surgical team
advertisement

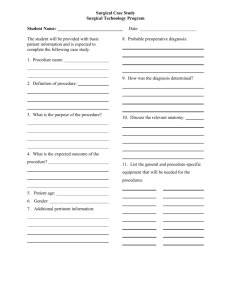
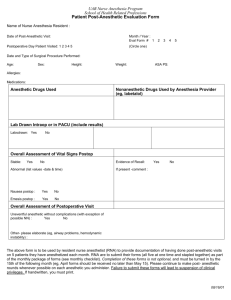
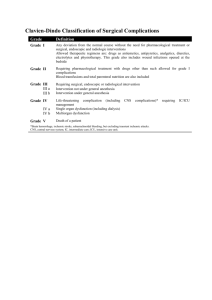
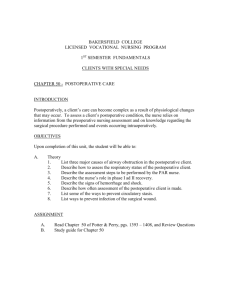
INTRAOPERATIVE PHASE Intraoperative Phase - Transferred to OR-ends with the transfer to the recovery area. • Transfer onto the operating table • Phases of anesthesia • Operative proceedure • Transfer from operating table to stretcher • Safe transport to post-operative area (PACU) SURGICAL TEAM • Surgeon • Anesthesiologist • Scrub Nurse • Circulating Nurse • OR techs Surgical team • Surgeon-responsible for determining the preoperative diagnosis, the choice and execution of the surgical procedure, the explanation of the risks and benefits, obtaining inform consent and the postoperative management of the patient’s care. • Scrub nurse- (RN or Scrub tech )- preparation of supplies and equipment on the sterile field; maintenance of pt.s safety and integrity: observation of the scrubbed team for breaks in the sterile fields; provision of appropriate sterile instrumentation, sutures, and supplies; sharps count. Surgical team • Circulating Nurse - responsible for creating a safe environment, managing the activities outside the sterile field, providing nursing care to the patient. Documenting intraoperative nursing care and ensuring surgical specimens are identified and place in the right media. In charge of the instrument and sharps count and communicating relevant information to individual outside of the OR, such as family members. Surgical team • Anesthesiologist and anesthetist- anesthetizing the pt. providing appropriate levels of pain relief, monitoring the pt’s physiologic status and providing the best operative conditions for the surgeons. • Other personnel- pathologist, radiologist, perfusionist, EVS personnel. Nursing Roles: Staff education Client/family teaching Support and reassurance Advocacy Control of the environment Provision of resources Maintenance of asepsis Monitoring of physiologic and psychological status Elements of Aseptic Technique *Sterile gowns and gloves. *Sterile drapes used to create sterile field. *Sterilization of items used in sterile field. Surgical asepsis • • • • The absence of pathogenic microorganisms. Ensure sterility Alert for breaks The practice of aseptic technique requires the development of sterile conscience, an individual’s personal honesty and integrity with regard to adherence to the principles of aseptic technique. Preanesthetic Preparation • Avoidance of foods and drink prevents passive regurgitation of gastric contents • Clients should typically continue medications up to surgery • Consent must be received Sedation • Reduction of stress, excitement, or irritability and some suppression of CNS • Typically used to relieve anxiety and discomfort during a procedure • Residual effects include amnesia and letheragy Types of Anesthesia • Regional Local Nerve block Epidural Spinal • General Spinal Anesthesia • Injected into cerebrospinal fluid (approx L 3-5) subarachnoid space • Indications surgical procedures below the diaphragm -patients with cardiac or respiratory disease • Advantages -mental status monitoring -shorter recovery • Disadvantages -necessary extra expertise -possible patient pain • Contraindications -coagulopathy -uncorrected hypovolemia - Spinal Anesthesia • Involved medications -lidocaine -bupivacaine -tetracaine • Patient assessment -continuous heart rate, rhythm, and pulse oximetry monitoring -level of anesthesia -motor function and sensation return monitoring Spinal Anesthesia • Complications -hypotension -bradycardia -urine retention -postural puncture headache -back pain Spinal Anesthesia (Subarachnoid Block) • Anesthesia: tip of xiphoid to toes • Risks: – Loss of vasomotor tone – “Spinal Headache” – Infection, Rising anesthesia above diaphragm • Nursing: KEEP FLAT, MONITOR VS & OFFER FLUIDS WHEN APPROPRIATE General Anesthesia • Inhalation-Mask, Endotracheal tube (ETT) or Laryngeal managed airway (LMA) • Intravenous • Combination General Anesthesia: Inhalation Agents • Inhalation most controllable method; lungs act as passageway for entrance & exit of agent • Gas Agents : Nitrous Oxide – must be given with oxygen – require assisted to mechanical ventilation – frequently shiver – taken in & excreted via lungs – Examples: halothane, enthrane, florane… Adjuncts to General Anesthesia • Hypnotics (Versed, Valium) – also used for conscious sedation • Opioid Analgesics (morphine, Demerol) – respiratory depression • Neuromuscular Blocking Agents – Causes muscle paralysis – Examples: Pavulon, Succinycholine – What vital function is affected? Potential General Anesthesia Complications • Overdose (consider risk factors) • Hypoventilation postoperatively • Intubation related: sore throat, hoarseness, broken teeth, vocal cord trauma • MALIGNANT HYPERTHERMIA – Genetic predisposition – Triggered by anesthetics such as Halothane Potential Intraoperative Complications Nausea and vomiting Anaphylaxis Respiratory complications Inadequate ventilation, airway occlusion, intubation of the esophagus, and hypoxia Hypothermia Malignant hyperthermia Disseminated Intravascular Coagulation What are measures to prevent or treat these complications? Nursing Interventions Communicating plan of care Identifying nursing activities Establishing priorities Coordinate