Anatomy-Joint-Orientation-and
advertisement

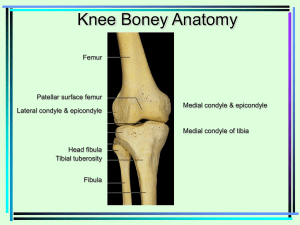
Anatomy, Joint Orientation and Arthrokinematics Knee Tibiofemoral Joint • Femur run in a medial and inferior oblique direction • Sits on a vertical tibia Tibiofemoral Joint • Femoral condyles are convex • Articular surface of medial femoral and tibial condyle larger • Poor congruency between the articulating surfaces Menisci • Fibro cartilaginous disks • Thicker peripherally • Good blood supply outer 1/3 • Rest Avascular Menisci • Roles within the knee – Increase congruency – Distribute weight bearing across the knee – Act as shock absorbers – Aid lubrication reducing friction – Add nutrition to articular cartilage – Aid the locking mechanism of the knee Medial Menisci • • • • Larger than lateral C Shaped Larger posteriorly Anchored to medial capsule and MCL • Anterior horn connects with transverse ligament • Lots of ligamentous and capsular restraints • Limits mobility increasing injury risk Lateral Menisci • More Circular • More Mobile • Medial and lateral meniscus move posteriorly with flexion • Medial and lateral meniscus move anteriorly with extension • If a tear occurs, normal movement is lost, causing locking Ligaments • Coronary Ligament – Part of the joint capsule – Connect meniscu to tibial plateau – Often injured in twisting injuries Ligaments • Transverse Ligament – Connects the anterior horns of the medial and lateral menisci together Ligaments • Meniscofemoral Ligament – Posterior horn of lateral menisci to medial femoral condyle – Anterior and Posterior Divisions Medial Collateral Ligament • Strong flat ligament • Merges with adductor magnus fibres • Deep portion attaches to medial meniscus • Deep portion capsular thickening • Seperated by pes anserinus tendons by bursa • Resists valgus force to the knee and external rotation of the tibia Lateral Collateral Ligament • • • • • Cord like ligament Extracapsular More flexible than MCL Resists varus stress Resists tibial external rotation Anterior Cruciate Ligament • Medial tibia to lateral femoral condyle • 2 bands – Anteromedial • Taut in knee flexion – Posterolateral • Taut in knee extension • Resists anterior translation of tibia on femur and hyperextension of knee Anterior Cruciate Ligament • Secondary restraint of varus/valgus motion • Prevents continued femoral posterior translation during closed chain flexion • Intracapsular but extrasynovial • Blood vessels form a periligamentous sheath around the ligament • Mechanoreceptors found in femoral attachment Posterior Cruciate Ligament • Posterior intercondylar area of tibia to medial condyle of femur • Twice as strong as ACL • 2 Bands – Anterolateral – Posteromedial • Merges with posterior horn of lateral menisci and meniscofemoral ligament Posterior Cruciate Ligament • Restricts posterior translation of tibia on femur and external rotation of tibia • Secondary restraint of varus/valgus motion • Intracapsular, but extrasynovial Posterior Ligaments • Oblique Popliteal Ligament – Thickening of posterior capsule – Expansion of semimembranosus tendon – Passes superior and laterally to femoral intercondylar line • Arcuate Popliteal Ligament – Inferior lateral aspect of posterior capsule – From fibula head to posterior tibial and lateral femoral condyle Joint Capsule • Thick ligamentous sheath composed mainly of muscle tendons and their expansions • Deficient anteriorly due to patella Bursae Infrapatella Fat Pad • Sits between the joint capsule and synovial membrane • Between Patella Ligament and knee joint • Can be impinged or damaged in trauma Arthrokinematics Knee Extension • Open Chain – Tibia Glides Anteriorly and Rolls Anteriorly – Tibia external rotation from 20° Flexion to Full Extension • Closed Chain – Femur Glides Posteriorly and Rolls Anteriorly – Femur Internally rotates on stable Tibia from 20° Flexion to Full Extension Knee Flexion • Open Chain – Tibia Glides Posteriorly and Rolls Posteriorly – Tibia internal rotation from Full Extension to 20° Flexion • Closed Chain – Femur Glides Anteriorly and Rolls Posteriorly – Femur Externally rotates on stable Tibia from Full Extension to 20° Flexion Arthrokinematics Extension Flexion Patellofemoral Joint • Anterior surface of the femoral condyles • Posterior surface of the patella • Divided into medial and lateral facets • 4-5 mm of articular hyaline cartilage on patella Ligamentum Patellae (Patellar Tendon) • Continuation of quadriceps tendon • Attaches into the tibial tuberosity Meniscopatellar Fibres • Fibrous bands running from patella to lateral aspect of medical and lateral menisci Retinaculum • Medial and Lateral • Expansions of different connective tissue • Patellofemoral and patellotibial ligaments • Vastus Medialis, Vastus Lateralis, ITB Patellofemoral Joint Arthrokinematics • Articulation – Inferior margin of patella articulates with the femur at approx 10-20° of knee flexion – As knee flexion increases the contact area of the patella moves proximally – As knee flexion increase the contact area of the condyles moves posteriorly – Patella does not articular with trochlea of femur near terminal extension Patellofemoral Articulations Patellofemoral Articulations Patellofemoral Contact Area • The larger the contact surface area the more a load can be distributed over a greater area • E.g which is more painful, a women standing on you in stilettoes or walking boots? • The contact surface of the patellofemoral joint INCREASES with flexion • @ 30° knee flexion the contact area = 2.0cm² • @ 90 ° knee flexion the contact area = 6.0cm²