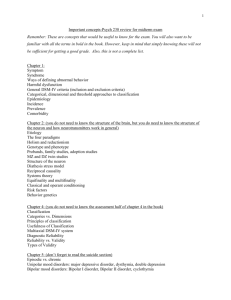
psychological disorders
advertisement

PSYCHOLOGICAL DISORDERS
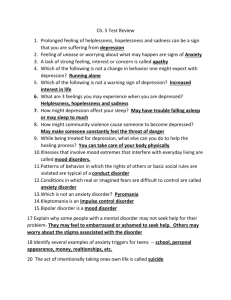
WTD3: Chapter 25
Disease burden by selected illness categories
in established market economies, 1990
Percent
All cardiovascular conditions 18.6
All mental illness**
15.4
All malignant disease (cancer)
15.0
All respiratory conditions
4.8
All alcohol use
4.7
All infectious disease
2.8
All drug use
1.5
2
Prevalence Of Depressive And
Anxiety Disorders
National Comorbidity Survey
Lifetime 40
Prevalence
(%)
30
20
10
0
Major
Depression
Dysthymia
Panic
Disorder
Social
Phobia
Generalized Any Anxiety
Anxiety
Disorder
Disorder
3
FACT SHEETS
26.2 percent of Americans ages 18 and older — about
one in four adults are diagnosed with a mental disorder
annually (57.7 million people )
Only 6% (one in 17) suffer from a serious mental
illness
A leading cause for disability in age group 15-44
45% of people diagnosed have more than 2 mental
disorders diagnosed
Higher in older people (14/100,000)
4
Suicide
eighth leading cause of death for males and
the sixteenth leading cause of death for females in 2004
Suicide by:
Males (%)
Females (%)
Firearms
57
32
Suffocation
23
20
Poisoning
13
38
5
Suicide
Call this toll-free number, available 24 hours a day,
every day: 1-800-273-TALK (8255).
Most suicide attempts are expressions of
extreme
distress, not harmless bids for
attention.
A person who appears suicidal should not be left alone
and needs immediate mentalhealth treatment.
6
Risk factors for Suicide
depression and other mental disorders, or
a substance-abuse disorder (More than 90 percent of people
who die by suicide have
these risk factors.)
prior suicide attempt
family history of suicide
family violence, including physical or sexual
abuse
firearms in the home, (the method used in more
than half
of suicides )
incarceration
exposure to the suicidal behavior of others, such
as family
members, peers, or media figures.
7
?Chemical Basis for suicide
Decreased levels of serotonin have been
found in:
people with depression
impulsive disorders
a history of suicide attempts, and
in the brains of suicide victims
8
? Genetic basis
Two genes are involved
Both genes code for components of the brain’s
glutamate chemical messenger system, involved in the
antidepressant response.
6 percent started to have suicidal thoughts while
taking an antidepressant.
This rate soared to 36 percent among the few
patients with both of the suspect gene versions;
59 percent of the patients who had suicidal
thoughts had at least one of the versions.
9
?Therapy
Cognitive behavioral therapy (useful in
Drug rehab
Clozapine helps in schizophrenics
bipolar)
10
ANXIETY DISORDERS
Generalized Anxiety Disorder
Obsessive-Compulsive Disorder (OCD)
Panic Disorder
Post-Traumatic Stress Disorder (PTSD)
Social Phobia (or Social Anxiety Disorder)
18% (40 MILLION FFECTED PER YEAR)
11
Panic Disorder
“For me, a panic attack is almost a violent
experience. I feel disconnected from reality.
I feel like I’m losing control in a very extreme way.
My heart pounds really hard, I feel like I can’t get my
breath, and there’s an overwhelming feeling that things
are crashing in on me.”
12
Panic Disorder: “Terror Attacks”
a pounding heart, sweatiness, weakness, faintness, or
dizziness
may flush or feel chilled; their hands may tingle or feel
numb; and they may experience nausea, chest pain, or
smothering sensations.
a sense of unreality, a fear of impending doom, or a fear
of losing control.
13
Panic Disorder
6 million American adults affected
Twice as common in women as men
Panic attacks often begin in late
adolescence or early adulthood
?inherited
?Claustrophba/ ?Agarophobia
both can occur
May be associated with other
mental disorders
14
OCD
“I would wash my hair three times as
opposed to once because three was a good
luck number and one wasn’t. It took me
longer to read because I’d count the lines in
a paragraph. When I set my alarm at
night, I had to set it to a number that wouldn’t
add up to a ‘bad’ number.”
