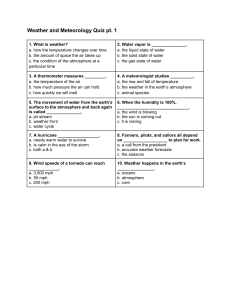
Study Guide Health System
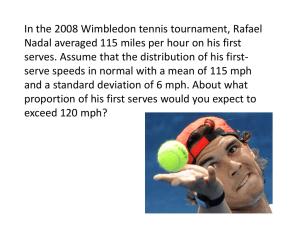
advertisement

Study Guide Health System-Based Practice List of Content Curriculum of Health System Based Practice 3 Planners Team 9 Facilitators 9 Reserve Facilitators 10 Time Table 11 Time Table for Discussion of Student Project 23 Assessment Method 23 Module 1 – 18 24 Curriculum Mapping 60 Udayana University, Faculty of Medicine, DME 1 Study Guide Health System-Based Practice List of Modules Day 1: MODULE ~ 1 p.24 Introduction to Health System and Primary Health Care: The Basic Principles Day 2 -3: MODULE ~ 2 Health Indicators and Health Services Related Problems p.29 Day 2-3: MODULE ~ 3 Health Care System in Several Countries p.31 Day 4-5: MODULE ~ 4 National Health Care System of Indonesia 2012 p.33 Day 4-5: MODULE ~ 5 Puskesmas as a Primary Health Care Service p. 35 Day 6-7: MODULE ~ 6 Primary Health Care and Health Promotion p.37 Day 6-7: MODULE ~ 7 Basic Theories underlying Health Promotion p.39 Day 8-9: MODULE ~ 8 Health Management in Health Services p.41 Day 8-9: MODULE ~ 9 Health Workforce and Human Resource Management p.43 Day 10-11: MODULE ~ 10-11 Quality Management 1 & 2 p.45 Day 12-13: MODULE ~ 12 Management of Facilities, Information, and Finance p. 49 Day 12-13: MODULE ~ 13 Managed Care p. 53 Day 14-15: MODULE ~ 14 Health Insurance and SJSN p. 55 Day 14-15: MODULE ~ 15 Family Medicine Practices: Family as a Unit of Care p.57 Day 16-17: MODULE ~ 16 Health Delivery System and Family Medicine Practices p.59 Day 16-17: MODULE ~ 17 Disease Management Skills p. 63 Day 18-19: MODULE ~ 18 Basic Clinical Skill: Discussion of Student Project p. 65 Udayana University, Faculty of Medicine, DME 2 Study Guide Health System-Based Practice CURRICULUM Health System Based Practice Competency Statements Manage health services in primary health system Instructional Goals Learning Objectives Topics 1. Demonstrate ability to provide health services in accordance with a country’s health system 1. Describe health problems using health indicators. 2. Describe definition and areas of health care system 3. Explain the relationship among people, health provider and finance state in health delivery system. 4. Explain the importance of implementation of health care system as a solution of health problem Health Indicators and Health Services Related Problems 5. Introduction to Health System and Primary Health Care: The Basic 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. Udayana University, Faculty of Medicine, DME Explain the role of a country in desGNing a health care system. Describe the role of health care system toward health status of the people. Describe stakeholders’ roles in health care system. Describe the challenges that might be faced in delivering health services. Explain the dilemmas in delivering health services. Describe the roles of family medicine in health care system. Describe the steps of family medicine development. Explain the objectives of health services. Explain the functions of health services. Describe the values that should be included in a health care system. Describe the problems of a country in developing health care system. Principles 3 Study Guide Health System-Based Practice Competency Statement Instructional Goals Learning Objectives Topics 16. Explain the challanges that are faced by every country in developing a health care system. 17. Describe the roles of primary health services in solving the health care system’s problems. Udayana University, Faculty of Medicine, DME 18. Explain the objectives of SKN. 19. Describe the subsystems in SKN including: a. Health services. b. Health financing. c. Human resources. d. Drug & health facilities. e. Community empowerment. f. Health management 20. Describe relationship among sub systems. 21. Describe the application of SKN. National Health System (Sistem Kesehatan Nasional (SKN)) 2012 22. Describe various types of Health Care System which have been or being adopted by a certain country. 23. Explain advantages and disadvantages of each system. 24. Describe the role of government and private sector in each system. 25. Describe various professions in Health Care System. 26. Explain the effect of Health Care financing to the health status of people. 27. Describe basic principles of WHO recommendation to the National Health Care System Health Care System in Several Countries 4 Study Guide Health System-Based Practice Competency Statement Instructional Goals 2. Demonstrate ability to apply the concept of management to provide health services at primary level Learning Objectives Topics 28. Describe major factors affecting health status. 29. Define Health Education and Health Promotion 30. Explain the aspects of health promotion based on the Ottawa Charter. 31. Explain the strategic role of Health Education and Health Promotion in achieving optimum health status of every individual. 32. Comprehend Health Promotion glossary. Primary Health Care and Health Promotion 33. Explain basic theories underlying Health Education and Health Promotion. 34. Describe basic principles of diffusion of innovations and the decision making process. 35. Summarized major theories of behavior change. Basic theories underlying health promotion 1. Describe the structure of primary health services in puskesmas. 2. Explain the basic programs and the additional programs in puskesmas. 3. Describe the financing system of basic programs in puskesmas. 4. Explain the application of private health services management based on the finance resources: Puskesmas as a Primary Health Care Service a. Askes b. Askeskin/JPKMM c. General patients 5. Describe the application of private and public health services management in puskesmas. Udayana University, Faculty of Medicine, DME 5 Study Guide Health System-Based Practice Competency Statement Instructional Goals Learning Objectives 6. 7. 8. 9. Describe the principles of management in health care services. Comprehend the concepts of managing people in health services Explain the concepts of supplies and stores management (SSM). Describe how to control discrepancies in a clinic. Topics Health Management Concepts in Health Services (Management of people, facilities, information, finance, and quality) 10. Comprehend the concepts of managing information and finance. 11. Describe basic concept of quality in health-care 12. Describe how to manage healthcare in whole system for quality improvement 13. Explain the concept of managed care. 14. Describe the types of managed care. Managed Care 15. Explain the basic concept of Health health insurance. Insurance and 16. Describe several models of SJSN health insurance. 17. Explain the financing system of health insurance. 18. Explain the application of health insurance through SJSN. 19. Describe the application of a managed care in health insurance. 3. Apply family medicine approach in primary health services Udayana University, Faculty of Medicine, DME 1. Describe the definition of a family. 2. Describe the functions of family. 3. Explain the cycle of family development including the main objective in each step. 4. Describe the influence of family toward the health status of its members. Family Medicine Practices: Family as a Unit of Care 6 Study Guide Health System-Based Practice Competency Statement Instructional Goals Learning Objectives Topics 5. Differentiate the characteristics of a happy and an unhappy family. 6. Describe the roles of family doctor in assisting an unhappy family 7. Explain the level of a doctor’s involvement in a family with health problems. 8. Describe the family dynamics that affecting health status of family member. 9. Draw and describe a family genogram. 10. Describe the definition of family medicine as a discipline. 11. Describe place and position of family medicine in the health care system. 12. Explain the knowledge and skill that are required in family medicine practice. 13. Compare integrated health activities within and between providers. 14. Describe the application of the principles of family doctor services covering: a. personal care b. primary care c. comprehensive care d. continuing care 15. Explain the coordinative and collaborative aspects using basic approaches of family medicine. 16. Describe the basic approaches of family medicine at the individual, family and community levels. Udayana University, Faculty of Medicine, DME Health delivery system and family medicine 7 Study Guide Health System-Based Practice Competency Statement Instructional Goals Learning Objectives 17. Describe the differences between acute and chronic diseases management. 18. Explain how to help patients to evaluate their conditions. 19. Describe how to educate patients with chronic diseases in order to empower them in diseases management. 20. Describe how to make similar perception of diseases with patients and how to determine the objectives to be achieved together. 21. Explain how to desGN and to apply the clinical management of chronic diseases. Udayana University, Faculty of Medicine, DME Topics Diseases management skill 8 Study Guide Health System-Based Practice ~ PLANNERS TEAM ~ No Name Department Phone 1 DR. Luh Seri Ani, SKM., M.Kes (Coordinator) Community/Preventive 08123924326 2 dr. Komang Ayu Kartika Sari, MPH (Secretary) Community/Preventive 082147092348 3 dr. I Nyoman Sutarsa, MPH Community/Preventive 087860380028 4 DR. dr. I Wayan Weta, MS, SpGK Community/Preventive 081337005360 5 dr. I.B. Wirakusuma, MOH DR. dr. GN Indraguna Pinatih, MSc, SpGk,Akp dr. Ni Luh Putu Ariastuti, MPH Community/Preventive 08124696647 Community/Preventive 08123816424 Community/Preventive 0818560008 6 7 ~ FACILITATORS ~ Regular Class (Class A) No 1 Name dr. Putu Anda Tusta Adiputra , Sp.B(K)Onk Department Surgery Phone Group Room Number A-1 A.3.09 08123826430 2 dr. Komang Ayu Kartika Sari, MPH Public Health 082147092348 A-2 A.3.10 3 Ni Wayan Tianing, S.Si, M.Kes Biochemistry 08123982504 A-3 A.3.11 4 dr. Ni Putu Ekawati, M.Repro, Sp.PA A-4 A.3.12 Anatomy Pathology 08113803933 Pharmacy 0811399886 A-5 A.3.13 Interna 08123803985 A-6 A.3.14 ENT 08113809882 A-7 A.3.15 Pharmacology 08123687288 A-8 A.3.16 A-9 A.3.17 A-10 A.3.19 5 Drs. I Nyoman Toya Wiartha, Apt 6 dr. A.A.A. Yuli Gayatri, Sp.PD 7 dr. Made Lely Rahayu, Sp.THT 8 dr. Ida Bagus Ngurah , M For 9 dr. Wira Gotera, Sp.PD-KEMDFINASIM 10 dr. I Wayan Sugiritama, M. Kes Udayana University, Faculty of Medicine, DME Interna Histology 08155736480 08123925104 9 Study Guide Health System-Based Practice English Class (Class B) No Name Department Phone Group Room Number Parasitology 08123662311 B-1 A.3.09 Anatomy 085103043575 B-2 A.3.10 Public Health 0818560008 B-3 A.3.11 Interna 08123853700 B-4 A.3.12 B-5 A.3.13 B-6 A.3.14 B-7 A.3.15 B-8 A.3.16 1 dr. Ni Luh Ariwati 2 dr. Muliani , M Biomed 3 dr. Ni Luh Putu Ariastuti, MPH 4 dr. I Ketut Mariadi, Sp.PD 5 Desak Gde Diah Dharma Santhi, S.Si, Apt, M.Kes Clinical Pathology 0817569021 dr. I Gusti Ngurah Wien Aryana , Sp.OT Orthopaedi 0811385263 dr. I Gusti Ngurah Pramesemara , S.Ked Andrology 081338605087 dr. I Gusti Lanang Ngurah Agung Artha Wiguna, Sp.OT (K) Orthopaedi 0811388859 Interna 08123989192 B-9 A.3.17 Orthopaedi 081338493832 B-10 A.3.19 6 7 8 9 dr. Putu Andrika, Sp.PD-KIC 10 dr. I Gede Eka Wiratnaya, , Sp.OT Reserve Facilitators No Name Department Phone 1 DR. dr. GN Indraguna Pinatih, MSc, SpGk, Akp 2 dr. A.A.Sg. Sawitri, MPH Com/Prev 08123816424 Com/Prev 0817340145 3 DR. dr. I Wayan Weta, MS, SpGK Com/Prev 081337005360 4 DR. Luh Seri Ani, SKM., M.Kes Com/Prev 08123924326 Udayana University, Faculty of Medicine, DME 10 Study Guide Health System-Based Practice ~ TIME TABLE ~ Regular Class (A) Days/date Time Activity Venue Lecturers dr. I Nyoman Sutarsa, MPH Introductory Lecture 08.00 – 09.00 Introduction to Health System and Primary Health Care: The Basic Principles Theatre Room (4th floor) 1 09.00 – 11.00 Movie Presentation (“John Q” ) Theatre Room (4th floor) Tuesday 14th of April 11.00 – 12.30 SGD (Task-1) 12.30 – 13.00 Independent Learning 13.00 – 14.00 Student presentation (SP) and feedback Discussion Room (DR) Class Room (CR) 3.01 Introductory lecture 09.00 – 10.00 Health Indicators and Health Services Related Problems CR 3.01 dr. I Nyoman Sutarsa, MPH DR. Luh Seri Ani, SKM., M.Kes Introductory Lecture 10.00 – 11.00 Health Care System in Several