Cardiovascular-blood vessels
advertisement

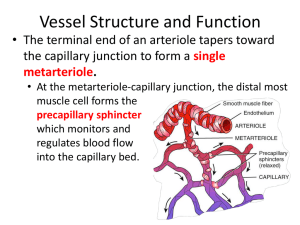
Blood Vessels Intracellular Fluid (ICF): Fluid located within the cell; cytosol Extracellular Fluid (ECF): Fluid outside of body cells; plasma and interstitial fluid Interstitial Fluid (IF): The portion of extracellular fluid that fills the microscopic spaces between the cells of tissues; tissue fluid Bulk Flow Filtration and reabsorption of fluids due to pressure (osmotic/hydrostatic) differences Balance of pressures = net filtration pressure (NFP) Starling's Law of the Capillaries movement of fluid between plasma and the interstitial fluid is in a state of near equilibrium at the arterial and venous ends of a capillary Blood hydrostatic pressure (BHP)= pressure of blood acting against the capillary walls forcing fluids out of capillaries Interstitial fluid hydrostatic pressure (IFHP) = pressure acting outside the capillaries pushing fluid in Blood colloid osmotic pressure (BCOP)= pressure as a result of moving fluid into capillaries due to attraction to non diffusible solutes (i.e. plasma proteins) Edema - filtration exceeds reabsorption resulting in increased interstitial fluid volume; causes include: Increased blood hydrostatic pressure in capillaries (cardiac failure, blood clots) Decreased concentration of plasma proteins (burns, malnutrition, kidney dis.) Increased permeability of capillaries Increased extracellular fluid volume Blockage of lymphatic vessels (radical mastectomy) Edema is not detectable in tissues until IF is increased 30% above normal Blood flows from high pressure (arterial) to low pressure (venous). Arteries-arterioles-capillaries-venules-veins Pressure: aorta: 90-130mmHg arteries: 80-120 arterioles: 60-80 capillaries: 20-40 venules: 10-20 veins: 5-10 vena cava: 0-5 NFP = (BHP+IFOP) - (BCOP+IFHP) Arterial end: NFP=(35+1)-(26+0)=(36)-(26)=10 mmHg Venous end: NFP=(16+1)-(26+0)=(17)-(26)= -9 mmHg Definition of Terms Resistance =the opposition to flow and is a measure of the amount of friction blood encounters as it passes through vessels. Blood viscosity Total blood vessel length Blood vessel diameter . Blood Pressure =the force per unit area exerted on a vessel wall by the blood contained within it (expressed in mm Hg). Arterial blood pressure Systolic pressure Diastolic pressure Pulse pressure Mean arteriole pressure Capillary blood pressure Venous blood pressure Venous Blood Pressure Muscular pump Respiratory pump Factors affecting Blood Pressure Cardiac Output Peripheral Resistance Increased CO = increased BP Decreased CO = decreased BP Increased vasoconstriction = increased BP Increased vasodilation = decreased BP Blood Volume Increased blood volume = increased BP Decreased blood volume = decreased BP Maintaining BP (Short-term: neural) Vasomotor center Baroreceptors Chemoreceptors Hypothalamus and cerebral cortex Peripheral chemoreceptors Maintaining BP (Short-term: chemical) Adrenal medulla hormone (Adrenalin) Atrial natriuretic peptide (ANP) Antidiuretic hormone (ADH) Angiotensin II Nitric oxide Alcohol Endothelin Maintaining BP (Long-term) Renal Regulation High blood pressure due to increased blood volume causes decreased reabsorption in kidneys resulting in a decrease in blood volume and a lowering of blood pressure. Renin-angiotensin II mechanism=when artery blood pressure drops, renin triggers angiotensin II production which causes vasoconstriction and increased blood pressure Blood flow =the volume of blood flowing through a vessel, an organ, or the entire circulation in a given period Blood pressure: Heart pumps blood through vessels. Blood flow is under pressure due to resistance in the system F= P R F= blood flow P= pressure R= resistance Blood flow is directly proportional to changes in blood pressure. Blood flow is inversely proportional to peripheral resistance. Systolic: Ventricles ejecting blood into the aorta Diastole:: ventricles relaxing, pressure drops in aorta Difference between the two is called pulse pressure. What is the pulse pressure on a normal BP of 120/80? 