15
OCD
Persistent, upsetting thoughts (obsessions)
Patients use rituals (compulsions) to control
the anxiety these thoughts produce.
Most of the time, the rituals end up
controlling them.
16
OCD
2.2 million American adults affected
M:F starts in early childhood-adulthood
?familial
Drugs/ ‘Desensitize’ the behavior
17
Post-Traumatic Stress Disorder (PTSD)
“Then I started having flashbacks. They
kind of came over me like a splash of
water. I would be terrified. Suddenly I
was reliving the event. Every instant was
startling. I wasn’t aware of anything
around me, I was in a bubble, just kind of
floating. And it was scary. Having a
flashback can wring you out.”
7.7 million American adults affected
F>M
18
PTSD features
startle easily,
become emotionally numb (especially in relation to
people with whom they used to be close),
lose interest in things they used to enjoy,
have trouble feeling affectionate,
be irritable,
become more aggressive, or even become
violent.
19
PTSD outcomes
Usually begin within 3 months.
Must last more than a month to be
considered PTSD.
The course of the illness variesRecover within 6 months,
While others have symptoms that last
much longer
Becomes chronic.
20
Social Phobia
(Social Anxiety Disorder)
“When I would walk into a room full of
people,
I’d turn red and it would feel
like everybody’s eyes
were on me. I
was embarrassed to stand off in
a
corner by
myself, but I couldn’t think of
anything to say to anybody. It was humiliating. I felt
so clumsy, I couldn’t wait to get out.”
15 million American adults affected
M:F
Childhood-early adolescence onset
21
SAD
Intense, persistent, and chronic fear of
watched and judged by others
and of
things that will embarrass them.
Blushing, profuse sweating, trembling,
and difficulty talking.
being
doing
nausea,
22
Specific Phobias : 19 million affected F>M
Fear of flying- ‘It was an awful feeling when that
airplane door closed and I felt trapped. My heart
would pound,
and I would sweat bullets. When
the airplane would start to ascend, it just
reinforced the feeling that I couldn’t get out.
When I think about flying, I
picture myself
losing control,
freaking
out, and climbing
the walls, …’
Others-closed-in places, heights,
escalators,
tunnels, highway driving, water, flying, dogs, and
injuries
involving blood.
23
Generalized Anxiety Disorder (GAD)
“I’d have terrible sleeping problems. There were
times I’d wake up wired in the
middle
of the
night. I had trouble concentrating,
even reading the
newspaper or a novel.
Sometimes I’d feel a little
lightheaded. My
heart would race or pound. And that
would make me worry more. I was always
imagining things were worse than they
really
were: when I got a stomachache, I’d
think it was an
ulcer.”
6.8 million affected F>M
24
GAD
Unprovoked exaggerated worry and
Overly concerned about health issues,
family problems, or difficulties at work
Worries excessively about a variety of
problems for at least 6 months
Can’t relax, startle easily, and have
concentrating, have insomnia
tension
money,
everyday
difficulty
25
GAD:
Associated Physical symptoms
fatigue,
headaches,
muscle tension/aches,
difficulty swallowing,
trembling, twitching, irritability, sweating,
nausea, lightheadedness,
having to go to the bathroom frequently,
feeling out of breath, and
hot flashes
26
ANXIETY DISORDERS
Therapy Guidelines
Psychotherapy and / or medications
Identify and treat drug abuse
Treat with- antidepressants, anti-anxiety
and beta-blockers
4 to 6 weeks before symptoms start to fade
drugs,
27
SSRIs
Fluoxetine (Prozac®),
sertraline (Zoloft®),
escitalopram (Lexapro®),
paroxetine (Paxil®), and
citalopram (Celexa®)
for panic disorder, OCD, PTSD, and social
phobia, OCD
venlafaxine (Effexor®), for GAD
28
“serotonin syndrome,”
confusion, hallucinations, increased
sweating, muscle stiffness, seizures,
changes in blood pressure or heart
rhythm
29
Tricyclics:
anxiety disorders other than OCD
cause dizziness, drowsiness, dry mouth,
and
weight gain,
imipramine (Tofranil®), which is
prescribed
for panic disorder and GAD,
and clomipramine
(Anafranil®), which is
the only tricyclic
antidepressant useful for treating OCD.