Countries 11.00 – 12.00 Break/Lunch 12.00 – 15.00 SGD (Task-2): Health Indicators and Health Services Related Problems 2 Wednesday 15th of April CR 3.01 dr. I Nyoman Sutarsa, MPH DR SGD (Task-3): Health Care System in Several Countries Student presentation and feedback: 09.00 – 10.00 3 Thursday 16th of April Health Indicators and Health Services Related Problems CR 3.01 DR. Luh Seri Ani, SKM., M.Kes CR 3.01 dr. I Nyoman Sutarsa, MPH Student presentation and feedback: 10.00 – 11.00 Health Care System in Several Countries 11.00 – 12.00 Break/Lunch 12.00 – 15.00 Independent Learning Udayana University, Faculty of Medicine, DME 11 Study Guide Health System-Based Practice Days/ date Activity Time Venue Introductory Lecture 09.00 – 10.00 National Health Care System of Indonesia 2012 CR 3.01 dr. I.B Wirakusuma, MOH / DR. dr. I Wayan Weta, MS, SpGK CR 3.01 dr. I.B Wirakusuma, MOH / DR. dr. I Wayan Weta, MS, SpGK Introductory Lecture 4 Friday 17th of April 10.00 – 11.00 Puskesmas as a Primary Health Care Service 11.00 – 12.00 Break/Lunch Lecturers SGD (Task-4): 12.00 – 15.00 National Health Care System of Indonesia 2012 DR SGD (Task – 5): Puskesmas as a Primary Health Care Service 09.00 – 10.00 5 Monday 20th of April 10.00 – 11.00 Student Presentation and Feedback: CR 3.01 dr. I.B Wirakusuma, MOH / DR. dr. I Wayan Weta, MS, SpGK CR 3.01 dr. I.B Wirakusuma, MOH / DR. dr. I Wayan Weta, MS, SpGK CR 3.01 dr. Komang Ayu Kartika Sari, MPH / dr. Ni Luh Putu Ariastuti, MPH CR 3.01 dr. Komang Ayu Kartika Sari, MPH / dr. Ni Luh Putu Ariastuti, MPH National Health Care System of Indonesia 2012 Student Presentation and Feedback: Puskesmas as a Primary Health Care Service 11.00 – 12.00 Break/Lunch SGD 12.00 – 15.00 Independent Learning Introductory Lecture 09.00 – 10.00 Primary Health Care and Health Promotion Introductory Lecture 6 10.00 – 11.00 Basic Theories underlying Health Promotion 11.00 – 12.00 Break/Lunch Tuesday 21st of April SGD (Task-6): 12.00 – 15.00 Primary Health Care and Health Promotion DR SGD (Task-7): Basic Theories underlying Health Promotion Udayana University, Faculty of Medicine, DME 12 Study Guide Health System-Based Practice Days/ date 09.00 – 10.00 7 Wednesday 22nd of April Activity Time 10.00 – 11.00 Student Presentation and Feedback: Student Presentation and Feedback: Break/Lunch 12.00 – 15.00 Independent Learning CR 3.01 dr. Komang Ayu Kartika Sari, MPH / dr. Ni Luh Putu Ariastuti, MPH CR 3.01 Health Management in Health Services Introductory Lecture 23rd of April CR 3.01 dr. Komang Ayu Kartika Sari, MPH / dr. Ni Luh Putu Ariastuti, MPH Basic Theories underlying Health Promotion Introductory Lecture 8 Thursday Lecturers Primary Health Care and Health Promotion 11.00 – 12.00 09.00 – 10.00 Venue 10.00 – 11.00 Health Workforce and Human Resource Management 11.00 – 12.00 Break/Lunch CR 3.01 dr. Komang Ayu Kartika Sari, MPH / DR. dr. GN Indraguna Pinatih, MSc, SpGK, Akp dr. Komang Ayu Kartika Sari, MPH / DR. dr. GN Indraguna Pinatih, MSc, SpGK, Akp SGD (Task-8): 12.00 – 15.00 Health Management in Health Services DR SGD (Task-9): Health Workforce and Human Resource Management 09.00 – 10.00 9 Friday 24th of April 10.00 – 11.00 Student Presentation and Feedback: CR 3.01 Health Management in Health Services Student Presentation and Feedback: Health Workforce and Human Resource Management 11.00 – 12.00 Break/Lunch 12.00 – 15.00 Independent Learning Udayana University, Faculty of Medicine, DME CR 3.01 dr. Komang Ayu Kartika Sari, MPH / DR. dr. GN Indraguna Pinatih, MSc, SpGK, Akp dr. Komang Ayu Kartika Sari, MPH / DR. dr. GN Indraguna Pinatih, MSc, SpGK, Akp 13 Study Guide Health System-Based Practice Days/ date 10 Monday 27th of April Activity Time 09.00 – 10.00 Introductory Lecture Quality Management (1) 10.00 – 11.00 Introductory Lecture Quality Management (2) 11.00 – 12.00 Break/Lunch Venue Lecturers CR 3.01 dr. I Nyoman Sutarsa, MPH / dr. Ni Luh Putu Ariastuti, MPH CR 3.01 dr. I Nyoman Sutarsa, MPH / dr. Ni Luh Putu Ariastuti, MPH SGD (Task-10): 12.00 – 15.00 Quality Management (1) DR SGD (Task-11): Quality Management (2) 11 Tuesday 28th of April 09.00 – 10.00 Student Presentation and Feedback: Quality Management (1) CR 3.01 dr. I Nyoman Sutarsa, MPH / dr. Ni Luh Putu Ariastuti, MPH 10.00 – 11.00 Student Presentation and Feedback: Quality Management (2) CR 3.01 dr. I Nyoman Sutarsa, MPH / dr. Ni Luh Putu Ariastuti, MPH 11.00 – 12.00 Break/Lunch 12.00 – 15.00 Independent Learning DR. dr. GN Indraguna Pinatih, MSc, SpGK, Akp Introductory Lecture 12 Wednesda y 29th of April 09.00 – 10.00 Management of Facilities, Information, and Finance CR 3.01 10.00 – 11.00 Introductory Lecture Managed Care CR 3.01 11.00 – 12.00 Break/Lunch DR. dr. I Wayan Weta, MS, SpGK SGD (Task-12): 12.00 – 15.00 Management of Facilities, Information, and Finance DR SGD (Task-13): Managed Care 13 Thursday 30th of April 09.00 – 10.00 Student Presentation and Feedback: Management of Facilities, Information, and Finance 10.00 – 11.00 Student Presentation and Feedback: Managed Care 11.00 – 12.00 Break/Lunch 12.00 – 15.00 Independent Learning Udayana University, Faculty of Medicine, DME CR 3.01 CR 3.01 DR. dr. GN Indraguna Pinatih, MSc, SpGk, Akp DR. dr. I Wayan Weta, MS, SpGK 14 Study Guide Health System-Based Practice Days/date 14 Monday 4th of May Time Activity Venue Lecturers 09.00 – 10.00 Introductory Lecture Health Insurance and SJSN CR 3.01 dr. I Nyoman Sutarsa, MPH 10.00 – 11.00 Introductory Lecture Family Medicine Practices: Family as a Unit of Care CR 3.01 DR. dr. I Wayan Weta, MS, SpGK 11.00 – 12.00 Break/Lunch SGD (Task-14): Health Insurance and SJSN 12.00 – 15.00 15 Tuesday 5th of May 16 Thursday 7th of May SGD (Task-15): Family Medicine Practices: Family as a Unit of Care DR Student Presentation and Feedback: Health Insurance and SJSN CR 3.01 09.00 – 10.00 10.00 – 11.00 Student Presentation and Feedback: Family Medicine Practices: Family as a Unit of Care 11.00 – 12.00 Break/Lunch 12.00 – 15.00 Independent Learning 09.00 – 10.00 Introductory Lecture Health Delivery System and Family Medicine Practices 10.00 – 11.00 Introductory Lecture Disease Management Skills 11.00 – 12.00 Break/Lunch 12.00 – 15.00 SGD (Task-16): Health Delivery System and Family Medicine Practices dr. I Nyoman Sutarsa, MPH CR 3.01 DR. dr. I Wayan Weta, MS, SpGK CR 3.01 DR. dr. I Wayan Weta, MS, SpGK CR 3.01 DR. dr. GN Indraguna Pinatih, MSc, SpGk, Akp DR SGD (Task-17): Disease Management Skills 17 Friday 8th of May 09.00 – 10.00 Student Presentation and Feedback: Health Delivery System and Family Medicine Practices CR 3.01 10.00 – 11.00 Student Presentation and Feedback: Disease Management Skills CR 3.01 11.00 – 12.00 Break/Lunch 12.00 – 15.00 Independent Learning Udayana University, Faculty of Medicine, DME DR. dr. I Wayan Weta, MS, SpGK DR. dr. GN Indraguna Pinatih, MSc, SpGk, Akp 15 Study Guide Health System-Based Practice Days/date 18 Monday, 11th of May 19 Tuesday, 12th of May 20 Wednesday, 13th of May Time Activity Venue Lecturers Basic Clinical Skill CR 3.01 Team CR 3.01 Team CR 3.01 Team (Group Discussion of Student Project) Basic Clinical Skill (Group Discussion of Student Project) Presentation of Student Project Thursday, 14th of May 2015 – Pre-Examination Break Monday, 18th of May Udayana University, Faculty of Medicine, DME Final Examination Team 16 Study Guide Health System-Based Practice ~ TIME TABLE ~ English Class (B) Days/ date Time Activity Venue Lecturers dr. I Nyoman Sutarsa, MPH Introductory Lecture 08.00 – 09.00 Introduction to Health System and Primary Health Care: The Basic Principles Theatre Room (4th floor) 1 09.00 – 11.00 Movie Presentation (“John Q” ) Theatre Room (4th floor) Tuesday 14th of April 11.00 – 12.30 Independent Learning 12.30 – 14.00 SGD (Task-1) 14.00 – 15.00 Student presentation (SP) and feedback 09.00 – 12.00 Independent Learning 12.00 – 13.00 Break/Lunch 2 Wednesda y 15th of April Discussion Room (DR) Class Room (CR) 3.01 Introductory lecture 13.00 – 14.00 Health Indicators and Health Services Related Problems CR 3.01 dr. I Nyoman Sutarsa, MPH DR. Luh Seri Ani, SKM., M.Kes Introductory Lecture 14.00 – 15.00 09.00 – 12.00 Health Care System in Several Countries SGD (Task-2): Health Indicators and Health Services Related Problems CR 3.01 dr. I Nyoman Sutarsa, MPH DR SGD (Task-3): Health Care System in Several Countries 3 Thursday 16th of April 12.00 – 13.00 Break/Lunch Student presentation and feedback: 13.00 – 14.00 Health Indicators and Health Services Related Problems CR 3.01 DR. Luh Seri Ani, SKM., M.Kes CR 3.01 dr. I Nyoman Sutarsa, MPH Student presentation and feedback: 14.00 – 15.00 Health Care System in Several Countries Udayana University, Faculty of Medicine, DME 17 Study Guide Health System-Based Practice Days/ date 09.00 – 12.00 Independent Learning 12.00 – 13.00 Break/Lunch Venue Lecturers CR 3.01 dr. I.B Wirakusuma, MOH / DR. dr. I Wayan Weta, MS, SpGK CR 3.01 dr. I.B Wirakusuma, MOH / DR. dr. I Wayan Weta, MS, SpGK Introductory Lecture 4 Friday 17th of April Activity Time 13.00 – 14.00 National Health Care System of Indonesia 2012 Introductory Lecture 14.00 – 15.00 Puskesmas as a Primary Health Care Service SGD (Task-4): 09.00 – 12.00 National Health Care System of Indonesia 2012 DR SGD (Task – 5): Puskesmas as a Primary Health Care Service 5 Monday 20th of April 12.00 – 13.00 13.00 – 14.00 14.00 – 15.00 Student Presentation and Feedback: CR 3.01 National Health Care System of Indonesia 2012 Student Presentation and Feedback: Independent Learning 12.00 – 13.00 Break/Lunch CR 3.01 dr. Komang Ayu Kartika Sari, MPH / dr. Ni Luh Putu Ariastuti, MPH CR 3.01 dr. Komang Ayu Kartika Sari, MPH / dr. Ni Luh Putu Ariastuti, MPH Introductory Lecture 13.00 – 14.00 21st of April Primary Health Care and Health Promotion Introductory Lecture 14.00 – 15.00 Basic Theories underlying Health Promotion Udayana University, Faculty of Medicine, DME dr. I.B Wirakusuma, MOH / DR. dr. I Wayan Weta, MS, SpGK dr. I.B Wirakusuma, MOH / DR. dr. I Wayan Weta, MS, SpGK Puskesmas as a Primary Health Care Service 09.00 – 12.00 6 Tuesday Break/Lunch SGD 18 Study Guide Health System-Based Practice Days/ date Activity Time Venue Lecturers SGD (Task-6): 09.00 – 12.00 Primary Health Care and Health Promotion DR SGD (Task-7): Basic Theories underlying Health Promotion 7 Wednesd ay22nd of April 12.00 – 13.00 13.00 – 14.00 14.00 – 15.00 Break/Lunch Student Presentation and Feedback: Student Presentation and Feedback: Basic Theories underlying Health Promotion 09.00 – 12.00 Independent Learning 12.00 – 13.00 Break/Lunch 13.00 – 14.00 CR 3.01 dr. Komang Ayu Kartika Sari, MPH / dr. Ni Luh Putu Ariastuti, MPH Primary Health Care and Health Promotion Introductory Lecture 8 Thursday CR 3.01 dr. Komang Ayu Kartika Sari, MPH / dr. Ni Luh Putu Ariastuti, MPH CR 3.01 Health Management in Health Services 23rd of April Introductory Lecture 14.00 – 15.00 Health Workforce and Human Resource Management Udayana University, Faculty of Medicine, DME CR 3.01 dr. Komang Ayu Kartika Sari, MPH / DR. dr. GN Indraguna Pinatih, MSc, SpGK, Akp dr. Komang Ayu Kartika Sari, MPH / DR. dr. GN Indraguna Pinatih, MSc, SpGK, Akp 19 Study Guide Health System-Based Practice Days /date Activity Time Venue Lecturers SGD (Task-8): 09.00 – 12.00 Health Management in Health Services DR SGD (Task-9): Health Workforce and Human Resource Management 9 Friday 24th of April 12.00 – 13.00 13.00 – 14.00 14.00 – 15.00 10 Monday 27th of April Break/Lunch Student Presentation and Feedback: CR 3.01 Health Management in Health Services Student Presentation and Feedback: CR 3.01 Health Workforce and Human Resource Management 09.00 – 12.00 Independent Learning 12.00 – 13.00 Break/Lunch 13.00 – 14.00 Introductory Lecture Quality Management (1) 14.00 – 15.00 Introductory Lecture Quality Management (2) dr. Komang Ayu Kartika Sari, MPH / DR. dr. GN Indraguna Pinatih, MSc, SpGK, Akp dr. Komang Ayu Kartika Sari, MPH / DR. dr. GN Indraguna Pinatih, MSc, SpGK, Akp CR 3.01 dr. I Nyoman Sutarsa, MPH / dr. Ni Luh Putu Ariastuti, MPH CR 3.01 dr. I Nyoman Sutarsa, MPH / dr. Ni Luh Putu Ariastuti, MPH SGD (Task-10): 09.00 – 12.00 Quality Management (1) SGD (Task-11): DR Quality Management (2) 11 Tuesda y 28th of April 12.00 – 13.00 Break/Lunch 13.00 – 14.00 Student Presentation and Feedback: Quality Management (1) CR 3.01 dr. I Nyoman Sutarsa, MPH / dr. Ni Luh Putu