40mm/Hg Pulse pressure is increased in conditions like arteriosclerosis. Total peripheral resistance is controlled by arterioles. BP is controlled by arterioles. Arteries and veins 1- Tunica intima: inside layer of the vessel. in veins= valves 2- Tunica media: smooth muscle is thicker in arteries and thinner in veins. Can dilate and constrict. - vasoconstriction and vasodilation 3- Tunica adventitia: outer layer. Thicker in veins Capillaries: - Extensions of the inner layer of the arteriole: endothelium (simple squamous) - Continuous: skin, muscles and blood brain barrier - Fenestrated: openings called pores that permeable to fluid and small solutes. Found in small intestine (absorption), endocrine glands (hormone release) and kidneys (filtration of blood) - Sinusoids: liver, bone marrow and spleen Very leaky. Capillary Transport Mechanisms Pulse Points Vascular anatomy: Arterial: Major branches off of aorta: Aortic sinus (ascending): right and left coronary artery Arch of aorta: 1- Brachiocephalic trunk which bifurcates into right subclavian a. and the right common carotid a. 2- Left common carotid a. 3- Left subclavian a. Descending aorta: Thoracic aorta lies anterior to the vertebral column and above the diaphragm Branches are: pericardial a. esophageal a. posterior intercostal a. Abdominal aorta lies below the diaphragm. Branches are: celiac a. - left gastric a. - hepatic a. - splenic a. (tortuous) Phrenic a.: diaphragm Superior mesenteric a.: jejunum, ileum, cecum, ascending colon and transverse colon. Inferior mesenteric a.: descending, sigmoid colon and rectum Renal and suprarenal a.: supplies blood to the paired kidneys and adrenal glands Gonadal a.: Male: spermatic a. that descend through the inguinal canal to supply blood to the testes. Female: ovarian a. Middle sacral a.: long slender a. descending anterior to the lumbar vertebra and sacrum to supply blood to sacrum and coccyx. Abdominal aorta will bifurcate into left and right common iliac arteries. - These further divide into: - internal iliac a. - external iliac a. Internal iliac a.: iliolumbar a.: ilium and back muscles superior and inferior gluteal a.: buttocks internal pudendal a.: external genitalia middle rectal a.: rectum External iliac a.: - main blood supply to lower limb - Between the pubis symphysis and the ASIS it becomes the femoral a. Femoral a.: - superficial circumflex iliac a.: groin - deep femoral a.: muscles of thigh and hip joint - deep geniculate a.: distal end of thigh Popliteal a.: knee joint - Will bifurcate into anterior and posterior tibial a. Posterior a. branches into fibular a. (largest branch) Ant. tibial a. becomes dorsalis pedis a. (pedal pulse) Arm, head and neck. Subclavian a.: - vertebral a.: through transverse foramina into brain through foramen magnum. - becomes single basilar a. along the ventral aspect of the brainstem - basilar a. divides into two post. cerebral a. - becomes part of the Circle of Willis at base of brain - thyrocervical a.: thyroid and parathyroid glands pharynx and trachea. Common carotid a.: branch into internal and external carotid a. External carotid a.: - superior thyroid a. - lingual a. - facial a. - occipital a. Internal carotid a.: - Ophthalmic a. - Post. communicating a. (circle of Willis) Terminate in the anterior and middle cerebral arteries. These vessels supply blood to the motor, sensory and speech cortices of the brain. Arm: Subclavian a. give rise to axillary a. - humoral circumflex a. Axillary becomes brachial a. (BP) - deep brachial a. supplies triceps At the elbow the brachial a. divides into ulnar and radial a. (pulse). Major Veins Superior vena cava braciocephalic external/internal jugular vertebral subclavian axillary cephalic brachial basilic median cubital ulnar Radial inferior vena cava splenic hepatic renal superior mesenteric inferior mesenteric common iliac external/internal iliac femoral great saphenous popliteal anterior/posterior tibial fibular dorsal digital Clinical corner Aneurysm - a balloon-like outpocketing of an artery wall that places the artery at risk for rupture Microangiopathic lesion - an abnormal thickening of a capillary basement membrane due to the deposit of glycoproteins Phlebitis - inflammation of a vein accompanied by painful throbbing and redness of the skin Hypotension (low BP) and hypertension (high BP) Angiogenesis - formation of new blood vessels Claudication - pain and lameness or limping caused by defective circulation of the blood in vessels of the limbs (Intermittant) Occlusion - the closure or obstruction of the lumen of a structure such as a blood vessel Hypovolemic shock - large-scale blood loss followed by "thready" pulse White coat hypertension!!!