30
MAO inhibitors
phenelzine (Nardil®),
tranylcypromine (Parnate®), and
isocarboxazid (Marplan®) \
panic disorder and social phobia
Food/Drug/Herb interactions-cannot eat a variety of foods and
beverages (including cheese and red wine) that contain
tyramine* or take certain
medications, including some types of
birth control pills, pain relievers (such as Advil®, Motrin®,
or Tylenol®), cold and allergy medications, and herbal
supplements
* tyramine - is similar to essential amino acid TYROSINE –
required for synthesis of epinephrine
31
High-potency benzodiazepines
Clonazepam (Klonopin®) is used for social
phobia and GAD,
Lorazepam (Ativan®) is helpful for panic
disorder, and
Alprazolam (Xanax®) is useful for both
panic disorder and GAD.
Note!-Some people experience withdrawal
symptoms if they stop
taking benzodiazepines
abruptly instead of tapering
32
Beta-Blockers
Propranalol (Inderal®)
Can prevent the physical symptoms that
accompany certain anxiety
disorders,
particularly social phobia.
33
CBT
Cognitive-behavioral therapy (CBT) is very useful in
treating anxiety disorders.
CBT or behavioral therapy often lasts about 12 weeks.
It may be conducted
individually or with a group of
people
who have similar problems. Group
therapy is particularly effective for
social phobia.
Psychotherapy by trained people
34
CBT
Benefits of CBT last longer than those of
medication for people with panic disorder,
and the same may be true for OCD, PTSD,
and social phobia. If a
disorder recurs at
a later date, the
same therapy can be
used to treat it
successfully a second
time.
35
ADHD:
Attention Deficit Hyperactivity Disorder
Impulsiveness: a child who acts quickly without
thinking first.
Hyperactivity: a child who can't sit still, walks,
runs, or
climbs around when others are seated, talks when others are
talking.
Inattention: a child who daydreams or seems to
be in
another world, is sidetracked by what is going on around him
or her during preschool and early school years
3 -5 percent of children have ADHD, or
approximately
2 million children
36
ADHD
First described in 1845
Remember!All children are sometimes restless,
sometimes act without thinking,
sometimes daydream the time
away.
37
ADHD
DSM-IV-TR classifies predominantly hyperactive-impulsive type
predominantly inattentive type
combined type
38
ADHD- hyperactive-impulsive
Always “on the go” or constantly in
motion.
They dash around touching
or
playing
with whatever is in sight, or
talk incessantly
Squirm and fidget
Wiggle their feet, touch everything, tap
the
pencil
39
ADHD- Impulsive
unable to curb their immediate reactions or think
before they act
‘blurt out’ inappropriate comments
Show emotions without restraint
Can’t wait!
Even as teenagers or adults, they may impulsively
choose to do things that have
an immediate but
small payoff rather than engage in activities that
may take
more effort yet provide much greater
but
delayed
rewards.
40
You are hyperactive –
impulsive-ADHD Feeling restless, often fidgeting with hands or feet,
or squirming while seated
Running, climbing, or leaving a seat in situations
where sitting or quiet behavior is expected
Blurting out answers before hearing the whole
question
Having difficulty waiting in line or taking turns.
41
You are inattentive –-ADHDDifficulty in- focusing deliberate, conscious
attention to organizing and
completing a task or
learning something new.
Homework is particularly hard
If finally finished, is full of errors and erasures
Homework is often accompanied by frustration
for both parent and child.
42
signs of inattention:‘Daydreamers’
Often becoming easily distracted by irrelevant
sights and sounds
Often failing to pay attention to details
and
making careless mistakes
Rarely following instructions carefully and
completely losing or forgetting
things like toys, or
pencils, books, and tools needed for a task
Often skipping from one uncompleted activity to
another.
43
Is it really ADHD?
Because everyone shows some of these
behaviors at times, the diagnosis requires that
such behavior be demonstrated to a degree that is
inappropriate for the person’s age.
Behaviors must appear early in life, before age 7,
and continue for at least 6 months. Above all, the
behaviors must create a real handicap in at least two
areas of a person’s life
44
Who can help?
Specialty
Can
Diagnos
ADHD
Can prescribe Provides
medication,
counseling
if needed
or training
Psychiatrists
yes
yes
yes
Psychologists
yes
yes*
yes
Pediatricians or
Family
Physicians
yes
yes
no
Neurologists
yes
yes
no
Clinical Social
workers
yes
no
yes
45
ADHD ‘like’ disorder caused by-
A sudden change in the child’s life—the death of
a parent
or grandparent; parents’ divorce; a parent’s job loss
Undetected seizures, such as in petit mal or temporal lobe
seizures
A middle ear infection that causes intermittent hearing
problems
Medical disorders that may affect brain functioning
Underachievement caused by learning disability
Anxiety or depression.
