Management of Life-Threatening Opioid Neurotoxicity
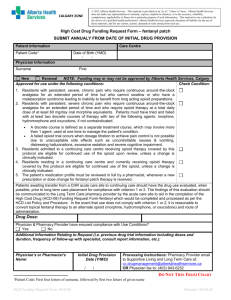
advertisement
Management of Life-Threatening Opioid Neurotoxicity Why Are We Seeing More Opioid Induced Neurotoxicity? • There has been a 3x increase in morphine consumption worldwide from 1986 to 1995 • There has also been an increase in reports and awareness of neuroexcitatory side effects (allodynia, hyperalgesia, myoclonus, seizures) of morphine and hydromorphone • As we succeed in educating and encouraging health care providers to be aggressive in pain management, we can expect to see more opioid-induced neurotoxicity Opioid Induced Myoclonus • Myoclonus: sudden, brief, shock-like involuntary movements caused by muscular contractions • All muscle groups • Often best observed when patient sleeping • Incidence of opioid-related myoclonus varies from 2.7% to 87% • Most recognized with metabolites of morphine (particularly M3G), however also seen with opioids with no active metabolites (methadone, fentanyl) CASE PRESENTATION Ms. W.P. 73 yo woman with met. NSCCL Dx. early Oct. 2001 – Seen Oct. 18/01 by oncology in community hospital ER with low back pain, dyspnea – At that time: morphine long-acting 200 mg bid plus morphine 2.5 mg IV push q3h (pr,, but given regularly) – Morphine long-acting increased to 300 mg bid, with plans for 300 mg tid, plus 5 mg IV q3h prn – Over the next 2 days became twitchy on morphine, changed to hydromorphone infusion – Over the subsequent 2 days, hydromorphone increased from a few mg/hr to 30 mg/hr, with no improvement in distress – Increase in agitation, fluctuating LOC, non-stop myoclonus Case presentation ctd. Oct. 22/01 – transferred to SBGH palliative care On exam at time of transfer (approx 1330h): – Lethargic, disoriented, restless, emaciated. – Resps. approx 20, reg. – Pupils 3-4 mm, reactive – Generalized myoclonus… non-stop – Lab: Oct. 19/01: Creat 50 μmol/l (60-110) BUN 2.9 mmol/l (2.5-6.1) Oct. 22/01: Creat 47 μmol/l (35-97) BUN 2.9 mmol/l (2.7-7.1) lytes, Ca++ normal – Assessed as having severe opioid neurotoxicity, with risk of seizures. Case presentation ctd. – Hydromorphone D/Cd – NS 500 ml IV bolus, followed by NS with KCl 10 mEq/l 250 ml/hr IV. (This was decreased to 200 ml/hr overnight, D/Cd Oct 23 1300h) – Furosemide 40 mg IV q8h – Lorazepam 0.5 mg IV push x1 dose @ 13:45h – Sufentanil 5 μg IV push x1 dose @ 14:25h – Sufentanil 10 μg/hr IV infusion started mid-afternoon Oct. 22 → 20 μg/hr Oct. 23 Breakthrough = sufentanil 25-50 μg SL q 30 min prn. Received total breakthrough of 75 μg Oct. 22 and 250 μg Oct. 23 – Midazolam 2.5 – 5 mg SQ q1h prn (needed just 1 dose, Oct. 23) – Marked improvement in myoclonus by 1700h Oct. 22 Case presentation ctd. – Methadone 10 mg bid added Oct 25 → 15 mg bid Oct 26 at which time sufentanil DCd. – Max methadone dose was 25 mg bid, Nov. 07 – Consider: hydromorphone 30 mg/hr SQ = 720 mg/day ≈ 3600 mg/day SQ morphine if a 5:1 ratio used ≈ 7200 mg/day po morphine Ripamonti et al J Clin Oncol 1998: #mg po Morphine/day Morphine:Methadone 30 – 90 3.7 : 1 90 – 300 7.75 : 1 > 300 12.25 : 1 – Calculated methadone equivalence to 7200 mg/day po morphine ≈ 588 mg/d po methadone – ie. throw out your opioid conversion tables in neurotoxicity Case presentation final – Nov. 20/01 marked decline – No longer able to swallow methadone… switched to hydromorphone 6 mg SQ q4h – Died comfortably Nov. 24/01 Spectrum of Opioid-Induced Neurotoxicity Opioid tolerance Mild myoclonus (eg. with sleeping) Delirium Opioids Increased Severe myoclonus Seizures, Death Hyperalgesia Agitation Misinterpreted as Pain Opioids Increased Misinterpreted as Disease-Related Pain Mayer D. et al Proc. Natl. Acad. Sci. USA Vol. 96, pp. 7731-7736 Jul. 1999 A Spinal Cord Model of InjuryInduced Hyperalgesia Mao, J. et al Pain 62 (1995) 259-274 A Spinal Cord Model of Morphine Tolerance Mao, J. et al Pain 62 (1995) 259-274 Harrison, C. et al Br. J. Anaesth. 1998; 81: 20-28 Harrison, C. et al Br. J. Anaesth. 1998; 81: 20-28 Harrison, C. et al Br. J. Anaesth. 1998; 81: 20-28 Agonist (fentanyl) Receptor (μ-opioid) G-protein 2nd messenger Response (analgesia) The process of signal transduction, with specific examples shown in parentheses Harrison, C. et al Br. J. Anaesth. 