Ariastuti, MPH 14.00 – 15.00 Student Presentation and Feedback: Quality Management (2) CR 3.01 dr. I Nyoman Sutarsa, MPH / dr. Ni Luh Putu Ariastuti, MPH Udayana University, Faculty of Medicine, DME 20 Study Guide Health System-Based Practice Days/ date 12 Wednes day 29th of April Time Activity 09.00 – 12.00 Independent Learning 12.00 – 13.00 Break/Lunch Venue Lecturers CR 3.01 DR. dr. GN Indraguna Pinatih, MSc, SpGK, Akp Introductory Lecture 13.00 – 14.00 14.00 – 15.00 Management of Facilities, Information, and Finance Introductory Lecture Managed Care CR 3.01 DR. dr. I Wayan Weta, MS, SpGK SGD (Task-12): 09.00 – 12.00 13 Thursda y 30th of April 14 Monday 4th of May Management of Facilities, Information, and Finance DR SGD (Task-13): Managed Care 12.00 – 13.00 Break/Lunch 13.00 – 14.00 Student Presentation and Feedback: Management of Facilities, Information, and Finance 14.00 – 15.00 Student Presentation and Feedback: Managed Care 09.00 – 12.00 Independent Learning 12.00 – 13.00 Break/Lunch 13.00 – 14.00 Introductory Lecture Health Insurance and SJSN 14.00 – 15.00 Introductory Lecture Family Medicine Practices: Family as a Unit of Care CR 3.01 DR. dr. GN Indraguna Pinatih, MSc, SpGk, Akp CR 3.01 DR. dr. I Wayan Weta, MS, SpGK CR 3.01 dr. I Nyoman Sutarsa, MPH CR 3.01 DR. dr. I Wayan Weta, MS, SpGK SGD (Task-14): Health Insurance and SJSN 15 Tuesday 5th of May 09.00 – 12.00 SGD (Task-15): Family Medicine Practices: Family as a Unit of Care 12.00 – 13.00 Break/Lunch 13.00 – 14.00 Student Presentation and Feedback: Health Insurance and SJSN DR CR 3.01 CR 3.01 14.00 – 15.00 dr. I Nyoman Sutarsa, MPH DR. dr. I Wayan Weta, MS, SpGK Student Presentation and Feedback: Family Medicine Practices: Family as a Unit of Care Udayana University, Faculty of Medicine, DME 21 Study Guide Health System-Based Practice 16 Thursday 7th of May Days/date 09.00 – 12.00 Independent Learning 12.00 – 13.00 Break/Lunch 13.00 – 14.00 Introductory Lecture Health Delivery System and Family Medicine Practices 14.00 – 15.00 Introductory Lecture Disease Management Skills Time 09.00 – 12.00 17 Friday 8th of May 18 Monday, 11th of May 19 Tuesday, 12th of May 20 Wednesda y, 13th of May Activity SGD (Task-16): Health Delivery System and Family Medicine Practices CR 3.01 DR. dr. I Wayan Weta, MS, SpGK CR 3.01 DR. dr. GN Indraguna Pinatih, MSc, SpGk, Akp Venue Lecturers DR SGD (Task-17): Disease Management Skills 12.00 – 13.00 Break/Lunch 13.00 – 14.00 Student Presentation and Feedback: Health Delivery System and Family Medicine Practices 14.00 – 15.00 Student Presentation and Feedback: Disease Management Skills Basic Clinical Skill CR 3.01 DR. dr. I Wayan Weta, MS, SpGK CR 3.01 DR. dr. GN Indraguna Pinatih, MSc, SpGk, Akp CR 3.01 Team CR 3.01 Team CR 3.01 Team (Group Discussion of Student Project) Basic Clinical Skill (Group Discussion of Student Project) Presentation of Student Project Thursday, 14th of May 2015 – Pre-Examination Break Monday, 18th of May Udayana University, Faculty of Medicine, DME Final Examination Team 22 Study Guide Health System-Based Practice TIME TABLE FOR DISCUSSION OF STUDENT PROJECT (Regular and English Class) Date: No 1. Monday 11th May 2015 2. Tuesday 12th May 2015 Class Group SGD Activity Time/Place 1 Regular I, II, III, IV, V Group Discussion 08.00 – 09.30 / Class room 2 Regular VI, VII, VIII, IX, X Group Discussion 09.30 – 11.00 / Class room 11.00 – 12.00 WITA Break/Lunch 3 English I, II, III, IV, V Group Discussion 12.00 – 13.30 / Class room 4 English VI, VII, VIII, IX, X Group Discussion 13.30 – 15.00 / Class room Guidance: 1. Each group is required to bring at least one laptop. 2. Each group will be provided with data/report of a community health center and will discuss the data based on a guideline. The data/report and the discussion guideline will be provided before the first discussion session. ASSESSMENT METHOD Student assessment of this block consists of: 1. a paper test with multiple choice questions at the end of the block with a proportion of 80% of the total score 2. a student project with a proportion of 15% of the total score 3. evaluation of activity during the small group discussion with a proportion of 5% of the total score Udayana University, Faculty of Medicine, DME 23 Study Guide Health System-Based Practice 2015 Day 1 MODULE ~ 1 MODULE~1 Introduction to Health System and Primary Health Care: The Basic Principles dr. I Nyoman Sutarsa, MPH AIMS: Demonstrate ability to provide health services in accordance with a country’s health system LEARNING OUTCOMES: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. Explain the role of a country in designing a health care system. Describe the role of health care system toward health status of the people. Describe stakeholders’ roles in health care system. Describe the challenges that might be faced in delivering health services. Explain the dilemmas in delivering health services. Describe the roles of family medicine in health care system. Describe the steps of family medicine development. Explain the objectives of health services. Explain the functions of health services. Describe the values that should be included in a health care system. Describe the problems of a country in developing health care system. Explain the challanges that are faced by every country in developing a health care system. 13. Describe the roles of primary health care in solving the health care system’s problems. CURRICULUM CONTENTS: Introduction to Health System and Primary Health Care: The Basic Principles ABSTRACTS (References: “John Q” movie; Boelen C, et al, pp.1-36) Meeting People’s Health Needs This topic covers the philosophy of Health Care System in which each country has a fundamental interest and responsibility for maintaining and improving the health status of its people. To reach this responsibility, each country should always consider its social and economic well being in order to be able to set up an appropriate organization, staffing and Udayana University Faculty of Medicine, DME Page 24 Study Guide Health System-Based Practice 2015 financing health care system. The organization should be initiated by government authorities and fully supported by health professionals, academic institutions and civil society. The Health Care System is intended to provide a high quality of health care services. However, the system should always agree with the basic principles of health care which include quality, equity, relevance and cost-effective to meet an optimal health status of its people. In this regards, Family Medicine seems to be the best choice for delivering health care services at the front line. Family Medicine is believed be able to adapt with health system challenges and creating synergies among polarities which universally been encountered by every country. Therefore, flexibility of each stakeholder will be necessary in order to manage tensions exemplified by preceding polarities in health care. Careful assessment of each nation’s economic, political and social conditions and epidemiological pattern of disease will allow leaders to select appropriate health policy strategies and to determine the resources necessary for Family Medicine to grow and contribute to health system improvements. Strategies for changes toward implementing Family medicine approach could be initiated by presenting evidence in which factual information and arguments emphasizing the benefit of it. It is also necessary to show living examples by doing side-visits and case studies to successful family medicine program. Improving Health Care System This chapter reviews the goals, functions and values of health care systems. It also describes common challenges that undermines their successful implementation and outlines strategies to respond to these challenges. It provides the context for assessing the contributions that family medicine can make to people’s health as an integral component of health care systems. The goals of health care system are to achieve optimal level of health as define by The World Health Organization at the smallest possible discrepancies in health status among individuals and groups. Therefore, health care systems should consist of several functions such as providing health care services, generating human and physical resources, financing and collecting data to inform planning and policy development. Furthermore, responsible leadership should direct and coordinate these interdependent functions to achieve the best possible outcomes. The importance of applying basic fundamental values of health care system is also covered in this subject. The values include quality, equity, relevance and cost effective.. In short, health care system of every country should provide a high quality of health care services possible at an affordable cost of the government and individual. The services should also equally assessable to everyone and relevance to the majority health problem of every country. In this topic, the trends affecting health service delivery are also covered such as burden and changing pattern of disease, ageing and population growth, globalization and immediate challenges. The importance of primary health care and its implementation strategies is also discussed to face those challenges. Uniting stakeholders through partnership is essential at Udayana University Faculty of Medicine, DME Page 25 Study Guide Health System-Based Practice 2015 the desGNing and implementing primary health care for achieving the optimum health status of the people. SCENARIO & LEARNING TASKS SYNOPSIS OF “JOHN Q” MOVIE Several concepts of Health System Based Practice that you can see in the movie: 1. Health care system in America uses social and private health insurance system. It can be seen in the movie while John Q brings his son to the hospital, he is asked to show the health insurance card at the receptionist. 2. Communication is an important thing in health care system. We can see in the movie, the doctor and the head of the hospital call John Q and his wife to explain their son’s condition. The doctor explains the condition of the patient and the alternative treatment. It is very important to use language that can be understood by the patient’s family. The head of the hospital explains about the cost of the treatment and John Q’s health insurance. 3. Health care system using health insurance has several models such as HMO, PPO, IPA and IPO. There is a scene that shows the first insurance followed by John Q is PPO. In PPO model, a company must pay a quite expensive premium. The company where John Q works then changes his insurance into HMO because he becomes a part time worker. The insurance is changed without any communication with John Q. Because of that change, John Q cannot get full treatment for his son. 4. Note: In HMO system, clients must pay a fixed amount of money and get the health services that are appropriate to the premium (contract). It has been arranged since the first contract. HMO will pay a doctor based on the standard in the contract, and then the doctor cannot make an additional examination even though it is needed by patient. 5. A nurse in the movie says that the heart disease suffered by John Q’s son cannot be detected because the health insurance only covers particular examination. 6. Health care system of a country is also influenced by its political condition: 1. The head of the hospital says that changing the health care system needs the legislative involvement. 2. There are different opinions in the community. People who are contra say that there are still a lot of people who cannot afford the health services. On the other hand, the government tries to emphasize the importance of a country’s authority to deliver health services. 3. It can be seen that government wants to hide the real situation because there will be a general election soon. 7. The mass media has various roles in disseminating the real situation. It can help the health care system to be better in the future. Task 1 1. Discuss in your group the importance of health care system for a country. Discussion should include the objectives of the government and the other stakeholders’ roles in the health care system. The discussion should also cover the challenges that might be faced in developing the health system and the dilemmas that need to be anticipated. Udayana University Faculty of Medicine, DME Page 26 Study Guide Health System-Based Practice 2015 2. Discussion should be expanded to values that are included in national health care system. What trends and challenges that might appear in the future of health services? What strategies should be prepared to solve the problems? 