Cardiorenal Syndrome
advertisement

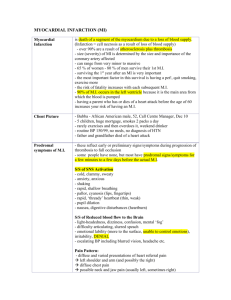
Combined renal dysfunction and heart failure: CARDIORENAL SYNDROME Richard Swartz MD University of Michigan – Nephrology & Palliative Care rswartz@umich.edu Cardiorenal Syndrome . . . - 60 yo M – Hx CAD (MI & stent), Afib & Vtach (AICD), COPD, IDDM, CKD Chest pain, mild fever and cough, increased edema, CXR w CHF LVEF 25% and creat 2.7 (both worse), Uo < 1000ml/d, BNP 7000 Adm Meds: 160mg furosemide, b-blocker, ACEi, ASA & statin - Dopamine + adm meds, creat up 3.8, BNP 10,000 Uo not improving, UNa 10, FENa 0.5%, no protein or RBC in urine Rx w IV dobutamine milrinone, furosemide (cont infusion) Over 2 -3 days CHF s/s improve, creat 1.9 - Ectopy develops, ? Ischemia, heart cath after N-acetylcysteine - no new coronary lesions found, but Uo falls and creat rises Cardiorenal Syndrome - a description: ** SPECIFIC: “decreased (> 25%) GFR, increased creatinine (> 0.5) , in the setting of CHF & aggressive diuresis” ** GENERAL: combined heart and kidney disease in which too much fluid ADHF/CHF too little fluid acute azotemia/”volume depletion” CHF ADHF ACS Congestive Heart Failure Acute Decompensated Heart Failure Acute Coronary Syndrome (ischemia) ARF AKI Pre-renal acute renal failure (“old” term) acute kidney injury (“new” term) physiologic decrease in GFR Clinical Impact of ADHF/CHF • CHF: prevalence is 2-3% in USA • ADHF: re-admission rate > 50% mortality > 20% annually • ADHF: associated w ARF/AKI in 20-45% mortality higher w AKI (Additional risks ~ age, DM, HTN, ACS) Clinical Impact of AKI/ARF AKI/ARF – incr creatinine, decr GFR, +/- oliguria 2 to 5% hospitalized patients w some degree of AKI/ARF increases risk of in-hosp mortality > 2-fold 0.2 to 1% hospitalized patients w severe AKI/ARF & dialysis in-hospital mortality is 50% overall and 70% in ICU AKI/ARF seldom occurs in a vacuum and usually is a complication rather than a disease entity ATN (tubular injury, “shock”) or PRE-RENAL > 80% GN, vasculitis, vasculopathy, AIN ~ 10% Obstruction ~ 5-10% “CARDIORENAL SYNDROME” Pump Failure Heart Failure Vicious Cycle Fluid Retention Kidney Failure The heart affects the kidney, which affects the heart, which . . . “Something goes around something, but that’s as far as I got.” Possible pathophysiologic in cardiorenal syndrome (???) FROM: Nat Rev Nephrol. 2013 Feb;9(2):99-111 Another way of looking at it . . . Better ?? • Cardiorenal 1 – acute ; cardiac dysf is primary AMI, dysrhythmia, pericarditis (AKI vs Pre-renal dysf) • Cardiorenal 2 – chronic ; cardiac dysf is primary CMP, congenital heart dis, HTN w LVH (CKD vs Pre-renal) • Renocardiac 3 – acute ; kidney dysf is primary AKI, obstr, pre-renal (HTN, vol retention, CHF, symp & RAAS dysf) • Renocardiac 4 – chronic ; kidney dysf is primary CKD (HTN, poor vol control, anemia, vasc calcif, hyperlipidemia) • Cardiorenal 5 – other systemic disease is primary Amyloidosis, cirrhosis, collagen-vasc disease Hemodynamic, renal function, plasma hormones, and body fluid compartment data in untreated congestive heart failure. Anand I, CJASN, Jul 2013 200% increase in LA pressure RV pressure ©2013 by American Society of Nephrology Potentially Treatable “Cardiorenal” Factors • Volume accumulation & high or low BP • Increased RAAS w mineralo-corticoid activity • Increased sympathetic activity • Cardiac support – RBF delivery, Pulm HTN • Anemia (Hgb) • Avoiding nephrotoxicity Diuretics (volume control) • • • • Thiazide - HCTZ, metolazone, indapimide Loop - furosemide, bumetanide, torsemide, ethacrynic acid “K-sparing” - spironolactone, eplerenone, amiloride Acetazolamide, nesiritide Diuretic resistance limits effectiveness: volume contraction, hypotension (decreased BP & GFR) incr RAAS & sympath activity, renal “edema”, met alkalosis Rx: measure PCWP (BNP) to assess impact of central volume incr doses of loop agents cont IV infusion combined loop + thiazide Rx tolvaptin, acetazolamine, +/- albumin ULTRAFILTRATION – if all else fails, but NOT as primary Rx ** severe intrinsic parenchymal ARF/AKI w oliguria DIALYSIS Rx** RAAS modulation (nl or high BP) • • • • Renin inhibitors (aliskerin) ACE inhibitors (lisinopril) Angiotension-receptor blockers (losartan) Aldo-receptor blockers (spironolactone or eplerenone) Limitations: Hyperkalemia Hypotension Decreased RBF Worse ARF/AKI Sympathetic blockers (nl or high BP) • • • • Beta-blockers (type, duration of action) Alpha-blockers (for HTN control) Combination agents (labetolol) Other central agents (clonidine) Limitations: