SOCIAL RESOURCES FOR THE ELDERLY
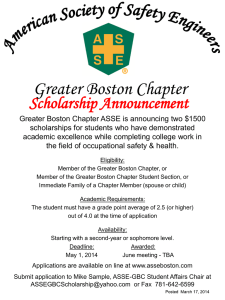
advertisement

Community Resources for Boston Elders Boston University Geriatric Services Catherine Fabrizi, MSN, APRN, BC Ellen Harrington, MSW, LICSW Patricia Kimball,RN, MS, BC Maureen Russell, RN, MPH, BC Purpose and Objectives Identify the community resource providers that oversee homecare and home health care in the Boston area. Assist patients in accessing home services. Describe basic Medicare and MassHealth eligibility and coverage. Discuss various housing options available to seniors in Boston and understand the eligibility requirements as well as services provided ~ Home-Based Services ~ Benefits & Insurance ~ Housing CASE 1 – 74 y.o. non-english speaking obese Haitian woman OA hips, knees, lumbar spine; HTN; urinary incontinence; h/o falls lives alone, cluttered studio apt., BHA senior building w/ elevator difficulty ambulating d/t pain cruises around apt. instead of using cane/walker; has w/c but cannot self propel depressed needs assist with ADLs and IADLs limited family support medicare and mass health (medicaid) What service plan would you design to help maximize function, minimize pain, increase socialization and meet all ADL/IADL needs? How will it get paid for? Aging Services Access Points “ASAP” 3 “ASAPs” cover Boston geographic areas. -Central Boston Elder Services (CBES) -Boston Senior Home Care (BSHC) -ETHOS (point of referral for adult protective services) Funded through the Executive Office of Elder Affairs -100% state funded with some additional federal funds Offers a package of home care services Provides case management services Eligibility and cost based on income and need Anyone can refer by calling: ELDER INFO (617) 292-6211 Services Provided by ASAPS Care Coordination Personal Care Homemaking Grocery delivery Laundry Service Personal Emergency Response System (PERS) Adult Day Health Home Delivered Meals Nutrition supplements Money management Home safety equipment Medical Transportation Volunteers –medical escort Caregiver Support /Respite Criteria for “ASAP” Eligibility 1. Age 60 or > (or under 60 if dx. of dementia & needs respite) 2. Functional impairment - ADL and IADL needs 3. Income single person <$ 1732.00/month couple <$ 2,450.00/month 4. Agrees to co-pays – ($7-$135.00/month) MassHealth members financially eligible -no co-pays 5. Respite needs – income exemptions may apply ASAP SERVICE PLAN (EXAMPLE- $230.00/month) Personal Emergency Response System Home Delivered Meals (20/month) Homemaking, 3 hours q 2 weeks $30 $95 $105 Service plans are individualized based on CM assessment of functional impairment level. Service packages are provided thru various programs within the ASAP based on need/income and even living situation (ie. GAFC in senior buildings, respite for caregivers) Certified Home Health Agency (“VNA”) Standard Services Skilled Nursing Physical Therapy Occupational Therapy Home Health Aides Other Contracted Services Medical Social Work Speech Therapy Nutritionist Community Resource Specialist Criteria for CHHA Eligibility Skilled nursing or physical therapy need -cannot refer just for nutrition, speech, OT or SW Insurance MD/NP orders Short term / intermittent monitoring / therapy needs 60 day certification period Payment Sources for Certified Home Health Agency Services • MEDICARE A • Covers100% of skilled care provided by RN/PT/OT/ST/SW as long as pt meets skilled level of care. • MASSHEALTH (MEDICAID) • Covers 100% all services if medically necessary • PRIVATE PAY • Patient may have out of pocket expenses if care not qualified as skilled or if there is no secondary insurance • COMMERCIAL • Coverage depending on individual plans MassHealth And I thought there were only two kinds ! Thirteen programs offered in Massachusetts Mass Health Standard: • age 65+ and income less </= to 100% federal poverty level ($8,960) • assets of less than $2,000/ind., $3,000/couple SSI Recipients –automatically eligible Former SSI recipients ages 65+ same as above Benefits/Covered Services MassHealth Standard Inpatient Hospital Services Outpatient Services Medical Services For 65+ entitled to Medicare A, Division of Medical Assistance will also pay for the cost of the Medicare A&B premiums as well as deductibles and coinsurance amounts Medical equipment and supplies Transportation Services Adult Day Health Foster Care Adult Day Health Centers Medical Model Supervised setting for qualified elders with skilled needs to receive medical, nursing, social and nutritional services such as: -health screening/monitoring, -teaching -counseling -medication assistance/monitoring -rehabilitative therapies. Mission: keep elder in the community by providing structure & social stimulation thru recreational & cultural activities as well as providing respite, support, counseling for caregivers. •May be covered by mahealth, ASAP, SCO, some LTC ins. or private pay (NOT COVERED BY MEDICARE) ADH Programs in Boston Area Ellis Memorial (Southend) Alianza (Roxbury) Cape Verdian (Dorchester) Laboure (South Boston) Golden Age Center (Chinatown) Rogerson (Roslindale) Rogerson (Brookline) Rogerson (at Egleston) Kit Clark (Codman Square) Kit Clark (Fields Corner) Greater Boston Guild for the Blind (JP) Cooperative Elders (Milton) May Institute (geri-psych) Volunteer Programs Little Brothers Friends of the Elderly MatchUp Interfaith Volunteers Kit Clark Senior Services ASAPs Congregations Commission for the Blind Case 2 - 82 y.o woman s/p CHF exacerbation and pelvic fx now being d/c’d from rehab. HTN; AFIB; OA; COPD; mild dementia lives alone, senior building new functional/cognitive decline: needs assist with ADLs/IADLs involved daughter but cannot provide 24hr care; assists with $, shopping, errands etc. caregiver stress- daughter cares for grandkids too daughter wants pt to consider alt. living but pt wants to go home medicare managed care thru TUFTs What is necessary for a safe d/c plan that maximizes function and ensures safety? How will it be paid for? Medicare Medicare is a federal health insurance program Eligibility: 65 years of age, or certain individuals with disabilities under 65 and any person with kidney failure on dialysis. Program overseen by CMMS (Centers for Medicare and Medicaid Services) PPOs and HMOs Medicare Part A Medicare A Covers inpatient hospital care some skilled nursing facility care hospice care certified home health agency Medicare Part B enrollee must be eligible for part A enrollee must apply –it is not automatic monthly premium required covers most physician/NP outpatient care; diagnostic x-rays and lab tests, outpatient therapy, some durable medical equipment and flu/pneumonia vaccines Medicare D Housing Options Public (BHA) senior buildings Privately owned and managed senior buildings Private home Supportive Housing Ana Bissonette House Congregate Living Tuttle House Assisted Living Group homes Group adult foster care Roxbury Community Adult Foster Care Program Continuing Care Retirement Community Lasalle Village - Newton Rest Homes Mount Pleasant and Hale House Nursing Home What is public housing? Public housing provides safe and affordable rental housing for eligible low-income families, the elderly, certain veterans and people with disabilities whose income does not exceed 80% of the area median income. People who live in public housing are expected to pay 30% of their household income towards rent. Median income of Boston residents: $38,691 Eligibility- Family of 1: $16,000 annual income Family of 2: $18,300 1701 Washington Street Boston Housing Authority Eligibility for Elderly Housing • • • • Age 62 or older Rent is 1/3 of income All utilities included except cable and phone Waiting period for prime locations is 2+ years. Some up to 5 years Priority is homelessness: • Residing in shelter • On the street • Evicted from residence deemed not fit for human habitation • Eviction papers with specific date of eviction • Waiting for public housing can be 3-6 months Ruggles Assisted Living Assisted Living Provides housing, meals and personal care services to adults ALs do not provide medical or nursing services Not designed for individuals that need serious medical care Intended for adults that need help with ADLs/ IADLs AL provides comfort of 24-hour security and assistance Costs range from $3,000 a month and upwards Individuals may receive subsidies, permitting low-income individuals to afford the monthly rate Residences have single and shared apartments with efficiency kitchens lacking oven space, but stove tops and microwaves. Some assisted living facilities have specialized dementia programs Note: Resident Care Director is usually an RN, but not permitted hands on nursing care as most people think but rather to supervise the aides Standish Village at Lower Mills Other Programs for Elders Program of All Inclusive Care for Elders (PACE) Senior Care Options (SCO) Personal Care Attendant (PCA) -Toward Independent Living and Learning (TILL) -United Cerebral Palsy (UCP) PACE Program of All-inclusive Care for the Elderly (AKA: ESP -Elder Service Plan) 1. PACE is a fully capitated medicare and medicaid managed care program which serves frail individuals age 55 and over who meet NH clinical criteria and who are able to remain in the community with supports 2. PACE sites utilize an interdisciplinary team of clinicians in an expanded adult day health model to provide and manage all health, medical and social service needs. Senior Care Options (SCO) SCO is another fully capitated medicare and medicaid managed care program that is offered to eligible MassHealth members age 65 and over at all levels of need, both community and institutional settings SCO organizations establish large provider networks which coordinate and deliver all acute, primary care, LTC, mental health services to enrollees with a geriatric model of care. SCO provides flexible funding vehicle to manage the delivery of all components of enrolled seniors medicare and medicaid covered services Promotes improved access for enrolled seniors to the most appropriate and necessary services Provides enrolled elders with access to healthcare, triage, and advice 24 hours a day, 7 days a week PCA Programs (personal care attendant) PCA services are for those who need daily