3. Discuss about the possibility of family medicine in national health care system. How is the possibility of the role of Family Medicine in Indonesia and Malaysia’s Health Care System? Through which steps Family Medicine possibly to be introduced in those countries? Discuss in your group the phenomena of health care system implementation; please refer to the movie presentation. 1. Why did the hospital refuse to deliver complete treatment to John Q’s son? 2. How many and what institutions that were responsible to cover John Q’s son hospitalization? 3. Why did John Q feel that his son has the right for hospitalization without any additional expectations? 4. Refer to the above phenomena and discuss the background of health care financing. 5. PPO and HMO give health service based on contract, not comprehensive care. Please discussed within the group, what type of health insurance that implemented by PPO or HMO? Is it social, regulated private or voluntary private insurance? 6. What are the duties of the government to solve the problem of highly cost health care? 7. Explain the relationship between politics and health care service in the movie. Self assessment 1. How are the roles of the government in health care system? 2. Describe several factors that influence health status of the people! 3. Describe stakeholder’s roles in health care system! 4. Explain challenges that are faced by every country in arranging health care system! 5. What dilemmas are possibly to appear in developing health care system? Explain your answer! 6. What are the roles of Family Medicine in health care system? Explain your answer! 7. Describe several steps that should be taken in introducing family medicine! 8. 9. What will be the ultimate objective of health care system? Explain your answer! Describe several functions of health care system! 10. Describe problems and challenges that are possibly to be faced by every country in developing health care system. 11. Explain why delivering Primary Health Services has an important role in health care system. 12. What strategies must be prepared to solve the problems in developing health care system? Explain your answer! Udayana University Faculty of Medicine, DME Page 27 Study Guide Health System-Based Practice 2015 Day 2 - 3 MODULE~2 Health Indicators and Health Services Related Problems DR. Luh Seri Ani, SKM., M.Kes AIM: Demonstrate ability to provide health services in accordance with a country’s health system LEARNING OUTCOMES: 1. 2. 3. 4. Describe health problems using health indicators Describe definition and areas of health care system Explain the relationship among people, health provider and finance state in health delivery system. Explain the importance of implementation of health care system as a solution of health problem CURRICULUM CONTENTS: Health Indicators and Health Services Related Problems ABSTRACT (References: Gan GL, et al, pp.14-21) There are three dimensions of health delivery service namely: patient, health provider and payment system. In general, the medical service is expensive, because it implements high competency of human resources, sophisticated medical technology and some kinds of drug regiments. If there is no medical guarantee (insurance) system, patient often complaints a high cost of medical service that is not affordable. This problem usually appears in countries where there is no social health guarantee systems conducted by the state or health insurance. SCENARIO AND LEARNING TASKS Task 2 Based on Primary Health Centre’s data, health indicators of the sub-district displayed in table below: Udayana University Faculty of Medicine, DME Page 28 Study Guide Health System-Based Practice 2015 Table 1. Health Indicators of Sundari Loka Sub District, 2006. Indicators Rate 1. Infant Mortality Rate (per 1000 life birth) 68.0 2. Under five mortality Rate (per 1000 under five children) 81.0 3. Mother mortality rate (per 100,000 live births) 450 4. Crude mortality rate (per 1000 people) 6.5 5. Life expectancy (year): - 55 Males Females 60 6. Under weight birth (%) 25 7. Children with Protein Energy Malnutrition (%) 40 8. Latrine occupation (%) 40 8. Interpret the community health status in sub-district of Sundari Loka year 2006 (Compare to data in Indonesia (available in Gan, G.L.)) Self Assessments: 1. Describe several aspects that are related to health problem and health care services. 2. Explain the rights and duties of medical doctor as a health provider in health care system. 3. Describe the prevalent health problems related to health care services in a clinic (hospital). 4. What necessary choices that should be prepared to anticipate the health problem? Udayana University Faculty of Medicine, DME Page 29 Study Guide Health System-Based Practice 2015 MODULE~3 Health Care System in Several Countries dr. I Nyoman Sutarsa, MPH AIMS: Demonstrate ability to provide health services in accordance with a country’s health system LEARNING OUTCOMES: 1. Describe various types of health care system which have been or being adopted by a certain country. 2. Explain advantages and disadvantages of each system. 3. Describe the role of government and private sector in each system. 4. Describe various professions in health care system. 5. Explain the effect of health care financing to the health status of people. 6. Describe basic principles of WHO recommendation to the National Health Care System CURRICULUM CONTENTS: Health Care System in Several Countries ABSTRACT (References: Taylor, RJ, pp.133-144 & Boelen C, et al, pp.1-36) The topic covers a wide range of Health Care System which has been or being adopted by many countries. In one hand, such system is totally own and control by the government (totalitarian) while the other is totally private (liberal). In addition, combination of the two systems is also being practiced by many countries in which government and private working side by side in synergy. Description of advantages and disadvantages of each system and the role of primary care/private sector are also covered in this topic. Further description concerning the role of various professions in Health Care System and allocation of fund are also discussed in this topic. No matter which Health System is adopted, the basic principle of WHO recommendation should always be put into consideration which include optimum health status of people, responsiveness and fair financing. Udayana University Faculty of Medicine, DME Page 30 Study Guide Health System-Based Practice 2015 SCENARIO & LEARNING TASKS Task 3 1. Discuss in the group about 3 types of National Health Care System. The discussion should also include the advantages and disadvantages of each system. Give at least 1 example the country that adopting each system! 2. Discuss about the role of the government and private sectors in each system! 3. Identify various types of professions taking part in National health Care System and estimated budget allocation among them depending upon the economic status of the country. 4. Discuss in the group about possible health seeking pattern of family in each types of Health Care System if each of the following is happening: a. One family member is suffering from pink eyes. b. A child in the family suffering from short breathing, coughing and extreme raise of body temperature! c. One family member suffering from prominent chest pain followed by cold sweating. He has been experiencing similar symptoms previously! d. A 60 years old grandfather is suffering from chronic coughing and blood strip in his sputum. He also lost his appetite and body weight. Self Assessment 1. Describe 3 types of National Health Care System which have been or being adopted and give at least 1 example of the country! 2. Explain the advantages and disadvantages of each system! 3. What is the role of the government and private sectors in each system! 4. Define various types of professions and their role in National Health Care System and average budget allocation among them depending upon the economic status of the country! 5. Describe 3 basic fundamental principles of WHO recommendation that should be considered in developing National Health Care System! Udayana University Faculty of Medicine, DME Page 31 Study Guide Health System-Based Practice 2015 Day 4 - 5 MODULE~4 National Health Care System of Indonesia 2012 dr. I.B Wirakusuma, MOH DR. dr. I Wayan Weta, MS, SpGK _____________________________________________________ AIMS Demonstrate ability to provide health services in accordance with a country’s health system LEARNING OUTCOMES: 1. Explain the objectives of SKN. 2. Describe the subsystems in SKN including: a. Health services. b. Health financing. c. Human resources. d. Drug & health facilities. e. Community empowerment. f. Health management 3. Describe relationship among sub systems. 4. Describe the application of SKN CURRICULUM CONTENTS: National Health Care System of Indonesia 2012 ABSTRACTS (References: Gan GL, et al, pp.14-21; SKN 2012, pp.1–97; Azwar A.) Indonesia National Health System (SKN) 2012 is the order that organizes all Indonesian nation resources through integrated, and synergisted approaches, for guaranting the optimal public health status, as a representative of people wellbeing, that has been mentioned in preface of Indonesian Constitutions (UUD 1945). SKN 2012 consists of six sub systems namely: 1. Health care service 2. Health financing 3. Human health resources 4. Drug and health facilities 5. Community empowerment 6. Health management Udayana University Faculty of Medicine, DME Page 32 Study Guide Health System-Based Practice 2015 SCENARIO & LEARNING TASK As a developing country with population more than 200 million, Indonesia has complex health problems. The average per capita income is 680 US dollar per year. More than 30% of the population is under the poverty line. Thirty percent of the health financing is from government and 70% is from community. Most of the government’s funding is for public services while the community funding is for private services. About 80% of the community funding is available from fee for services and 20% is from insurance. Based on the gross per capita income, only 2,5% of it is allocated for health financing. Because most of the population is not covered by health insurance, they don’t depend on any particular health services. The authority of health provider is quite high. People are often unable to pay health services especially in a hospital. They are even getting poorer, because they have to spend almost all of their money to pay the health services. Task 4 1. 2. 3. 4. 5. What components should be considered to find the solution of various problems above? How is the application of public and private health services in Indonesia? How public and private services will be applied based on SKN 2012? Can SKN 2012 give the solution of all problems above? Explain the several possibilities! What facilities need to be prepared and optimal zed in order to apply the SKN 2012 concept? Self Assessment 1. What is the background of SKN 2012? 2. What are the subsystems of SKN 2012? What are the relevancies of each subsystem toward health problems in Indonesia? 3. Who are the subjects of SKN 2012? What are the roles of each subject? 4. How is the financing system of public health services based on SKN 2012? 5. How is the financing system of private health services based on SKN 2012? 6. How should the following system be done to deliver comprehensive, holistic, integrative and continuous services? a. Financing system b. Services approaches c. Teamwork of the subjects Udayana University Faculty of Medicine, DME Page 33 Study Guide Health System-Based Practice 2015 MODULE~5 Puskesmas as a Primary Health Care Service dr. I.B Wirakusuma, MOH DR. dr. I Wayan Weta, MS, SpGK _____________________________________________________ AIM Demonstrate ability to apply the concept of management to provide health services at primary level. LEARNING OUTCOMES (Reference: Azwar, A.) 1. 2. 3. 