Hypotension, reduced renal perfusion Vasodilators (periph resistance) • • • • Calcium-channel blockers Direct vasodilators (hydralazine, minoxidil) Milrinone, dopamine or dobutamine Nitrates, nitroprusside Limitations: Hypotension, reduced renal perfusion Pressors, Inotropes, Hemodynamic Support • • • • Midodrine PO Alpha-sympathetic agents IV Vasopressin IV Endothelin inhibitors PO • • • • • • Digoxin Adenosine-receptor blockers (rolofylline for RBF) Pulm arteriolar dilators (riociguat for PHT) Calcium agonists (levosimedan as inotrope) Erythropoietin and/or transfusion N-acetylcysteine (as periph vasodilator) Some “News” from Recent Literature Comparative studies show no advantage of extracorporeal ultrafiltration vs medical Rx (diuretic plus hemodynamic meds) for survival or further AKI (NEJM 2011) Erythropoietin to boost Hgb in CHF does not improve survival or CHF readmission rate, but does increase thromboembolic events by 50% (NEJM 2013) N-acetylcysteine (for endothelial dysf) improves forearm blood flow but not the degree of CHF or BNP level (Heart Lung Circ 2012) BNP level predicts progression of CKD to ESRD, but nesiritide does not improve outcome in severe CHF (Neph Dial Transpl 2012) Vit D normalization may improve CHF (& reduce CRP), but large osteoporosis studies do not show the same effect (Cong Ht Fail 2103; Osteopor Internat 2013) Fatal & Non-fatal Events in ESRD ~ B Lines on US SURVIVAL % Zoccali et al, Clin J Amer Soc Neph, 2013 DAYS Cardio-renal Syndrome Limitations of Medical Rx in Cardiorenal Syndrome • • • • • Oliguria – refractory to diuretics, UF required Hypotension – limits RBF and GFR pharmacoRx Hyperkalemia – limits some medications Uremia – ultimately requires dialysis Rx Suitability for advanced cardiac support Dialysis - Renal Replacement Therapy (RRT) • Simple ultrafiltration (fluid removal) if diuretics fail No clearance of urea, K, phos, other solutes • Intermittent Hemodialysis for fluid & uremic s/s Often lowers BP; intervals w fluid reaccumulation • Continuous RRT (dialysis + hemofiltration) Limited to ICU Rx for combined resp failure, hypotension, oliguria • Peritoneal dialysis Combination of ascites, low BP & poor CO, recurring CHF • Palliative Care – when enough is enough ? Morphine … PD in Cardiorenal Syndrome 64 yo M, w CABD 1999, progressive CMP, AICD Jun09, recurring hosp adm for CHF PEA arrest Apr10 and VT w ICD shock Sep 2010 Progressive CKD, BUN 180 & creat 3.2 in Oct 2010 HD initiated w low BP and cont fluid overload (incl ascites) PD successfully initiated, trained for home self care Dec 2010 Improved overall clinical status, control of edema & ascites no further hosp adm for vol or CHF complications return to part-time work & primary care of chronically ill wife BNP 1200-3800 on HD, then 700 in 2011, 370 in 2013 on PD Cont PD self care through Aug 2013 (PVOD, gangrene, died) “Palliative” PD in Cardiorenal Syndrome A 43-yr-old man with congenital heart disease and stroke, presented with refractory CHF, low BP and renal failure (BUN 150, creat 4; both rising). He was continuously dyspneic even when kneeling at his bedside. His sister was his care provider and decision maker. We discussed comfort care with Hospice support but also discussed dialysis (HD would risk hemodynamic chgs, and PD would require home-based care). They deferred any new decision in favor of continued supportive cardiac infusion at home. He returned within a few days with cont’d distress and worse renal failure. A time-limited 1-2 wk trial of PD was begun – improving his CHF so that he could walk, sleep in bed, and function at home. He continued PD successfully for > 14 months, eventually developing refractory arrhythmias that required ICU treatment. When intubation became the only remaining option, his sister chose to withdraw support and he died quietly with his sister and mother at the beside. In the end, Ed, most of us are carried along by our delusions But often we don’t have all the answers. How many ways can you say “I don’t know” ? “it’s a virus” “it must be genetic” “let’s see what happens” “needs further evaluation” “several causes likely” multifactorial idiopathic inherent idiosyncratic essential occult primary agnogenic cryptogenic A Few Recent Reviews Anand I. Cardiorenal syndrome: a cardiologist’s perspective. Clin J Amer Soc Nephrol, Jul 2013. House A. Cardiorenal syndrome: new developments in understanding and pharmacology. Clin J Amer Soc Nephrol, Aug 2013 Kim C. Cardiorenal syndrome. Electrolytes & Blood Pressure, Jun 2013.