Blood flow notes
advertisement

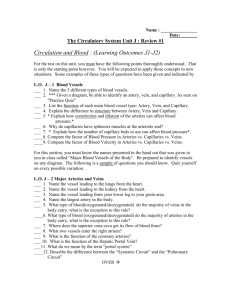
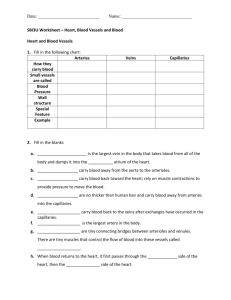
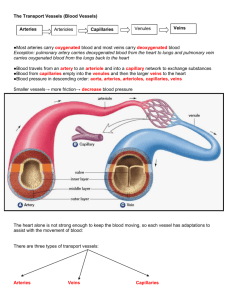
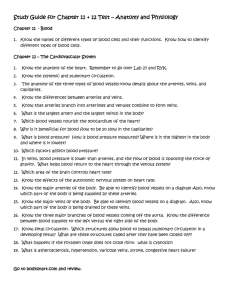
Peripheral Circulation and Regulation 21-1 Peripheral Circulatory System • Systemic vessels – Transport blood through most all body parts from left ventricle and back to right atrium • Pulmonary vessels – Transport blood from right ventricle through lungs and back to left atrium • Blood vessels and heart regulated to ensure blood pressure is high enough for blood flow to meet metabolic needs of tissues 21-2 Blood Vessel Structure • Arteries – Elastic, muscular, arterioles • Capillaries – Blood flows from arterioles to capillaries – Most of exchange between blood and interstitial spaces occurs across the walls – Blood flows from capillaries to venous system • Veins – Venules, small veins, medium or large veins 21-3 Capillaries • Capillary wall consists mostly of endothelial cells • Types classified by diameter/permeability – Continuous • Do not have fenestrae – Fenestrated • Have pores – Sinusoidal • Large diameter with large fenestrae 21-4 Capillary Network • Blood flows from arterioles through metarterioles, then through capillary network • Venules drain network • Smooth muscle in arterioles, metarterioles, precapillary sphincters regulates blood flow 21-5 Structure of Arteries and Veins • Three layers except for capillaries and venules • Tunica intima – Endothelium • Tunica media – Vasoconstriction – Vasodilation • Tunica adventitia – Merges with connective tissue surrounding blood vessels 21-6 Structure of Arteries • Elastic or conducting arteries – Largest diameters, pressure high and fluctuates • Muscular or medium arteries – Smooth muscle allows vessels to regulate blood supply by constricting or dilating • Arterioles – Transport blood from small arteries to capillaries 21-7 Structure of Veins • Venules and small veins – Tubes of endothelium on delicate basement membrane • Medium and large veins • Valves – Allow blood to flow toward heart but not in opposite direction • Atriovenous anastomoses – Allow blood to flow from arterioles to small veins without passing through capillaries 21-8 Blood Vessel Comparison 21-9 Aging of the Arteries • Arteriosclerosis – General term for degeneration changes in arteries making them less elastic • Atherosclerosis – Deposition of plaque on walls 21-10 Pulmonary Circulation • Moves blood to and from the lungs • Pulmonary trunk – Arises from right ventricle • Pulmonary arteries – Branches of pulmonary trunk which project to lungs • Pulmonary veins – Exit each lung and enter left atrium 21-11 Systemic Circulation: Arteries • Aorta – From which all arteries are derived either directly or indirectly – Parts • Ascending, descending, thoracic, abdominal • Coronary arteries – Supply the heart 21-12 Branches of the Aorta 21-13 Systemic Circulation: Veins • Return blood from body to right atrium • Major veins – Coronary sinus (heart) – Superior vena cava (head, neck, thorax, upper limbs) – Inferior vena cava (abdomen, pelvis, lower limbs) • Types of veins – Superficial, deep, sinuses 21-14 Major Veins 21-15 Veins of Thorax 21-16 Hepatic Portal System 21-17 Dynamics of Blood Circulation • Interrelationships between – – – – Pressure Flow Resistance Control mechanisms that regulate blood pressure – Blood flow through vessels 21-18 Laminar and Turbulent Flow • Laminar flow – Streamlined – Outermost layer moving slowest and center moving fastest • Turbulent flow – Interrupted – Rate of flow exceeds critical velocity – Fluid passes a constriction, sharp turn, rough surface 21-19 Blood Pressure • Measure of force exerted by blood against the wall • Blood moves through vessels because of blood pressure • Measured by listening for Korotkoff sounds produced by turbulent flow in arteries as pressure released from blood pressure cuff 21-20 Blood Pressure Measurement 21-21 Blood Flow, Poiseuille’s Law and Viscosity • Poiseuille’s Law • Blood flow – Amount of blood moving through a vessel in a given time period – Directly proportional to pressure differences, inversely proportional to resistance – Flow decreases when resistance increases – Flow resistance decreases when vessel diameter increases • Viscosity – Measure of resistance of liquid to flow – As viscosity increases, pressure required to flow increases 21-22 Critical Closing Pressure, Laplace’s Law and Compliance Critical closing pressure – Pressure