4. Describe the structure of primary health services in puskesmas. Explain the basic programs and the additional programs in puskesmas. Describe the financing system of basic programs in puskesmas. Explain the application of private health services management based on the finance resources: a. Askes b. Askeskin/JPKMM c. General patients 5. Describe the application of private and public health services management in puskesmas. CURRICULUM CONTENTS Puskesmas as a Primary Health Care Service SCENARIO AND LEARNING TASK Scenario: Sub-district of Sundari Loka with population of 30,000 people, most of them work as farmers, their income not constant depend on climate and natural condition, the average income only sufficient for simple daily life. In Sub-district there are one Public Health Center (PHC/Puskesmas), 4 health satellites (Puskesmas Pembantu), and 8 village’s midwifes (bidan di desa). There are also 2 private medical doctors, 4 private midwifes, and 2 nurses. Beside of the conventional health provider, there are also 3 traditional healers. The six basic programs that are served by Public Health Center namely: 1. 2. 3. 4. 5. 6. Mother and child health and family planning. Communicable and non communicable disease program Environmental health Community nutrition program Health education Polyclinic services Udayana University Faculty of Medicine, DME Page 34 Study Guide Health System-Based Practice 2015 People who go to public health center pay less than those who go to private health services. People choose whether the public or private health services, depend on their perception and financial situation. Task 5 1. Describe the characteristics and examples of public health services! 2. Describe the characteristics and examples of private health services! 3. Discuss the differences between public and private health services! 4. Based on the above scenario, discuss how the health care system in Sundari Loka is! 5. Discuss the concept of integrated health services! 6. Discuss the concept of comprehensive health services! Self Assessment 1. Differentiate the finance resources, facilities and human resources between public and private health services! 2. Discuss the differences between structured and unstructured health services! 3. Discuss the differences between structure of public health services and private health services! Day 6 - 7 MODULE~6 Primary Health Care and Health Promotion dr. Komang Ayu Kartika Sari, MPH dr. Ni Luh Putu Ariastuti, MPH AIMS: Demonstrate ability to provide health services in accordance with a country’s health system. LEARNING OUTCOMES: 1. 2. 3. 4. Describe major factors affecting health status Define Health Education and Health Promotion Explain the aspects of health promotion in the Ottawa Charter Explain the strategic role of Health Education and Health Promotion in achieving optimum health status of every individual Udayana University Faculty of Medicine, DME Page 35 Study Guide Health System-Based Practice 2015 CURRICULUM CONTENTS: Primary Health Care and Health Promotion ABSTRACTS (Reference: FHI, WHO, Jirojwong, S.) This topic contains major factors affecting health status. It also describes the definition of Health Education and Health Promotion and their strategic roles in improving health status of every individual in the community. It explains how the aspects of health promotion conceptualised by The Ottawa Charter. The topic also describes some health behaviors that need to be practiced by every individual in order to be able to maintain his/her health status. SCENARIO & LEARNING TASKS Task 6 Discuss in your group the following topics or aspects of Public Health: 1. 2. 3. 4. 5. 6. The definition of Public Health The definition of health Major factors affecting health status The definition of Health Education and Health Promotion Aspects of health promotion in the Ottawa Charter The strategic role of Health Education and Health Promotion in achieving optimum health status of every individual Udayana University Faculty of Medicine, DME Page 36 Study Guide Health System-Based Practice 2015 MODULE~7 Basic Theories underlying Health Promotion dr. Komang Ayu Kartika Sari, MPH dr. Ni Luh Putu Ariastuti, MPH AIM: Demonstrate ability to provide health services in accordance with a country’s health system. LEARNING OUTCOMES: 1. 2. 3. 4. Explain basic theories underlying Health Education and Health Promotion Describe basic principles of diffusion of innovations and the decision making process Summarized major theories of behavior change Comprehend Health Promotion glossary CURRICULUM CONTENTS: Basic Theories underlying Health Promotion ABSTRACT (References: FHI, WHO, Nutbeam, D.) This topic discusses basic theories underlying Health Education and Health Promotion and their relationship to basic principles of diffusion of innovations and decision making process. Moreover, the topic also summarized major theories of behavior change and health promotion glossary. SCENARIO AND LEARNING TASK Task 7 Discuss in your group the following topics or aspects of Public Health: 1. 2. 3. 4. 5. 6. Some basic theories underlying Health Education and Health Promotion Basic principles of diffusion of innovations and the decision making process. Classification of individual based on their rates of adoption Major theories of behavior change. Describe relationship between decision making and stages of behavior change. Comprehend Health Promotion glossary. Self Assessments: 1. 2. 3. 4. 5. Describe the definition of Public Health. Compare the previous definition of health with the latest one. Describe 4 major factors affecting health status. Which one is the most prominent? Describe the definition of Health Education and it gradual sifts to Health Promotion. Explain the strategic role of Health Education and Health Promotion in achieving optimum health status of every individual. 6. Describe some basic theories underlying Health Education and Health Promotion. Udayana University Faculty of Medicine, DME Page 37 Study Guide Health System-Based Practice 2015 7. Describe basic principles of diffusion of innovations and the decision making process. 8. Describe classification of individual based on their rates of adoption and their specific characteristics. 9. Explain 4 major theories of behavior change. 10. Describe relationship between decision making and stages of behavior change. 11. Describe 7 core definitions of Health Promotion and some important terminology being used in Health Promotion. Day 8 - 9 MODULE~8 Health Management in Health Services dr. Komang Ayu Kartika Sari, MPH DR. dr. GN Indraguna Pinatih, MSc, SpGK, Akp AIMS: Demonstrate ability to apply the concept of management to provide health services at primary level LEARNING OUTCOMES: Describe the principles of management in health care services. CURRICULUM CONTENTS: Health Management in Health Services ABSTRACT (Reference: Gan GL, et al, pp.78-87) A doctor is often the manager of the practice. Managing is to get work done through the efforts of others. Managing is also producing an aoutput from input and process. The four basic functions of a manager are planning, organizing, leading and control. The process whereby one person influences the thoughts and behaviors of others is a definition of leadership. Between the extrems of complete autocracy on the one hand and a totally permissive approach on the other, there exists a continuum of possible leadership styles. Each of us has a basic personal leadership style and may be motivating or demotivating depending on the situation. An insight of the range of personal leadership styles helps us to choose what is appropriate for the situation. Udayana University Faculty of Medicine, DME Page 38 Study Guide Health System-Based Practice 2015 SCENARIO & LEARNING TASKS TASK 8 CASE-1 Dr. Drupadi will make a family medicine clinic in Denpasar. It needs knowledge and basic competencies in management. a. Discuss some definitions of management. b. What aspects needed to be managed in a clinic? CASE-2 Dr. Drupadi thinks that finally she has to be the manager of his clinic. If she doesn’t want to, she has to choose somebody with good qualification. a. What skills must be owned by a manager? b. What are the roles of a manager in leading a clinic? c. What is the meaning of leadership? CASE-3 In a meeting (conducted after the clinic was made), dr. Drupadi tells all of her staff that purposes of the clinic were responsibilitiy of all staff to achive them. a. Which leadership model is applied by dr. Drupadi? b. Explain the reasons of your answer! SELF ASSESSMENT 1. Describe the definitions of management. 2. Explain the meaning of planning in management. 3. Explain in your own words the meaning of leading in management. What do we need to be a good leader? 4. What components must be in control process? 5. Describe in your own words the definition of human skill. 6. What is the meaning of leadership? 7. Make a comparation of the task, group and individual need leadership model! 8. Describe the meaning of personal leadership! Udayana University Faculty of Medicine, DME Page 39 Study Guide Health System-Based Practice 2015 MODULE~9 Health Workforce and Human Resource Management dr. Komang Ayu Kartika Sari, MPH DR. dr. GN Indraguna Pinatih, MSc, SpGK, Akp AIM: Demonstrate ability to apply the concept of management to provide health services at primary level. LEARNING OUTCOME: Comprehend the concepts of managing people in health services CURRICULUM CONTENTS: Health Workforce and Human Resource Management ABSTRACT (Reference: Gan GL, et al, pp.78-87) Motivating staff to contribute their best is a big challange. There is a need for an ongoing appraisal of the motivation level of staff. Channels for upward communication must be open for staff dissatisfaction to be identified and dealt with before it has caused widespread motivational problems. People management also requires the ability and willingness to deal with unpleasant issues, such as grievances, discrepancies and absenteeism. SCENARIO AND LEARNING TASK Task 9 CASE-1 Cleaning services have a lot of duties including cleaning the clinic and open the clinic’s door every morning. Ambulance’s driver has duties to bring the referred patients to hospital and take the doctor to patient’s house for oncall services. a. Which model of leadership that is needed for those cases? b. Discuss your reason in your group! CASE-2 Dr. Drupadi notices that her staff have different motivation. There are dilligent staff while the others will take the job only if they are asked to. a. What are the possible cause of different motivation level of staff? b. What should be done to increase the motivation of staff in the clinic? Udayana University Faculty of Medicine, DME Page 40 Study Guide Health System-Based Practice 2015 CASE-3 Sinta, the clinic nurse, reports that there are fewer antibiotics in the place than they should be. Ambulance driver has already been absent for 4 times because of sickness and out of town. Dr. Bima and dr. Arjuna complained that their rooms are less ventilated. a. What problems are facedby dr. Drupadi? b. Which problem must be solved soon? c. How to solve the absence problem? CASE-4 Dr. Drupadi’s clinic has been operated for 2 years, she wants to develop it (open the new clinics) in Kuta. a. What sould be done by dr. Drupadi? b. Explain the steps that must be taken by her. c. Explain the meaning of SWOT analysis. d. Are point b and point c different? Self Assessments: 1. 2. 3. 4. 5. 