46
?Blame ADHD on environment
cigarettes and alcohol during pregnancy
high levels of lead in the bodies of young
preschool children
brain injury
diet restrictions helped about 5 % of children
with ADHD, mostly young children who had food
allergies
47
?Size matters
As a group, the ADHD children showed 3-4
percent smaller brain volumes in all regions—the
frontal lobes, temporal gray matter, caudate
nucleus, and cerebellum.
48
ADHD Associated conditions
20-30% have additional learning disabilitydifficulty in understanding certain sounds or
words and/or difficulty in expressing oneself in
words
reading or spelling disabilities, writing
disorders, and arithmetic disorders may appear
reading disorder, dyslexia, is quite
widespread (8%)
49
ADHD Associated conditions
Tourette Syndrome -nervous tics
and
repetitive mannerisms, such as eye blinks, facial
twitches, or grimacing. Others may clear their
throats frequently, snort, sniff, or bark out words.
Oppositional Defiant Disorder
(ODD)-
boys-defiant, stubborn, non-compliant, have
outbursts of temper, or become belligerent. They
argue with adults and refuse to obey. (30-50%)
50
ADHD Outcome 20-40%-conduct disorder (CD), a more serious pattern of
antisocial behavior conduct disorder:
frequently lie or steal,
fight with or bully others, and are at a real risk of getting into
trouble at school or with the police.
violate the basic rights of other people,
are aggressive toward people and/or animals,
destroy property, break into people’s homes, commit thefts,
carry or use weapons, or engage in vandalism.
These children or teens are at greater risk for substance use
experimentation, and later dependence and abuse.
51
ADHD Associated conditions
Anxiety and Depression
Bipolar Disorder
(difficult to differentiate)
52
ADHD Drug Therapy- Stimulants
Trade Name
Generic Name
Approved Age
Adderall
amphetamine
3 and older
Concerta
methylphenidate (long acting)
6 and older
Cylert*
pemoline
6 and older
Dexedrine
dextroamphetamine
3 and older
Dextrostat
dextroamphetamine
3 and older
Focalin
dexmethylphenidate
6 and older
Metadate ER
methylphenidate (extended release)
6 and older
Metadate CD
methylphenidate (extended release)
6 and older
Ritalin
methylphenidate
6 and older
Ritalin SR
methylphenidate (extended release)
6 and older
Ritalin LA
methylphenidate (long acting)
6 and older
53
ADHD Therapy Drug – non
stimulant
Strattera®, or atomoxetine, works on the
neurotransmitter norepinephrine, whereas the
stimulants primarily work on dopamine
Side effects of Ritalin-The most common side
effects are decreased appetite, insomnia, increased
anxiety, and/or irritability. Some children report
mild stomach aches or headaches.
54
?Duration of medication
About 80 percent of children who need
medication for ADHD still need it as teenagers.
Over 50 percent need medication as adults.
55
AUTISM:
(Pervasive Developmental Disorders)
Severe and pervasive impairment in thinking, feeling, language,
and the ability to relate to others.
SubtypesAutistic disorder,
Pervasive development disorder not otherwise specified (PDD-NOS),
Asperger syndrome
Rett syndrome and childhood disintegrative disorder.
56
Autism
3.4 of every 1,000 children 3-10 years old had autism
only 50 percent of children are diagnosed
before
kindergarten.
demonstrate deficits in
1) social interaction,
2) verbal and nonverbal communication, and
3) repetitive behaviors or interests, unusual responses to sensory
experiences, such as certain sounds or the way objects look
57
Indicators of Autism Disorders:
Does not babble, point, or make meaningful gestures by 1 year of age
Does not speak one word by 16 months
Some kids are late speakers, though. Make sure they don’t have infections, hearing problems, etc.
Does not combine two words by 2 years
Does not respond to name
Loses language or social skills
58
Other Indicators of Autism Disorders:
Poor eye contact
Doesn't seem to know how to play with toys
Excessively lines up toys or other objects
Is attached to one particular toy or object
Doesn't smile
At times seems to be hearing impaired
59
Autism:
By age 3, most children have passed predictable milestones on the
path to learning language;
Can be mute
May simply scream or grab
?genetics: fragile-X syndrome/ tuberous sclerosis
Specifically associated with autism spectrum disorders
60
Autism:
no single best treatment package
early intervention is important; another is that most individuals
with ASD respond well to highly structured, specialized programs
applied behavior analysis
build on the child's interests
offer a predictable schedule
teach tasks as a series of simple steps
actively engage the child's attention in highly structured activities
provide regular reinforcement of behavior.
