HSCI319W Midterm Review Session
advertisement

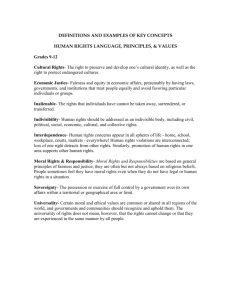
HSCI319W Midterm Review Session By the SFU Health Ethics Club Moral Theories: Deontology (Kantianism) Kant and Ross Duty-based Some behaviours are morally obligatory or prohibited Prima facie duties (take priority over other duties, ex: fidelity, reparation, gratitude, justice, beneficence, self-improvement, nonmaleficence) Beneficence: acts performed for the overall benefit of a patient (doing good) Categorical imperative: a universally binding, unconditional, or absolute moral requirement (ex: do not kill) Autonomy: ability of an individual to govern themselves, formulate and pursue their own goals and values Moral Theories: Utilitarianism Bentham and Mill Principle of utility: belief that we ought to maximize beneficial and minimize harmful consequences for the greatest number of people Cost-benefit analysis Moral agent: rational individual who is capable of understanding the consequences of their actions and is held responsible for the choices they make Nonmaleficence: do no harm Rule utility: (use first) use general rules that benefit all people and acknowledge and protect individual rights Act utility: (use second, if can’t use rule utility) make decisions on a case-by-case basis Justice: duty to give each individual equal consideration based on contextual details of the situation, and to treat similar cases similarly Moral Theories: Biomedical Ethics Four principles: Respect for autonomy Beneficence Nonmaleficence Justice Moral community: group of moral agents who agree to limit their behaviour in order to achieve personal and social benefits (ex: professional code of ethics) Moral Theories: Paternalism, Libertarianism, and Communitarianism Paternalism: the policy of people in power to restrict the freedoms of those dependent on them “for their own good” Libertarianism: focus on personal freedom of choice, autonomy, and concerned about state (government) interference in personal affairs as it may limit freedom Communitarianism: moral decisions are made based on what is best for the group/society Note: can you see any similarities between libertarianism and Kantianism? Or communitarianism and utilitarianism? Scenario: Compulsory Vaccinations? When is it ethically justifiable to mandate a vaccination? What conditions need to be met? Should child benefits only be paid to those who have their children vaccinated (Australia) Should we grant nonmedical exemptions from mandated vaccinations? Pros and cons of limiting this to religious Answer using: Autonomy Beneficence Nonmaleficence Justice Case 1: Refusing Treatment While Incompetent A brilliant physics prodigy named Scott has a history of mental illness and has been hospitalized in psychiatric units on multiple occasions for his erratic behaviour associated with bipolar disorder. Upon his latest hospitalization, doctors recommended treatment including anti-psychotic medications. Scott refused to take the medication even though he knew he was mentally ill and would not be allowed to return home unless he took it. Should Scott be able to determine his own course of treatment even when he may or may not be in a competent mental state? Defend your position using moral theories or principles. Case 2: HIV and Confidentiality Carlos is a 21-year-old HIV+ gay man who is in hospital for a gunshot wound. He is sent home to recover in the care of his older sister, who does not know of his sexual orientation or HIV status. Carlos is very concerned that if his sister knew, she would tell their father and he would be disowned by the family. Would Carlos’s physician be morally justified in breaching patient confidentiality on the grounds that he had a “duty to warn”? Defend your position using moral theories or principles. Case 3: Prenatal Diagnosis and Abortion or Infanticide through Declining Treatment A woman becomes pregnant later in life, putting her child at risk of developing Down syndrome. Her physician offers for her to have a test for the condition done early in the pregnancy so she can decide whether to continue the pregnancy, but she refuses. The baby is born with Down syndrome, and needs life-saving heart surgery in order to survive, but with the surgery could live a long and healthy life. The mother refuses to let the child have the surgery, saying it s no different than had she had the test done in the first trimester and chose to abort then, and it is her decision to make. Is the mother justified in making this claim? Defend your position using moral theories or principles. Case 4: Illegal organ transplant and medical care Bob, a 50-year-old man with diabetes, is on dialysis for chronic renal failure and on the waiting list for a kidney transplant. Because he is in relatively good health, he is low on the list. His physicians advise him that he could be on the list for up to 3 years and that his health during that time would not be jeopardized, aside from the risks and inconveniences associated with long-term dialysis. He does not have family members or friends that are willing to donate a kidney. Unable to find a living donor and dismayed at the thought of remaining on dialysis for years, Bob decided to use his financial resources to purchase a kidney through the black market overseas and undergo a transplant despite of the dangers involved. After returning from his trip, he undergoes septic shock due to an infection from the kidney transplant and is bumped up on the list to receive a kidney and immediate medical care. Should Bob have received care despite his reckless behaviour? Defend your position using moral theories or principles. Case 5: Cultural Health Remedies You are a general practitioner and a mother comes into your office with her child who is complaining of flu-like symptoms. Upon entering the room, you ask the boy to remove his shirt and you notice a pattern of very distinct bruises on the boy's torso. You ask the mother where the bruises came from, and she tells you that they are from a procedure she performed on him known as "cao gio," which is also known as "coining." The procedure involves rubbing warm oils or gels on a person's skin with a coin or other flat metal object. The mother explains that cao gio is used to raise out bad blood, and improve circulation and healing. When you touch the boy's back with your stethoscope, he winces in pain from the bruises. You debate whether or not you should call Child Protective Services and report the mother. Should we completely discount this treatment as useless, or could there be something gained from it? When should a physician step in to stop a cultural practice? (If someone answers "when it harms the child" remind that person that there is some pain in many of our medical procedures, for example, having one's tonsils removed) Should the physician be concerned about alienating the mother and other people of her ethnicity from modern medicine? Do you think that the physician should report the mother?