6. Explain the diagram that shows the scope of human resources management. How many factors that influence motivation? Explain each of the components! Describe the meaning of grievances and give 1 example. Describe the meaning of discrepancies and give 1 example. Explain how we can solve absenteeism problem! Describe the meaning of one minute manager! Day 10 - 11 M O D U L E ~ 10 - 11 Quality Management 1 & 2 dr. I Nyoman Sutarsa, MPH dr. Ni Luh Putu Ariastuti, MPH AIM: Demonstrate ability to apply the concept of management to provide health services at primary level LEARNING OUTCOMES: 1. Describe basic concept of quality in health-care 2. Describe how to manage health-care in whole system for quality improvement Udayana University Faculty of Medicine, DME Page 41 Study Guide Health System-Based Practice 2015 CURRICULUM CONTENTS: Quality Management ABSTRACT (References: Gan GL, et al, pp.108-110; Boelen C, et al, pp.148-160; WHO. Quality of Care) There are wide variations in standards on health care delivery within and between health care systems. The aim of managing quality is optimizing resource use and expanding coverage based on a specified standard. The process of improving quality in health-care would be based on sound local strategies in order to achieve the best results by optimizing resources use and new investment. Quality of Health Care Quality in health care is simply defined as care that meets or exceeds expectations, both technical and patient satisfaction. In can be evaluated by three indicators those are (1) structure personnel, facilities, equipment, organization and coverage), (2) process (activities with continuous monitoring and evaluation), and (3) outcomes (health status of patient or community). Dimensions of quality in health care would be (1) effective (improved health outcomes), (2) efficient (maximize resource use), (2) accessible (timely and geographically), (4) acceptable (patient centered needs), (5) equitable (does not vary in quality), and (6) safe (minimize risk and harm). Besides that health care would be also comprehensive (includes primary, secondary and tertiary prevention), and appropriate (evidence based). The Process of Quality Improvement Managing quality in health care means that to follow the process of quality improvement. This process includes three steps those are (1) analysis (stakeholder involvement, situational analysis and confirmation of health goals), (2) building strategy (defining quality goals and choosing interventions for quality), and (3) implementation (process of implementation and monitoring progress). However, the quality intervention would be determined by six dimensions such as leadership, management information system, patient or population engagement, regulation (standard), organizational capacity, and the model of care. Implementation change may be needed that based on monitoring progress or self auditing process. SCENARIO & LEARNING TASKS Task 10 There are wide variations in standards on health-care delivery within and between healthcare systems. The aim of managing quality is optimizing resource use and expanding coverage based on a specified standard. The process of improving quality in health-care would be based on sound local strategies in order to achieve the best results by optimizing resources use and new investment. 1. Describe quality of health-care based on point of view of patients and healthcare providers. 2. Describe dimensions of health-care quality, and give example for each dimension. Udayana University Faculty of Medicine, DME Page 42 Study Guide Health System-Based Practice 2015 3. Describe assessment of health-care quality, and what indicators do we use? 4. Describe the difference between quality goals and health goals, and give examples. 5. Describe seven activities (elements) those are grouped into three categories (analysis, strategy and implementation) for quality improvement, and give examples foe each element. 6. Describe six domains of quality intervention, and give examples for each domain. 7. Explain what quality assurance program in health-care is. 8. Explain the importance of self-auditing or self evaluation for quality assurance program, and what aspects? Task 11 Case: MELATI Health Center Health Centre of Melati that located in suburban area was always crowded by ambulatory patients, especially on Monday. Some patients often stand on their own legs in a relative inconvenient space because of unfriendly weather and limited seats in the waiting room. That was quite common; the patients have to wait 2 hours until they got turn of medical service. However, Melati Health Centre becomes the first choice of community for seeking health services, because of some reasons. The price of visit to Melati Health Centre is relatively very cheap, and the location is not so far from most of the community. Monday at 9.30 AM: Conversation between patients in waiting room Mrs Ani: “Finally the doctor is coming too. Last week I had same experience, wait from 7 AM, and did not know what time the doctor would come. Then I had turn at 10 AM”. Mrs Mur: “There are 2 doctors here, which one you will meet?” Mrs Ani: “Who knows, which doctor would come. I just need my daughter get examination and medicine”. Mrs Mur: “What’s happened with your daughter?” Mrs Ani: “At the beginning my daughter was suffered from high fever, and the followed by bad coughing. That was 4 four days already. Three days ago she was treated here but she won’t recover. Even she was getting difficulties to breathe and fever again. To go to private doctor must be very expensive, maybe I can’t afford it”. Mrs Mur: “Yes, the condition of my son is almost same as your daughter. Two days ago I came about 11 AM. One staff here got angry with me, why I came late at afternoon, and I forgot to bring the control card of my son. At that time there was no doctor, because of official meeting somewhere. My son was treated by one midwife, and up to now he won’t recover”. Udayana University Faculty of Medicine, DME Page 43 Study Guide Health System-Based Practice 2015 At 10 AM the same day: between doctor and patient Doctor: “What’s happened with your daughter?” Patient: “My daughter was treated three days ago, but she still suffered from high fever. Please Doctor, help my daughter”. Doctor: “Your daughter was 4 years old, yes? (Saw the card). Please, lying down there (pointed the bed). Woo, your daughter is quite ill” Patient: “Please help doctor, I want my daughter get recover” Doctor: “Ye, if she still gets fever, please control again (writing prescription). Please, you get medicine next door”. At 11 AM: at Pharmacy of Health Centre Pharmacy’s staff: “Mom, there was no stock of antibiotic that was written in this prescription. The doctor should write other kind of antibiotic” Patient’ mother: “Do I have to turn back to the doctor?” Pharmacy’s staff: “No need Mom. Maybe the antibiotic could not be changed. (the pharmacy’s staff knows that was no stock of other antibiotics). Mom, there is one pharmacy not so far from here. Maybe you can buy the antibiotic over there. Patient’ mother: “…………… ?????” (I am worried that my money is not enough). Questions: 1. From the above case, please analyze how was the health service quality of Melati Health Centre? Analyze each dimension of quality! 2. What kind of strategy that you can implement in order to increase the health service quality in that health centre? Self Assessment 1. 2. 3. 4. 5. Could you explain what means by quality in health-care? How you will implement each dimension of quality in health-care delivery? How you can optimize resource use for better quality of heal-care. Could you explain building strategy for quality in health-care? What indicators do you use to assess quality and health outcomes? Udayana University Faculty of Medicine, DME Page 44 Study Guide Health System-Based Practice 2015 Day 12 - 13 M O D U L E ~ 12 Management of Facilities, Information, and Finance DR. dr. GN Indraguna Pinatih, MSc, SpGk, Akp AIM: Demonstrate ability to apply the concept of management to provide health services at primary level LEARNING OUTCOME: 1. Explain the concepts of supplies and stores management (SSM). 2. Describe how to control discrepancies in a clinic. 3. Comprehend the concepts of managing information and finance. CURRICULUM CONTENTS: Management of Facilities, Information, and Finance ABSTRACT Managing Facilities (Reference: Gan GL, et al, pp.87-90) The supplies and stores system deals with ordering, receipt, maintenance, and issue when required. The supplies can range from drugs and pharmaceuticals to syringes and needles as well as general use items like stationery. Stocks of pharmaceuticals and medical require close monitoring to ensure they do not deteriorate or reach expiry dates, they are not pilfered and their storage and usage comply with existing regulations. The operating principles of supplies and stores management are: have an efficient system, determine stocking levels, have a storekeeper, insist on bin cards, have an ordering system, have a store ledger, have defined procedures, conduct regular stock takings and have a system to deal with problems. Managing Information (Reference: Gan GL, et al, pp.90-97) Medical records are more than a documentation of clinical details. Properly kept and used, they allow us to see the problem solving process from which we can deliver better care. An effective record keeping system contributes to the standard of care. Attention paid to how medical records are organized, filed, and maintained is integral to effective practice. The problem oriented medical record (POMR) is better than the source oriented medical record (SOMR) and we should progress towards it. Udayana University Faculty of Medicine, DME Page 45 Study Guide Health System-Based Practice 2015 Managing Finance (References: Gan GL, et al, pp.97-107; Boelen C, et al, pp.135-143; Sulastomo, pp. 173180) Financial management consists of: keeping proper records of income, expenditure and profit; preparing financial statements at the end of accounting period; analysing financial statements and taking the necessary actions; implementing inventory and stock control processes; acting on discrepancies; ensuring that financial records are audited and developing financial plans. It is essential to have accurate knowledge of the financial status of the practice in order to plan ahead. This is in turn dependent on keeping proper records for income, expenditure and profit. It is also important to have summaries of the financial activities of an organization, which contain information useful to management (financial statement). Financial audits and financial planning, as the other activities, have purposes to ensure accountability in the use of financial and material resources and to develop the organization’s budgets (operating budgets and financial budgets) respectively. SCENARIO AND LEARNING TASK TASK 12 CASE 1 After the medicines have been lost several times, dr. Drupadi evaluates the system of managing facilities and utilities in her clinic. a. b. c. d. e. f. What are the principles of managing facilities and utilities? Explain briefly each of the principles! Describe the possible causes of discrepancies in facilities and utilities management. What efforts should be done to prevent the discrepancies happened again? What rules should be determine in managing drugs and chemical agent? What principles should be noticed in managing drugs and vaccines? CASE-2 Dr. Drupadi’s clinic is going very well. The number of patients has already increased from 510 patients per day in first few years, to 20-30 patients per day now. The nurse finds difficulties to look for medical records of the patients. The doctor also finds difficulties in making diagnosis because the previous medical records cannot be found. a. b. c. d. e. f. What are the benefit of using medical records? Why is it very important? What are the principles of managing patients’ medical records? What are the differences between SOMR and POMR? Which one is better? What steps should be taken to manage the medical record better? How are the principles of computer usage in managing medical records? How is the using of PDA to look for an information? Udayana University Faculty of Medicine, DME Page 46 Study Guide Health System-Based Practice 2015 CASE-3 One day, Dr. Drupadi saw somebody in medical record room whom are known as a boyfriend of a nurse in that medical record room. She saw him openned and read several medical records on the nurse’s table. After gave advices and told him to go out, dr. Drupadi called some nurses that worked in medical records room. a. What information will dr. Drupadi tell to her nurses? b. When are medical records able to be informed to people other than patients? CASE-4 After being operated for 5 years, dr. Drupadi’s clinic shows an increasing of the number of patients. However, she has never got a high income even though the finance capital has never runned out. Her wish to develop a clinic in Kuta has not been realized. All this time, dr. Drupadi manage her clinic’s finance, helped by one of her nurse. 1. What should be done to manage a clinic’s finance? 