61
Autism: ?Diet
gluten-free, casein-free diet
? use of secretin- Anecdotal reports have shown
improvement in autism symptoms, including sleep patterns,
eye contact, language skills, and alertness.
62
? Causes Autism
Unknown
Heavy metals not proven/ mercury no longer used in vaccines
That said, shouldn’t give multiple vaccines at once – need to give them gradually.
DPT (whooping cof, diptheria, tetanus) should be given 1st 9 months of life.
18 months, mumps, measles, rubella
Age 5 - Hep A, B
The catch is that daycare can expose kids to all of these before the age of 12 months! Rotavirus,
staph, strep and more can be acquired here as well. That means more antibiotics and resulting
superinfections.
Postmortem and MRI studies have shown that many major brain
structures are implicated in autism. This includes the cerebellum,
cerebral cortex, limbic system, corpus callosum, basal ganglia, and
brain stem.
Abnormal brain development beginning in the infant’s first few
months.
“Growth dysregulation hypothesis”
63
Structures involved in Autism
64
65
Bipolar Disorder: Manic-Depressive
2.6% (5.7million)
“Manic-depression distorts moods and thoughts, incites dreadful
behaviors, destroys the basis of rational thought, and too often
erodes the desire and will to live. One that brings in its wake
almost unendurable suffering and, not infrequently, suicide.”
Mood swings
66
Signs and symptoms of mania
(or a manic episode)
Increased energy, activity, and restlessness
Excessively “high,” overly good, euphoric mood
Extreme irritability
Racing thoughts and talking very fast, jumping from one idea to another
Distractibility, can’t concentrate well
Little sleep needed
Unrealistic beliefs in one’s abilities and powers
Poor judgment
Spending sprees
A lasting period of behavior that is different from usual
Increased sexual drive
Abuse of drugs, particularly cocaine, alcohol, and sleeping medications
Provocative, intrusive, or aggressive behavior
Denial that anything is wrong
67
DSM-IV Criteria for Manic episode
3 or more of the other symptoms most of the day, nearly every day,
for 1 week or longer.
If the mood is irritable, four additional symptoms must be present.
Psychotic symptoms -hallucinations (hearing, seeing, or otherwise
sensing the presence of things not actually there) and delusions
(false, strongly held beliefs not influenced by logical reasoning or
explained by a person’s usual cultural concepts).
68
Signs and symptoms of depression
(or a depressive episode)
Lasting sad, anxious, or empty mood
Feelings of hopelessness or pessimism
Feelings of guilt, worthlessness, or helplessness
Loss of interest or pleasure in activities once enjoyed, including sex
Decreased energy, a feeling of fatigue or of being “slowed down”
Difficulty concentrating, remembering, making decisions
Restlessness or irritability
Sleeping too much, or can’t sleep
Change in appetite and/or unintended weight loss or gain
These are the early signs. Can happen quickly or slowly.
Chronic pain or other persistent bodily symptoms that are not caused by
physical illness or injury
Thoughts of death or suicide, or suicide attempts
69
Criteria for Depressive Episode
A depressive episode is diagnosed if five or more
of these symptoms last most of the day, nearly
every day, for a period of 2 weeks or longer
70
Bipolar: DSM-IV-TR classifiesBipolar 1:recurrent episodes of mania and depression (Classic
type)
Bipolar 2:never develop severe mania but instead experience
milder episodes of hypomania that alternate with depression
Rapid-recycling type: four or more episodes of illness occur
within a 12-month period
71
Outcomes:
Bipolar disorder is a recurrent illness, long-term preventive
treatment is strongly recommended and almost always
indicated
“mood stabilizers” –
This is the best western tx for it – keep the mood swings from occuring.
Lithium
Controls mood swings, but high doses can cause convulsions, coma, death.
Must measure blood levels every couple of months. This is the 2nd choice
now.
Anti-convulsants- valproate (Depakote®) or carbamazepine
(Tegretol®), (valproate may lead to adverse hormone changes
in teenage girls and polycystic ovary syndrome in women who
began taking the medication before age 20)
All drugs here are teratogenic…not for use with preggers.
72
Depression: A Systemic Illness—
The Emotional and Physical Signs
Depressed mood
Anhedonia
Hopelessness
Low self-esteem
Impaired memory
Difficulty concentrating
Anxiety
Preoccupation with negative
thoughts
Headache
Fatigue
Disturbed sleep
Dizziness
Chest pain
Vague joint/limb pain
Vague back/abdominal pain
GI complaints (nausea, vomiting,
constipation, diarrhea, gas)
Sexual dysfunction/apathy
Menstrual problems
73
Types of Depression
Major depressive disorder
More than 12 weeks
Dysthymic disorder
Psychotic depression
Postpartum depression
Can manifest up to 18 months after delivery!
