOCTURNAL HEMOGLOBINURIA (PNH) • Acquired clonal mutation of PIG-A gene in myeloid progenitors – no GPIenchored proteins in the cell membrane of affected cells (rbc, plt, wbc) • CD59 and CD55 complement regulatory proteins are GPI-enchored proteins • No CD59 and/or CD55 PNH patients are highly susceptible to complement-mediated lysis • The lysis of red blood cells leads to high levels of hemoglobins in the blood that appears in the urine (hemoglobinuria) • Elevated levels of TF derived from complement-damaged leukocytes cause thromboses Change in the colour of urine samples taken from PNH patient during the day Paroxysmal nocturnal hemoglobinuria (PNH) symptoms and therapy • Haemolytic anaemia and associated symptoms • Specific th.: eculizumab (Soliris) - anti-C5 monoclonal antibody • Haemoglobin and its products in the urine • Curative th.: bone marrow transplantation • Thrombosis: • Alternative th.: steroids (general immunosuppression) – brain veins, – mesentheric veins, – hepatic veins (Budd-Chiarisyndrome) • Chance of transformation to acut myelogenous leukemia (AML), aplastic anaemia, myelodisplastic syndrome (MDS) • Anticoagulants: sc. heparin p.o. kumarin • Iron replacement • Transfusion (filtered-irradiated blood) Abbreviations C1Inh: inhibitor of C1 and MBL (serin protease inhibitor – multiple effects) α2-macroglobulin: inhibitor of MBL C4bp: C4 binding protein - inhibitor of the classical C3 convertase Factor H: inhibitor of the alternative C3 convertase Factor I: cleaves C4b and C3b Properdin: stabilizes the convertases of the alternative pathway DAF (CD55): Decay Accelerating Factor (of C3 convertases) MCP (CD46): Membrane Cofactor Protein, cleavage of C3 convertases with factor I CR1: complement receptor 1, inhibitor of C3 convertases CD59 (MIRL): Membrane Inhibitor of Reactive Lysis – inhibits binding of C9 to C8 HRF: Homologous Restriction Factor (inhibits binding of C8 and C9)