2. What is the meaning of: a. financial records? b. financial statement? c. financial audit? 3. Do we need to do an external audit? CASE-5 Based on an audit result of a public accountant, the doctor and the nurse has already made a complete finance records. However dr. Drupadi has not made a good financial planning, particularly in calculating the unit cost of each services in the clinic. a. What is the meaning of financial planning? b. What is the definition of unit cost? c. Why is it mportant to determine the unit cost?6 CASE-6 Based on the audit result, dr. Drupadi then calculates the unit cost of her clinic’s services. First, she determines the components such as fix cost, operational cost and maintenance cost. Then she determines the output of the working unit which is an outpatient care and calculates the total of fix, operational and maintenance cost. After that she divides the total cost by production of each working unit to get the unit cost. At last, she determines the marginal cost to get the tariff. a. What is the definition of fix cost? Give the example! b. What is the deinition of marginal cost? Give the example! c. Is unit cost the same as tariff? Discuss your answer! Self Assessments 1. Give some examples of “supplies”! 2. Why do we need to monitor drugs and chemical agents stock? 3. What is the meaning of “first in, first out” system (FIFO)? 4. How to manage a cold chain for vaccines? Udayana University Faculty of Medicine, DME Page 47 Study Guide Health System-Based Practice 2015 5. What is the meaning of discrepancies in managing facilities and utilities? Give some examples of its possible causes! 6. What is the definition of medical records? Why do we need medical records? 7. How many groups of people are allowed to read the medical records? Explain who they are! 8. What should be done to manage information using a computer? 9. Why is managing finance important for family doctor’s practice? 10. What is the meaning of financial records? Explain in your own words and give some examples! 11. Mention the steps of managing finance! 12. What is the important activity in financial planning? 13. What is the definition of financial audits? 14. What is the meaning of finance analysis and unit cost? Why do we need to know a unit cost? Udayana University Faculty of Medicine, DME Page 48 Study Guide Health System-Based Practice 2015 M O D U L E ~ 13 Managed Care DR. dr. I Wayan Weta, MS, SpGK AIMS: Demonstrate ability to apply the concept of management to provide health services at primary level LEARNING OUTCOMES: 1. Explain the concept of managed care. 2. Describe the types of managed care. CURRICULUM CONTENTS: Managed Care ABSTRACT (References: Sulastomo; Thabrany H.;Subawa) There are two models of health care depend on their financing systems, namely: 1. Indemnity care: post paid direct payment, fee for service-out of the pocket, curative oriented. 2. Managed care: prospective payment, capitation, comprehensive care oriented. Managed (health) care is the system that integrates both financial and health care services. Health care services through managed care approach will produce more cost-effective services. Characteristics of managed health care are: - Developing financial and health care system - Implementing family medicine concept - Implementing referral care system - Implementing prospective payment system - Applying standard price of drugs SCENARIO & LEARNING TASK Case: Dr. Ketut Cespleng is a famous general practitioner in Denpasar. Not less than 15 patients get treatment in 2 hours at his practice. His equipments are modern such as USG, ECG, roentgen, laboratory, and drug store beside his practice. Putu Gd Ajum, a patient, came to his practice complaining headache, nausea and fever since in the morning. To Udayana University Faculty of Medicine, DME Page 49 Study Guide Health System-Based Practice 2015 make the diagnosis, dr. Ketut did an anamnesis, physical examination, additional examination such as ECG, USG, roentgen and laboratory examination, and then give 5 branded medicine to Putu Gd Ajum. He then paid (a fee for services) Rp 555.500,-. Putu Ajum was very satisfied to get complete medical care and many kinds of medicine; the doctor was also very friendly. Spending a lot of money was not a problem for him because he was very rich. Task 13 Discuss in your group: 1. Did dr. Cespleng use the managed care approach in his practice? Explain the reasons of your answer! 2. What were the possible reasons why dr. Cespleng uses that kind of practice method? 3. How is the cost effectiveness of the medical care given by dr. Cespleng? 4. Mention several factors why dr. Cespleng’s patients feel satisfied with the services! 5. Did his ability to satisfy the patients mean he had already worked professionally? 6. Describe several consequences that are possible to happen if the above services are applied for patients with health insurance. 7. What are the obstacles of managed care application in Indonesia? SELF ASSESSMENT 1. Describe the differences between conventional indemnity care and managed care. 2. Describe what the backgrounds of managed care concepts (such as HMO, PPO, etc) are. 3. Explain several reasons why managed care concept is applied by almost all countries in the world? 4. 5. What is the meaning of “cost control”? What is the definition of “quality control”? 6. What is the definition of “cost effectiveness”? 7. What are the differences between bipartite and tripartite managed care? Describe the advantages and the disadvantages of those managed care. Udayana University Faculty of Medicine, DME Page 50 Study Guide Health System-Based Practice 2015 Day 14 - 15 M O D U L E ~ 14 Health Insurance and SJSN dr. I Nyoman Sutarsa, MPH AIMS: Demonstrate ability to apply the concept of management to provide health services at primary level. LEARNING OUTCOMES: 1. 2. 3. 4. 5. Explain the basic concept of health insurance. Describe several models of health insurance. Explain the financing system of health insurance. Explain the application of health insurance through SJSN. Describe the application of a managed care in health insurance. CURRICULUM CONTENTS: Health Insurance and SJSN ABSTRACTS (References: Sulastomo; Thabrany H.; Subawa) Insurance is a social device for reducing risk of financial loss, which involves the principle of pooling or co mining separate exposure so that the risk for the group is reduced by the operation of the law of overage. Health insurance includes all such devices with reduces the risk of financial loss from ill-health (Deckerson, 1963, in Sulastomo, 2004). There are three kinds of it namely, social, private voluntary, and regulated private health insurance. Social health insurance is not profit oriented. Private voluntary and regulated private health insurance are profit oriented. There are some differences of sharing risk among these insurances. Social health insurance has most complete sharing risk (rich-poor, ill-health, oldyoung, high risk-low risk), and private voluntary has the least (only ill-health). Social health insurance applies comprehensive health care approach, but in private voluntary and regulated private health services depend on selective contract. Social health insurance is usually conducted by the state, while private voluntary and regulated private are generally operated by insurance companies. Udayana University Faculty of Medicine, DME Page 51 Study Guide Health System-Based Practice 2015 SCENARIO & LEARNING TASKS Case: The populations of CintaDamaiVillage are members of social health insurance program (Jaminan Pemeliharaan Kesehatan Masyarakat/JPKM). They have to pay a same premium of Rp 20.000/family/month. The health services covered by the insurance are comprehensive cares (primary, secondary and tertiary cares). Dr. Koming is acting as the primary health provider in the village. Tut Bagus, a member of the JPKM program, came to see dr. Koming complaining his penis had been swollen. He felt very painful during passing water. He also has morning discharge for several days. He honestly confessed that he had sex with a prostitute several times. Without talking and advising too much, dr. Koming gave the medicine. On the next 3 days, Tut Bagus came back with his wife to dr. Koming’s practice. His wife complained with vaginal discharge and swollen vulva. Dr. Koming then gave a medicine to her. One week later Tut Bagus came back again and complaining of being very weak, difficult to sleep and lost his appetite. Task 14 Discuss in your group: 1. Based on the scenario above, which one of health insurance program was followed by Tut Bagus? Describe the reasons of your answer! 2. Had dr. Koming given a comprehensive care? Explain your answer! 3. Had dr. Koming applied the managed care concepts? Explain your answer! 4. What can be concluded from frequent attendance of Tut Bagus to dr. Koming’s practice? 5. Is there an over-utility aspect? In which component? Self assessment 1. Describe several types of “sharing risk” in health insurance! 2. Explain the differences between social and commercial health insurance! 3. 4. Describe the types of rating based on actuarial analysis! Describe several paying systems to the health provider. 5. Which one of the health insurance program will be implemented in Indonesia? 6. Why should managed care be applied for patients that are covered by health insurance? Udayana University Faculty of Medicine, DME Page 52 Study Guide Health System-Based Practice 2015 M O D U L E ~ 15 Family Medicine Practices: Family as a Unit of Care DR. dr. I Wayan Weta, MS, SpGK AIMS: Apply family medicine approach in primary health services LEARNING OUTCOMES: 1. Describe the definition of a family. 2. Describe the functions of family. 3. Explain the cycle of family development including the main objective in each step. 4. Describe the influence of family toward the health status of its members. 5. Differentiate the characteristics of a happy and an unhappy family. 6. Describe the roles of family doctor in assisting an unhappy family 7. Explain the level of a doctor’s involvement in a family with health problems. 8. Describe the family dynamics that affecting health status of family member. 9. Draw and describe a family genogram. CURRICULUM CONTENTS: Family Medicine Practices: Family as a Unit of Care ABSTRACTS (Reference: Gan GL, et al, pp.56-62) This topic covers a wide range of aspects related to family as a unit of care. It describes who forms a family and how an individual enters and leaves the family. The general role of family is also covered particularly in seeking health care delivery. It also describes reasons of individual to form a family and family life cycle starting from married couple without children until ageing family members and is ended up with the death of both spouses. Each stage of family cycle is completed with its specific role and functions and estimated length of time for each period. The family’s influence on the individual health is also discussed in this subject. In addition, the characteristics of a happy and unhappy family are identified to be used by the physician to give the best possible support for specific health problem to each family. The level of physician involvement to family members suffering a health problem is also specified in this subject. There are a few examples of emergency care and house calls commonly dealt by physician at the front line of health care services. Finally, this topic assesses the family dynamic which includes its structure (genogram) and relationship among members in the family. Udayana University Faculty of Medicine, DME Page 53 Study Guide Health System-Based Practice 2015 SCENARIO & LEARNING TASKS Task 15 1. Discuss about family dynamics covering membership, functions and the role changes in the development cycle. 2. Draw your own family’s genogram and (if possible) explain the meaning of your diagram to your group! Explain generally the social economics status and the relationship among your family member. Is there any genetic disease in your family? Self Assessments 1. Describe the definition of family and how it is formed. 2. Describe the functions of family! 3. Explain the steps of family cycle and the roles in each step! 4. How is the influence of family toward its member’s health status? Explain your answer! 5. Compare the characteristics of a happy family and an unhappy family! 