Seasonal affective disorder (SAD)
74
Symptoms of Depression
Persistent sad, anxious or "empty" feelings
Feelings of hopelessness and/or pessimism
Feelings of guilt, worthlessness and/or helplessness
Irritability, restlessness
Loss of interest in activities or hobbies once pleasurable,
including sex
Fatigue and decreased energy
Difficulty concentrating, remembering details and making
decisions
Insomnia, early–morning wakefulness, or excessive sleeping
Overeating, or appetite loss
Thoughts of suicide, suicide attempts
Persistent aches or pains, headaches, cramps or digestive
problems that do not ease even with treatment
75
Co-existing conditions:
Anxiety/ PTSD/ OCD/ Panic Disorder
Alcohol/ Substance abuse
Heart Disease/ Stroke/ Cancer/ HIV/ Diabetes/
Parkinson’s
All above have or can have an element of depression.
76
Etiology?
Genetic/ Biochemical/ Environmental
Functional MRI/PET scans show the depressed brain functioning
differently than a non-depressed brain
Trauma
Head injuries can result in depression
F>M (?Hormone related)
High estrogen for instance
Men present with fatigue, irritability, loss of interest in once–
pleasurable activities, and sleep disturbances
Women present with feelings of sadness, worthlessness and/or
excessive guilt.
77
Childhood depression
Pretend sick/ Refuse to go to school
Sulk/ ‘Trouble’
At age 15 F:M =2:1 – females more likely to get
depressed.
‘Identity’ issues (i.e., gender)
78
Depression Therapy
Highly treatable
Check for medical reasons- thyroid/viral diseases
Psychotherapy / Medication
MedicationSSRIs include fluoxetine (Prozac), citalopram (Celexa), sertraline
(Zoloft)
SNRIs –(Serotonin and norepinephrine)-venlafaxine (Effexor) and
duloxetine (Cymbalta).
Tricyclics and MAOIs
Food/drug interactions, so less commonly used now.
79
Side Effects
SSRIs and SNRIs:
Headache–usually temporary and will subside.
Nausea–temporary and usually short–lived.
Insomnia and nervousness (trouble falling asleep or waking often during the
night)–may occur during the first few weeks but often subside over time or if the
dose is reduced.
Agitation (feeling jittery).
Sexual problems– reduced sex drive, erectile dysfunction, delayed ejaculation,
or inability to have an orgasm.
80
Side Effects
TricyclicsDry mouthConstipationBladder problems–
Sexual problems–
Blurred vision–
Drowsiness during the day–
81
FDA ‘Black Box’ Warning
2007- all antidepressant medications extend the warning to
include young adults up through age 24. A "black box"
warning is the most serious type of warning on prescription
drug labeling.
Possible side effects to look for are worsening depression,
suicidal thinking or behavior, or any unusual changes in
behavior such as sleeplessness, agitation, or withdrawal
from normal social situations.
Black box warning happened after Columbine shootings –
at least one of those kids was on some of these anti-depressants
82
Talk Therapies
Short–term (10 to 20 weeks) / long term
Cognitive Behavioral Therapy - Helps change negative
thinking
IPT (Inter Personal Therapy)-Understand and work through
troubled personal relationships
Both are useful as stand alone therapy for mild to moderate
depressions
83
? ECT- Electro Convulsive Therapy
For severe unresponsive forms of Depression
ECT may cause some short-term side effects,
including confusion, disorientation and memory
loss.
Age old treatment since electricity was invented…shock therapy.
84
Brodmann Areas
Done for severly intractible depressive patients – area 25 is the region where needles are inserted, wired up…
See next page. Experimental – done in Dallas and at Emory at Atlanta.
85
Deep Brain Stimulation for Depression
For about 10 percent of people with
severe depression, when no other
available treatments work
Area in the brain -- called area 25 -- that
plays a critical role in depression.
Deep Brain Stimulation for Treatment-Resistant
DepressionNeuron, Helen Mayberg et. Al, Neuron,
Vol 45, 651-660, 03 March 2005
86
Help Line for depression
Call the doctor.
Call 911 or send to a hospital emergency room to get
immediate help or ask a friend or family member to
help with these things.
Call the toll-free, 24-hour hotline of the National
Suicide Prevention Lifeline at 1-800-273-TALK (1800-273-8255); TTY: 1-800-799-4TTY (4889) to talk
to a trained counselor.
Make sure the suicidal person is not left alone.
