Knee disorders – Part 1
advertisement

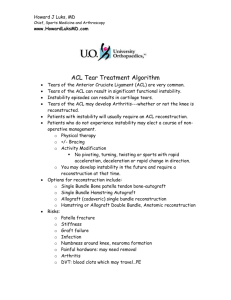
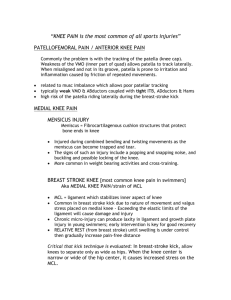
Salsabeel Matalqah Medical ppt http://hastaneciyiz.blogspot.com Menisci Tears *Common among young active adults. *Common in Football players: flexion of knee joint in addition to twisting. *Little force is needed in middle aged, because fibrosis restricts mobility of meniscus. *After age 50, tears are more commonly due to arthritis than trauma. *Medial Menisci: more prone to injury because of its restricted anatomy due to attachment to the joint capsule and to the tibial collateral ligament make it less mobile. Meniscus Tears Classification according to Mechanism ( traumatic Vs degenerative) Pattern of tear ( bucket handle Vs horizontal…. ). Menisci Tears Patterns of tears: *Bucket-Handle Tears: The split is vertical, along the circumference of the meniscus leaving anterior and posterior segments attached loosely. Sometimes the torn part displaces towards the center, causing “locking” (extension block). Menisci Tears Horizontal tears: *Usually degenerative in origin or due to repetitive minor trauma, or with association with meniscal cysts. *Generally speaking, most of the meniscus is avascular, except the outer third-from capsule-, due to this spontaneous repair doesn’t occur. *The loose part act as a mechanical irritant causing recurrent synovial effusion, and in severe cases secondary osteoarthritis. Menisci Tears Clinical Features: • Patients may complain of pain at the joint line area, locking, clicking, giving way, and swelling with activity. • In ptn >40yrs the main complaint is recurrent giving way or locking. Physical exam: •Joint line tenderness (Mostly medial). •Joint held slightly flexed. •Joint effusion may be present. •In late cases quadriceps are wasted. •Flexion is full , extension limited. _ Joint line tenderness: the most imp and specific test _ Apley’s grind test: • Isolates meniscii • Prone with knee flexed,axial load and rotation. - McMurray’s test • Flex/ext with varus/valgus and int/ext rotation. • Goal is to get torn piece to pop in and out of place. • Positive if pop or reproduction of pain. Menisci Tears Imaging X-ray – Normal MRI – most useful may reveal tears missed by arthroscopy Arthroscopy : Diagnostic and therapeutic. You have to be certain that the lesion you can see is the one causing the patient’s symptoms. Treatment Most meniscal tears do not heal without intervention. If conservative treatment does not allow the patient to resume desired activities, occupation, or sport, surgical treatment is considered. Surgical treatment of symptomatic meniscal tears is recommended because untreated tears may increase in size and may abrade articular cartilage, resulting in arthritis. Menisci Tears Treatment Conservative treatment of meniscal injuries begins with RICE (Rest, Ice, Compression, and Elevation). Arthroscopy is the preferred method. peripheral tears – surgery. The displaced portion should be excised. Postoperative physiotherapy. Recurrent patellar dislocation Anatomy of patella Soft tissue elements affecting the patella are the stabilizing capsular and ligamentous structures within which the patella lies. Some ligaments of the knee are continuous with the fibrous capsule surrounding the patella. When injuries occur, all structures are simultaneously affected. These ligaments hold the patella in place during static and dynamic phases. Recurrent patellar dislocation The knee is normally in slight valgus so there is a natural tendency for the patella to pulled to the lateral side when the quadriceps muscle is contracted Traumatic dislocation is due to sudden sever contraction of the quadriceps muscle while the knee is stretched in valgus and external rotation. The patella dislocates laterally and the medial retinacular fibers may be torn 15-20. % of patient with patellar dislocation will have recurrent episodes. It may develop without initial trauma Recurrent patellar dislocation The predisposing factors are : 1- generalized ligamentous laxity . 2- under development of lateral femoral condyle and flattening of the intercondyler groove. 3- maldevelopment of the patella;too high or to small . 4- valgus deformity of the knee. 5- primary muscle defect. Clinical features Females > males . Often bilateral c/o: -acute pain :tearing sensation - knee is stuck in flexion and the patient may fall. Often the patella is repositioned spontaneouslly - if the patella remain unreduced Medial mass because the uncovered medial femoral condoyle stand out prominently- NOT THE PATELLA-. no active or passive movement is possible On exam : - Tenderness on the medial side of the joint. - Swelling . - Aspiration may reveled a blood stained effusion . - positive Apprehension test. Clinical features CONT. Apprehension sign. The knee is placed at 30° flexion, and lateral pressure is applied. Medial instability results in apprehension .by the patient Imaging : X-ray (includes anteroposterior, true lateral, and axial or sunrise views ( CT scan MRI lateral patellar dislocation (arrows) Sunrise (skyline) view Recurrent patellar dislocation Complications : -Repeated dislocation damage the contiguous surface of patella and femoral condyle which lead to further dislocation -later Secondary OA. Rx: If still dislocated : PUSH IT BACK ( gently) + cylinder plaster or splint is applied for 2-3 weeks + quadriceps strengthening exercise for 3 months. In children : The patellar mechanism tends to stabilize as the child grows but 15% of these children will suffer from repeated attacks which will be an indication for surgery . Role of surgery in recurrent patellar dislocation : 1- to repair or strengthen the medial patellofemoral ligament . 2- to realign the extensor mechanism. Ligament injury Anterior Cruciate Ligament: The Anterior Cruciate Ligament (ACL) is the main support structure of the knee that prevents rotation of the Femur on the Tibia .The ACL also prevents the Tibia from translating forward on the Femur. This ligament is injured in sports more. The knee is a hinge joint, comprised of three bones and four main ligaments. The joint has one plane of motion, flexion and extension. Due to this construction, a slight amount of rotation does occur, but the ligaments limit this motion. The three bones are the Femur, Tibia and Patella .The four ligaments in the knee are the ACL, Posterior Cruciate (PCL), Medial Collateral (MCL), and Lateral Collateral (LCL). These ligaments connect the Tibia and Femur and provide the structural integrity to the knee. The ACL and PCL were named for their location. The two ligaments are located in the middle of the knee and cross one another (cruciate is Latin for cross). The ACL has its origin on the front, or anterior, aspect of the Tibia, while the PCL originates on the back, or posterior, aspect of the Tibia. The MCL is located on the inside, or medial, aspect of the knee and the LCL is located on the outside, or lateral, aspect of the knee. Which ligament is affected? History History of hyper-extension and twisting injury, claim to have heard a “pop” as the tissue snapped (at the time of injury). Immediate swelling Knee is painful Tenderness is most acute over the torn ligament. Stressing one or other side of the joint may produce excruciating pain P/E Physical exam shows a positive anterior drawer sign at 30 degrees (Lachman test) and at 90 degrees. drawer test Lachman test the pivot shift test is also positive. Investigation Stress x-rays may provide evidence of instability Plain x-rays may show that the ligament has avulsed a small piece of bone:-The MCL usually from the femur -LCL from the fibula -ACL from the tibial spine -PCL from the back of the upper tibia treatment • Conservative management is indicated in patients who can accept modification of activities that produce instability; instability is thought to put the menisci at risk of damage • Surgical repair is not successful; reconstruction is an individual decision based on the patient’s desires and requirements • Patients engaging in competitive athletics generally require reconstruction; the methods vary but generally use autograft to replace the ACL Sprains and partial tears Intact fibers splint the torn ones and so spontaneous healing will occur Adhesions may result, so active exercise is prescribed Aspirating the haemarthrosis and applying ice packs intermittently relieves pain Weight-bearing is allowed Knee is protected from rotation or angulation strains by a heavily padded bandage or a functional brace Complete tears Isolated MCL or LCL treated as above Isolated tears of ACL may be treated by early operative reconstruction if the individual is a professional sportsman Cast-brace is worn until symptoms subside, thereafter movement and muscle-strengthening exercise. This is sufficient in about half of the patients as they regain good function and need no further treatment. Remainder will have varying instability, late assessment will identify those who will benefit from ligament reconstruction. Isolated tears of the PCL are usually treated conservatively Combined injuries In ACL and collateral ligament injury treatment starts with joint bracing and physiotherapy to restore a good range of movements before ACL reconstruction Combined injuries involving the PCL the same approach is used however all damaged structures need to be repaired Complications Adhesions If the knee with a partial ligament tear is not actively exercised, torn fibers will stick to intact fibers and bone. The knee gives way with catches of pain, localized tenderness and pain on lateral or medial rotation occur Confusion with a torn meniscus can be resolved by the grinding test or arthroscopy Instability The knee continues to give way and tends to get worse predisposing to osteoarthritis. Reconstruction before degeneration is wise. Medical ppt http://hastaneciyiz.blogspot.com