6. How are the roles of family doctor in assisting an unhappy family? Explain your answer! 7. Describe the family dynamics that can influence the health status of its members. Udayana University Faculty of Medicine, DME Page 54 Study Guide Health System-Based Practice 2015 Day 16 - 17 M O D U L E ~ 16 Health Delivery System and Family Medicine Practices DR. dr. I Wayan Weta, MS, SpGK AIMS: Apply family medicine approach in primary health services LEARNING OUTCOMES: 1. 2. 3. 4. 5. Describe the definition of family medicine as a discipline. Describe place and position of family medicine in the health care system. Explain the knowledge and skill that are required in family medicine practice. Compare integrated health activities within and between providers. Describe the application of the principles of family doctor services covering: a. personal care b. primary care c. comprehensive care d. continuing care 6. Explain the coordinative and collaborative aspects using basic approaches of family medicine. 7. Describe the basic approaches of family medicine at the individual, family and community levels. CURRICULUM CONTENTS: Health Delivery System and Family Medicine Practices ABSTRACTS (References: Boelen C, et al, pp.37-48; Gan GL, et al, pp.42-49) Family medicine is a discipline concerns with the provision of personal, primary, comprehensive and continuing health care of individual in relation to their family, community and environment. The central value of family medicine is to anticipate and avoid fragmentation of care and impersonal care brought by subspecialisation and growth of high medical technology. Implementation of family medicine practice must be supported by health care delivery system and prospective payment health insurance. Prospective payment supports the comprehensive care service (especially promotive and preventive), that can not be constructed in post payment system (fee for service). As a good primary health provider, doctor must have basic family medicine competencies. Udayana University Faculty of Medicine, DME Page 55 Study Guide Health System-Based Practice 2015 The competency characteristics of family doctors are in: Attitudes: Patient centre care and attention to doctor-patient relationship Holistic approach to the patient and his/her problem that contribute to ill-health and well being not only physical, but also social and psychological dimensions (the bio-psychosocial model of ill-health) as well as from the family and community. Emphasize on preventive medicine, because it has greater long term impact on health status than curative medicine. Central values of family doctor’s work: Looks after health problem that may be initially unclear. Looks after whole spectrum of age (specialist in breadth, unlike hospital specialist- in depth). Looks after patient not only in consultation room but also at home and other settings. Skill: General clinical skill Special clinical skill: 1. Doctor-patient relationship 2. Communication 3. Skill in managing special groups of patient 4. Solute undifferentiated problems 5. Identify risk and early departure from normality. Skill in resource management Practical management skill SCENARIO & LEARNING TASKS Scenario: A 25 years old woman came to “Sehat” family medicine clinic, complaining that she had been coughing for 1 month. She also experienced fever particularly at night and loosing weight. The patient had worked as a waitress in a cafe and also as a commercial sex worker since 5 years ago. One of her client was suffering from HIV-AIDS and died several days before. Task 16 As a family doctor you are required giving appropriate service. 1. What will you do to apply patient-center care with attention to doctor-patient relationship? 2. How do yo do the holistic approach to this patient? 3. How do you do the preventive medicine to this problem? Who is the target of preventive medicine? Explain your reason! Udayana University Faculty of Medicine, DME Page 56 Study Guide Health System-Based Practice 2015 4. What do you do to solve the undifferentiated/unclear case above? 5. With whom the coordinative and collaborative cares should be done? 6. What approach should you take for the medical team, family and community to solve this problem? Self Assessments 1. What are the differences between family medicine services and conventional general practitioner? 2. What are the authorities and the duties of family doctor? 3. Explain the 7 areas of integrated health services. 4. Describe the principles of family medicine service approach. M O D U L E ~ 17 Disease Management Skills DR. dr. GN Indraguna Pinatih, MSc, SpGk, Akp AIMS: Apply family medicine approach in primary health services LEARNING OUTCOMES: 1. Describe the differences between acute and chronic diseases management. 2. Explain how to help patients to evaluate their conditions. 3. Describe how to educate patients with chronic diseases in order to empower them in diseases management. 4. Describe how to make similar perception of diseases with patients and how to determine the objectives to be achieved together. 5. Explain how to design and to apply the clinical management of chronic diseases. CURRICULUM CONTENTS: Disease Management Skills ABSTRACTS (Reference: Gan GL, et al, pp.145-155) Medical services must be constructed depend on type of illnesses whether acute or chronic disease. There are two approaches of care: doctor centered and patient centered. Doctor centered only works in acute care, not works effectively in chronic disease care. New disease paradigm is needed for chronic disease care. Effective chronic disease care requires two things; the medical care team and an active involved patient (patient centered). Patients must be empowered to solve their problems, they can change their behavior. The patient should be able to set self management goal for their problem. Patient Intervention grouped included into three strategies: Education, Behavior and Affective. Health provider Udayana University Faculty of Medicine, DME Page 57 Study Guide Health System-Based Practice 2015 team must imply the care management process included: Practice guideline, population disease management, case management, health promotion or disease prevention, and clinical information system. Frame work for action of the team is how to: 1. 2. 3. 4. Identify the problem Organize a multidisciplinary team Define core component, treatment protocols and evaluation methods Measure the outcome and aims. The ways ahead those are emphasized in disease management: Providing care that is respectful to patients preferences Educating and supporting patient to self-manage their condition Linking to resources in the broader community Developing and supporting health care providers Reorganizing health system Coordinating care across patients condition Monitoring quality of service and outcome Reorganizing health care financing SCENARIO & LEARNING TASKS Task 17 Case 1: Mr. Nyoman Polos, a 50 years old man, came to his family doctor, dr. Siddhi. He complained about frequent coughing for more than 1 month and sometimes he saw blood strip the sputum. He lost weight and weak. He was diagnosed with tuberculosis (TB) based on the physical and laboratory results. The treatment regimen was given for 6 months. In the first month he had to take 5 different pills every day. For the following 5 months he had to take the medicine twice a week. At the end of the first month he stopped the medication for several reasons such as he felt his complain would not getting better, he lost his hearing and worried about experiencing severe side effects. He then tried to find alternative medication by visiting a traditional healer. Assignments: Discuss in your group: What are Mr. Nyoman Polos’ reasons to stop his medication? If you are his family doctor, what will you do to anticipate the drop out of the treatment? What can you do to empower patients to help themselves? What can you do to the patients’ family to prevent the drop out of the treatment? Try to develop a TB medication system which involves the family to increase compliance. Explain how is the methode of the system! (Read: The DOTS system from WHO) 6. What should be done to prevent transmission of the diseases to the other family members? 7. What approach will you use toward the patients’ behavior using alternative medication? 1. 2. 3. 4. 5. Udayana University Faculty of Medicine, DME Page 58 Study Guide Health System-Based Practice 2015 Case 2: Luh Manis, a 35 years old woman, a housewife, came to dr. Siddhi complaining of feeling thirsty and hungry very often. She also felt weak since few months. Luh Manis loved to eat various food until she gain weight. She was diagnosed suffering from Diabetes Mellitus (DM). The doctor said that the disease could not be totally recovered without controlling her eating habit. The doctor adviced to combine the treatment with life style modification such as diet control and appropriate sports. She had never comply the doctor’s advice. Her disease became uncontrolled. She is now suffering from a severe wound at her right leg and cannot be treated with antibiotics. The only choice to save her life is by performing amputation of her leg. Assignments: 1. What was the cause of Luh Manis’ difficulties to change her habits? 2. How to make the same perception between doctor and patients? 3. How to determine the objectives of the treatment in order to be understood and applied by the patients? 4. What kind of approach should be used to anticipate such a case above? 5. As a family doctor, what should you inform to the patient and her families related to the amputation that must be done? Self Assessments 1. Compare the approaches of caring the acute and chronic diseases! 2. Describe the differences between doctor centered model and patient centered model in treatment program! 3. What information should be told to patients with chronic diseases in order to make them actively involved in their treatment? 4. How to make the same perception of diseases between doctor and patient? 5. How to determine the objectives of the treatment in order to be understood and obeyed by the patients Day 18 & 19 M O D U L E ~ 18 Basic Clinical Skills (Discussion of Student Project) Data/report and discussion guidelines will be provided before the first discussion session Udayana University Faculty of Medicine, DME Page 59 Study Guide Health System-Based Practice 2015 ~ CURRICULUM MAP ~ Smstr Program or curriculum blocks 10 Senior Clerkship 9 Senior Clerkship 8 Senior clerksh ip 7 6 Medical Emergency (3 weeks) Special Topic: -Travel medicine (2 weeks) Elective Study III (6 weeks) Clinic Orientation (Clerkship) (6 weeks) BCS (1 weeks) The Respiratory System and Disorders (4 weeks) The Cardiovascular System and Disorders (4 weeks) The Urinary System and Disorders (3 weeks) The Reproductive System and Disorders (3 weeks) BCS (1 weeks) Alimentary & hepatobiliary systems & disorders (4 Weeks) BCS (1 weeks) The Endocrine System, Metabolism and Disorders (4 weeks) BCS (1 weeks) Clinical Nutrition and Disorders (2 weeks) BCS (1 weeks) Elective Study II (1 weeks) 5 BCS (1 weeks) BCS (1 weeks) BCS (1 weeks) 4 3 2 Musculoskeletal system & connective tissue disorders (4 weeks) Neuroscience and neurological disorders (4 weeks) Behavior Change and disorders (4 weeks) BCS (1 weeks) Hematologic system & disorders & clinical oncology (4 weeks) BCS (1 weeks) Immune system & disorders (2 weeks) BCS(1 weeks) Infection & infectious diseases (5 weeks) BCS (1 weeks) The skin & hearing system & disorders (3 weeks) BCS (1 weeks) Medical Professionalism (2 weeks) BCS(1 weeks) Evidence-based Medical Practice (2 weeks) BCS (1 weeks) Health System-based Practice (3 weeks) BCS(1 weeks) Community-based practice (4 weeks) - BCS (1 weeks) Studium Generale and Humaniora (3 weeks) Medical communication (3 weeks) BCS (1 weeks) The cell as biochemical machinery (3 weeks) Growth & development (4 weeks) BCS (1 weeks) BCS(1 weeks) BCS: (1 weeks) Special Topic : - Palliative medicine -Compleme ntary & Alternative Medicine - Forensic (3 weeks) Elective Study II (1 weeks) Special Topic - Ergonomi - Geriatri (2 weeks) Elective Study I (2 weeks) The Visual system & disorders (2 weeks) 1 Pendidikan Pancasila & Kewarganegaraan (3 weeks) Udayana University Faculty of Medicine, DME Page 60