87
88
89
90
Depression/Anxiety Disorders Comorbidity*
56% (PD + depression3)
42%
(simple phobia +
depression2)
GAD
Specific
Phobia
PD
PTSD
Depression
62%
48%
(PTSD +
depression4)
SAD
37%
(SAD +
depression2)
(GAD +
depression1)
OCD
27%
(OCD + depression5)
91
Schizophrenia
Positive symptoms are unusual thoughts or perceptions,
including hallucinations, delusions, thought disorder, and
disorders of movement
Negative symptoms represent a loss or a decrease in the
ability to initiate plans, speak, express emotion, or find
pleasure in everyday life.
Men in their late teens and early 20s and in women in their
mid-20s to early 30s
92
Schizophrenia
1% to 1.5%
M=F
?genetic
?>’born in’ winter and spring months
in 2nd trimester)
?Industrialization
?altered brain anatomy
Hypoxia/difficult labor
(viral- flu
93
Schizophrenia chemistry
DA system hyppothesis –’blocking DA receptors
helps the
patients
5-HT receptors blocking
Glutamate and NMDA
(N-methyl- D-aspartate ) receptors hypo function
GABA receptor overactvity
Decreased brain peptides
NE activity decreased
94
Diagnosis
Positive symptoms : actively expressed and
easily observed –
hallucinations, thought disorder, delusions, and
bizarre behavior.
Negative symptoms : decrease in emotional
range, poverty of speech, loss of interests, and loss
of drive
95
Diagnosis
Cognitive symptoms : deficits in attention,
memory, and executive functions
96
Medical Causes of Psychosis
Medical Causes of Psychosis
Temporal lobe epilepsy
Brain tumor, stroke, brain trauma
CNS infections (AIDS, neurosyphilis)
Dementia (Alzheimer's, Lewy's body, vascular)
Wilson's disease
Huntington's disease
Vitamin deficiency (B12)
Endocrine disorders (Cushing's syndrome)
Autoimmune disorders (systemic lupus)
Metabolic disorders (porphyria)
97
Therapy
Hospitalize during acute phase
DA-receptor antagonists (called typical
antipsychotics) –haloperidol and
fluphenazine
5-HT (serotonin)-dopamine antagonists
(called atypical antipsychotics)
98
Atypical
Antipsychotic
Initial
Dose(mg)
Clozapine
25-50
Olanzapine
5-10
Standard Dose
(mg/day)
300-600
15-20
Max
Dose
900
20
Advantages
Disadvantages
Effective in
refractory
schizophrenia
Agranulocytosis
Lowest risk of
extrapyramidal
symptoms (EPS)
No injectable form
Well tolerated
Weight gain
Approved for
acute mania
No liquid form
No liquid form
Weight gain,
seizures
No injectable form
Quetiapine
25-50
400-600
800
Well tolerated
Slow titration
Lowest EPS risk
Sedation
No liquid form
No injectable form
Risperidone
Ziprasidone
1-2
40-80
4-8
80-160
16
160
Well tolerated
Dose-dependent
EPS
Well-defined
dose range
No injectable form
Well tolerated
QT prolongation
No weight gain
Taken with food
Injectable form
Nausea, insomnia
No liquid form
99
OUTCOMES
Favorable short-term outcome –
Continued medication.
Good premorbid adjustment / good health prior to illness
onset.
Being married improves prognosis
Female sex
More acute or more obvious presentation of illness.
Fewer and briefer psychotic episodes.
Less exposure to high levels of overly critical, demanding, or
emotionally over-involved relatives (so-called "high expressed
emotion" factor).
100
Long term outlook
Remissions/ Relapses
49-68% improvement
Illness tends to fade with age
101
DELIRIUM
“Rapid onset of variable and
fluctuating changes in
mental status”
102
Delirium
1. Physiologic consequences of a medical
disturbance
2. Disturbance in consciousness
3. A change in cognition that cannot be better
accounted for by a preexisting or evolving
dementia
103
Delirium
AKA:
acute confusional state
acute brain syndrome
metabolic encephalopathy
toxic psychosis and
acute brain failure
104
Delirum
Higher in older patients
AIDS
CABG
Prescription Drugs
Features- disorientation, concrete thinking, and
inattention
105
Mechanism of Delirium
Excessive neurotransmitter release
Abnormal signal conduction
Overactivity of muscarinic cholinergic neurons in
reticular-activating system, cortex, and hippocampus
Hypoxia leads to increased DA release
the
106
Therapy
Haloperidol {Haldol®}(preferred)
BZs –useful in quick relief
Delirium is associated with significant morbidity and
mortality (30%)
107
Eating Disorders:
Anorexia Nervosa
Refusal to maintain body weight (85% +)
Intense fear of gaining weight or becoming fat, even
though underweight.