care with team members Coordinate supplies and equipment Control environment Document plan of care Intraoperative Nursing Care Nurses are responsible for managing six areas of risk: • Risk of infection related to invasive procedure and exposure to pathogens. • Risk for injury related to positioning during surgery. • Risk of injury related to foreign objects inadvertently left in the wound. • Risk for injury related to chemical, physical, and electrical hazards. • Risk for impaired tissue integrity. • Risk for alteration in fluid and electrolyte balance related to abnormal blood loss and NPO status. Nursing Process Intraop Phase • Intervention – Safety – Advocacy – Verification – Counting-instruments, sponges, needles Altered Skin Integrity • How many sutures? • Staples or sutures or glue??? POSTOPERATIVE PHASE • Postoperative - Begins with transfer to PACU and ends with the discharge of the patients from the surgical facility or the hospital. • Nursing Interventions Communicating pertinent information about surgery to the PACU staff. Postoperative evaluation in clinic or home. Nursing assessment in the Recovery Room • Vital signs- presence of artificial airway, o2 sat,BP,pulse, temperature. • Ability to follow command, pupillary response • Urinary output • Skin integrity • Pain • Condition of surgical wound • Presence of IV lines • Position of patient Immediate Post-anesthesia Care • Airway • Breathing • Circulation How often should vital signs be assessed? Postop SKIN Assessment “Altered Skin Integrity” • Day 3 or so to Day 14 (or 21 or more) – Proliferation: fibrin strands form scaffold • Collagen with blood = granulation tissue • Protect from damage or stress – No lifting, heavy exercise, driving etc. • At risk for dehiscence or evisceration • Day 15 (or weeks, months, years) – Scar is organized, less red, stronger – Max strength = 70 – 80% Postoperative RESPIRATORY Assessment • Impaired gas exchange or impaired airway clearance • Risks: pneumonia, atelectasis • Assessment: – Open airway – Pulse oximetry (what is normal?) – Check opioid use (why?) – Monitor quality & quantity of respirations Postoperative RESPIRATORY Assessment • Interventions: – Turn (also relates to cardiovascular risk – any ideas?) – Deep breathe & cough – Incentive spirometry – In-bed exercises (see text) – AMBULATION!! Postop SKIN Assessment “Altered Skin Integrity” • Wound healing – How is the face healing time-line different from the foot? • OR to Day 2 (may 3-5) – Inflammation vs. infection • redness, pain, swelling, warmth • skin held together by blood clots & tiny new blood vessels – Avoid pressure/ be sure to splint Postop CARDIOVASCULAR Assessment: Potential for hypoxemia • Think (hypovolemic) shock (hemorrhage) – Assessment: • Prevention of venous stasis – Who is at risk? – What should be done? Avoiding Venous Stasis • Avoidance of positions leading to venous stasis • In Bed Exercises • Antiembolism stockings • Sequential Compression Device • When all is said & done, AMBULATION is the best! Postop NEUROLOGIC Assessment • Assess cerebral function – Think elderly • Assess motor/sensory function Postop F & E Assessment • Fluid Status – Intake – Output • Why would a postop client need an IV?? Postop URINARY Assessment • Anuria (define) • Urinary Retention – Or Urinary retention with overflow • Differentiate • Intervention: – Fluids – AMBULATION – Careful monitoring Postop GI Assessment • Nausea & vomiting • Assessment of peristalsis/paralytic ileus • Interventions: – N/G tube, GI rest (NPO), AMBULATION • Postop Diets – Why are clear liquids usually the first diet? – What does “advance as tolerated” mean? – What are nursing responsibilities?? Postoperative Diets • • • • • 1. Clear Liquid 2. Full Liquid 3. Soft 4. Regular Postop Diets – Why are clear liquids usually the first diet? – What does “advance as tolerated” mean? – What are nursing responsibilities?? Postop SKIN Assessment “Altered Skin Integrity” • • • • • • R edness E dema E cchymosis D rainage A pproximation Is a scar as strong as the original skin? The Ultimate in “Altered Skin Integrity” • Risk factors: -Dehiscence -Evisceration • Prevention: -Wound Splinting -Abdominal binder -Diet Nursing Diagnosis • Ineffective airway clearance- increased secretions 2 to anesthesia, ineffective cough, pain • Ineffective breathing pattern- anesthetic and drug effects, incisional pain • Acute pain • Urinary retention • Risk for infection Postoperative Goals • Re-establishment of physiologic equilibrium • Alleviation of pain • Prevention of complications Postoperative Management • • • • • Maintain a patent airway Stabilize vital signs Ensure patient safety Provide pain Recognize & manage complications When caring for post-surgical patient, think of the “4 W’s” • Wind: prevent respiratory complications • Wound: prevent infection • Water: monitor I & O • Walk: prevent thrombophlebitis Complications • Respiratory- atelectasis, pulm. Embolus • Cardiovascular- venous thrombosis • Gastrointestinal-Hiccoughs, N/V,abd. Distention, paralytic ileus, stress ulcer. • GU- urinary retention • Hemorrhage-slipping of a ligature(suture) • Wound infection• Wound dehiscence and evisceration- Postoperative Pain Control • What is the definition of Pain? • As nurses, what do we need to remember about the pain experience? • What is the key reason to control postoperative pain?