at which a blood vessel collapses and blood flow stops Laplace’s Law – Force acting on blood vessel wall is proportional to diameter of the vessel times blood pressure Vascular compliance – Tendency for blood vessel volume to increase as blood pressure increases – More easily the vessel wall stretches, the greater its compliance – Venous system has a large compliance and acts as a blood reservoir 21-23 Physiology of Systemic Circulation • Determined by – Anatomy of circulatory system – Dynamics of blood flow – Regulatory mechanisms that control heart and blood vessels • Blood volume – Most in the veins – Smaller volumes in arteries and capillaries 21-24 Cross-Sectional Area • As diameter of vessels decreases, the total cross-sectional area increases and velocity of blood flow decreases • Much like a stream that flows rapidly through a narrow gorge but flows slowly through a broad plane 21-25 Pressure and Resistance • Blood pressure averages 100 mm Hg in aorta and drops to 0 mm Hg in the right atrium • Greatest drop in pressure occurs in arterioles which regulate blood flow through tissues • No large fluctuations in capillaries and veins 21-26 Pulse Pressure • Difference between systolic and diastolic pressures • Increases when stroke volume increases or vascular compliance decreases • Pulse pressure can be used to take a pulse to determine heart rate and rhythmicity 21-27 Capillary Exchange and Interstitial Fluid Volume Regulation • Blood pressure, capillary permeability, and osmosis affect movement of fluid from capillaries • A net movement of fluid occurs from blood into tissues. Fluid gained by tissues is removed by lymphatic system. 21-28 Fluid Exchange Across Capillary Walls 21-29 Vein Characteristics and Effect of Gravity on Blood Pressure Vein Characteristics • Venous return to heart increases due to increase in blood volume, venous tone, and arteriole dilation Effect of Gravity • In a standing position, hydrostatic pressure caused by gravity increases blood pressure below the heart and decreases pressure above the heart 21-30 Control of Blood Flow by Tissues • Local control – In most tissues, blood flow is proportional to metabolic needs of tissues • Nervous System – Responsible for routing blood flow and maintaining blood pressure • Hormonal Control – Sympathetic action potentials stimulate epinephrine and norepinephrine 21-31 Local Control of Blood Flow by Tissues • Blood flow can increase 7-8 times as a result of vasodilation of metarterioles and precapillary sphincters in response to increased rate of metabolism – Vasodilator substances produced as metabolism increases – Vasomotion is periodic contraction and relaxation of precapillary sphincters 21-32 Nervous Regulation of Blood Vessels 21-33 Short-Term Regulation of Blood Pressure • Baroreceptor reflexes – Change peripheral resistance, heart rate, and stroke volume in response to changes in blood pressure • Chemoreceptor reflexes – Sensory receptors sensitive to oxygen, carbon dioxide, and pH levels of blood • Central nervous system ischemic response – Results from high carbon dioxide or low pH levels in medulla and increases peripheral resistance 21-34 Baroreceptor Reflex Control 21-35 Baroreceptor Effects 21-36 Chemoreceptor Reflex Control 21-37 Effects of pH and Gases 21-38 Long-Term Regulation of Blood Pressure • • • • • Renin-angiotensin-aldosterone mechanism Vasopressin (ADH) mechanism Atrial natriuretic mechanism Fluid shift mechanism Stress-relaxation response 21-39 Renin-Angiotensin-Aldosterone Mechanism 21-40 Vasopressin (ADH) Mechanism 21-41 Long Term Mechanisms • Fluid shift • Atrial natriuretic – Hormone released from cardiac muscle cells when atrial blood pressure increases, simulating an increase in urinary production, causing a decrease in blood volume and blood pressure – Movement of fluid from interstitial spaces into capillaries in response to decrease in blood pressure to maintain blood volume • Stress-relaxation – Adjustment of blood vessel smooth muscle to respond to change in blood volume 21-42 Shock • Inadequate blood flow throughout body • Three stages – Compensated: Blood pressure decreases only a moderate amount and mechanisms able to reestablish normal blood pressure and flow – Progressive: Compensatory mechanisms inadequate and positive feedback cycle develops; cycle proceeds to next stage or medical treatment reestablishes adequate blood flow to tissues – Irreversible: Leads to death, regardless of medical treatment 21-43