Undue influence of body weight or shape on selfvaluation, or denial of the seriousness of the current
low body weight.
In postmenarchal females, amenorrhea ie, the
absence of at least three consecutive
cycles.
108
Anorexia Types
Restricting Type:
Not regularly engaged in
binge- eating or purging
behavior (ie, self-induced
vomiting or the misuse of
laxatives, diuretics,
or enemas)
Binge-Eating/
Purging Type:
Regularly engaged
in binge-eating or
purging behavior
109
Bulimia Nervosa
Recurrent episodes of binge eating
(1) Eating, in a discrete period of time (eg, within any 2-hour
period)
(2) A sense of lack of control over eating during the episode
Recurrent inappropriate compensatory behavior in order to
prevent weight gain
The binge eating and inappropriate compensatory behaviors
both occur, on average, at least twice a week for 3 months.
Self-evaluation is unduly influenced by body shape and weight.
Does not occur exclusively during episodes of anorexia
nervosa.
110
Pathophysiology
Unknown
? Ednorphins- denial of hunger
Decreased 5HT/NE turnover in the body
?genetic (5%)
FH: substance abuse/ alcoholics/ obesity/ mood
disorders
111
Psychosocial Factors
>Hostility
>Chaos
>Isolation
<care and empathy
>Societal pressures
High achievers
Impaired impulse regulation
112
PSYCHIATRIC COMORBIDITY
Major depressive disorder or dysthymia
(50%
to 75%)
Bipolar disorder (4% to 13%)
OCD (25% with AN)
Sexual abuse (20% to 50%)
Substance abuse (12 to 18% with AN especially
binge/purge subtype) and (30% to 37% with BN)
113
Therapy
Rehab / Psychotherapy/ Medication
Hospitalize if:
wt <75% of expected wt.
Electrolytes/ Otrho. Htn/ HR <40/ tachycardia/
hypothermia / suicidal
114
Therapy
Psychosocial Treatments –
dynamic expressive-supportive therapy and
cognitive behavioral techniques
Antidepressants: SSRIs
Rule of 3- 1/3 recover fully/ 1/3 partial/ 1/3 no
response
115
Prognosis
AN: long time follow up- 60 months
Mortality (20%)- cardiac arrest/ suicide
Good factors-admission of hunger, lessening of
denial and improved self- esteem
Bad factors- initial lower minimum weight,
vomiting/laxative abuse, failure to respond to previous
treatment, disturbed family relationships and
parental
conflicts.
116
BN: Prognosis
Short term success- 70%
Relapse rates- 30-50% at 6 months
Better than AN
Poor Factors hospitalization
higher frequency of vomiting
poor social and occupational functioning
poor motivation for recovery
severity of purging and
presence of medical complications,
high levels of impulsivity
longer duration of illness
presence of obesity and substance abuse
117
Alcohol Dependence
10-15% of general population
Cage – cut down, annoyed by others, guilt,
opener
1 – 50% sensitivity
2 – >75%
MOA – varied, mostly GABA agonist
eye
118
Alcohol Dependence
Genetics – 50% Environment – 50%
Father to son 4-5 times
Mother to daughter 4-5 times
+FH – natural “tolerance”
119
Alcohol Levels
Body can metabolize about 1 drink per hour
Eliminates about .015-.02/hour
0.1 – euphoria
0.2 – confusion
0.3 – stupor
0.4 – coma
0.5 - death
120
Alcohol Cont.
50% of all MVA related fatalities
Legal limit 0.08 – 0.10 (or 80 – 100)
12oz beer = 5oz wine = 1.5oz of liquor (80 proof)
2nd highest risk factor for suicide attempts
121
Treatments
Detoxification
Alcoholics Anonymous/12 Step
Residential/PHP
Intensive Outpatient
Half-Way Houses
122
Treatment Cont.
Antabuse – blocks aldehyde dehydrogenase
Naltrexone
Acamprosate
Ondansetron – 5HT3 antagonist
Questionably SSRI’s
123
Clinical Effects of Amphetamines:
CNS:
Increased alertness
longer-lasting than cocaine
decreased fatigue/appetite
Irritability, weakness
“amphetamine psychosis”
Arrhythmias, circulatory collapse
124
Psychotomimetic Drugs
"Faster, faster, until the
thrill of speed overcomes
the fear of death."
Hunter S. Thompson
125
126