1998; 81: 20-28 Approach To The Patient With Opioid Neurotoxicity OVERVIEW OF BASIC STEPS 1. Recognize the syndrome 2. Discontinue the offending opioid Note: naloxone does not reverse neuroexcitatory effects, and may in fact exacerbate them 3. Hydrate to help clear opioid and metabolites 4. Consider benzodiazepines to decrease neuromuscular irritability 5. Explore options to address the suffering Recognizing The Syndrome Of O.I.N. • Delirium, agitation, restlessness • Myoclonus, potentially seizures • Allodynia, Hyperalgesia - pain presentation changes to “pain all over”; doesn’t make sense in terms of underlying disease • Rapidly increasing opioid dose; seems to make things worse Discontinue the Offending Opioid • Simply decreasing the dose only postpones the need to switch opioids • Adding a benzodiazepine without addressing the opioid ignores potential reversibility • Stepwise conversion (days) in mild neurotoxicity • Abrupt discontinuation if life-threatening neurotoxicity (seizures imminent) Hydrate to Help Clear Opioid and Metabolites • Morphine and hydromorphone metabolites are renally excreted • Oral, SQ, or IV… depends on the severity and venous access • Example of aggressive hydration: NS 500 ml bolus followed by 250 ml/hr plus furosemide 40 mg IV q6h Consider Benzodiazepines to Decrease Neuromuscular Irritability • Clonazepam: long-acting; p.o. • Lorazepam: intermediate duration of action; p.o., SL, IV, (IM – for seizures) • Midazolam: short-acting; SQ, IV, SL, (IM – generally not used this route) • Be cautious with additive respiratory depressant effects if also giving opioids by bolus Explore Options to Address the Suffering • This can include: – Switching opioids – Steps to ↓ opioid requirements o adjuvants (eg/gabapentin, corticosteroids, ketamine, bisphosphonates) o Procedural intervention- epidural, spinal, intrathecal catheters o Radiation,chemotherapy o Orthopedic intervention o Seating, positioning Explore Options to Address the Suffering ctd May be other issues to address that have been treated with opioids as physical pain PHYSICAL PSYCHOSOCIAL SUFFERING SPIRITUAL EMOTIONAL CHALLENGES IN MANAGING PAIN / DISTRESS IN SETTINGS OF NEUROTOXICITY • Quite possible that a substantial proportion of the current offending opioid dose is being targeted at treating opioid-induced hyperalgesia or restlessness the opioid has been increased to treat its own side effects • + + tolerance to the offending opioid, not “crossed-over” to alternatives (incomplete cross-tolerance) • Impossible to calculate dose equivalences of alternative opioids; conversion charts dangerous to use ADVANTAGES OF FENTANYL OR SUFENTANIL IN NEUROTOXICITY • No known active metabolites • Different opioid class (anilinopiperidines) than morphine and hydromorphone (benzomorphans) • Not common (though not impossible) to develop signs of neurotoxicity • Sufentanil – patients will not be on this as an outpatient… will not be presenting with related neurotoxicity tolerance will not have developed • Rapid onset, short-acting – facilitates titration in difficult, unstable circumstances METHADONE • Racemic mixture of 2 stereoisomers • only the R-enantiomer has analgesic properties • S-enantiomer: NMDA receptor antagonist ? Role in mitigating effects of M3G Approach to Changing Opioids in Settings of O.I.N. ? Life-Threatening (severe myoclonus,seizures) No • • 1. 2. 3. Can titrate off of offending opioid over days As you titrate down, add appropriate doses of an alternative opioid: Pain Poorly Controlled: ↑ dose of new opioid Pain well controlled, patient alert: ↑ new opioid, ↓offending opioid Pain well controlled, patient lethargic: ↓offending opioid Yes • Abrupt withdrawal of offending opioid • Aggressive hydration • prn dosing of either fentanyl, sufentanil, or methadone • Don’t try to calculate an appropriate starting dose based on current opioid use…. Start low and titrate up • After a few hours, consider starting a regular administration (infusion, perhaps oral methadone) Equivalency Ratios in Converting to Methadone: Interpret With Caution Morphine Total Daily mg po Morphine:Methadone Ratio 30 – 90 3.7 90 - 300 7.75 > 300 12.25 Ripamonti et al; J Clin Oncol 1998 Hydromorphone Total Daily mg po Hydromorphone:Methadone Ratio 3-6 0.30 6 - 24 0.89 24 - 100 0.74 100 - 300 1.5 >300 1.5 Ripamonti et al; Annals Oncol 1998 The Latest Innovation in Opioid Conversion Calculation