assistance in meeting personal care needs. With PCA help a person can live independently in their home. PCA -assists with ADLs & IADLs -assists with health related functions - delegated by consumer under the direction of a licensed health care professional (i.e. catheter care, home glucose monitoring) PCA programs are consumer driven and managed by consumer Eligibility 1. Medicaid subscriber 2. Medical necessity 3. Person must be able to make decisions about his/her own care or have a responsible party who can make those decisions 4. MD must order the services PCA Programs in the Boston Area Toward Independent Living and Learning (TILL) United Cerebral Palsy (UCP) ASAPs Boston Center for Independent Living (BCIL) Other Resources Elder Law Attorney Boston Elder Legal Services Financial Advisors Guardianship Programs Money Management Adult Protective Services / Elders At Risk Private Care Managers Transportation -Senior Shuttle -The RIDE WHEN IN DOUBT CALL: ELDER INFO 617-292-6211 OR ElderINFO.org CASE 1 Mrs. T is a 74 y.o. non-english speaking obese Haitian woman with OA of hips, knees and lumbar spine; HTN; urinary urge incontinence and h/o falls followed by Geriatrics Home Care Team. She lives alone in a cluttered studio apartment in a Boston Housing Authority (BHA) senior elevator building. While she transfers independently using walker or quad cane she has difficulty ambulating alone d/t chronic back/hip/knee pain. Usually she “cruises around apt”. She limits going out b/o pain and ambulation difficulties thus is becoming isolated and depressed. Mrs T. has a standard manual wheelchair which she does not use because she is unable to self-propel. In addition to impaired mobility, she needs help with most ADL’s and IADLs d/t OA and related chronic pain. She has 1 son who visits on weekends. But no other supports. She has medicare and mass health (medicaid). What service plan would you design to help maximize function, minimize pain, increase socialization and meet all ADL/IADL needs? How will it get paid for? Case 2 Ms. S is an 82 y.o woman with HTN, Afib, CHF, OA, COPD and mild cognitive impairment who lives alone in a south end senior building. Her daughter who lives nearby is very involved. She assists with IADLs but she cannot provide 24 hr care or assist with daily ADLs b/o providing child care for 2 grandchildren while her daughter works. Ms. S was recently hospitalized with a fall d/t CHF exacerbation after forgetting to take her lasix for few days and is now returning home from a short rehab stay. She has a healed pelvic fracture and is walking short distances with a walker but needs assist with bathing, dressing and grooming. She cannot stand long enough to cook meals or clean. She has medicare managed insurance thru Tufts. Prior to hospitalization pt was independent with ADLs and had a HM 1 day/wk for cleaning/laundry. And she was attending the lunch program in the building daily. Daughter took pt shopping on weekends and assisted with banking/finances. Given Ms. S’s recent functional and cognitive decline daughter is worried about her ability to live alone and would like to consider alternative living options but Ms S is adamant about going home. You are involved in planning Ms. S’s discharge from rehab – what care plan would you design to maximize function; ensure supervision and safety? Who would you involve in the discharge planning? How will services be paid for? Case 3 Mrs C is an 92 y.o. woman with HTN, DM, hypothyroidism, COPD, mild cognitive impairment and depression who was referred to geriatrics from her PCP b/o difficulty getting to appts. Pt suffered a stroke over 1 year ago and has made remarkable progress with PT, OT, speech therapy. She is able transfer safely with 1 person assist and walk short distances. She spends most of they day in her w/c. She is occasionally incontinent but it is more related to functional impairment and urgency. She can feed self soft foods but does not take in enough calories by mouth so tube feedings continue. Until now she has had a HHA 3 days/week for 1 hr each to assist with bathing. Her son Thomas is the primary caregiver who manages meds, feedings, personal care when no HHA and all IADLs. He never leaves her alone d/t safety concerns. While his sister visits weekly for 1-2 hrs she does not help with ADLs. Thomas has missed his own medical appts b/o not wanting to leave pt alone. Mrs C has medicare and medicaid. She is on15 medications requiring copays. She will be losing the HHA now that the CHHA will be terminating therapies. A referral was made to the area ASAP but the CM could only offer PC/HM 1-2 hrs daily. On your initial assessment you identify major caregiver stress and you are concerned about pt’s son neglecting his own health. While the other case studies examples demonstrate services options which will aid the pt and decrease stress on caregivers there are other programs which provide additional support to pts who require a lot of care and are nursing home eligible but want to remain living at home. What services would help this patient remain safely living at home and decrease caregiver stress?