Introduction
advertisement
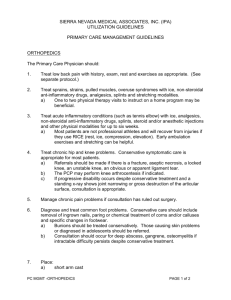
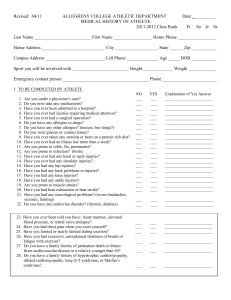
ACE Personal Trainer Manual, 4th edition Chapter 15: Common Musculoskeletal Injuries and Implications for Exercise 1 Introduction When there is an injury to the human body, a variety of structures can be damaged, including: – Bone – Cartilage – Ligaments – Muscle – Skin – Nerves – Blood vessels – Viscera Having a basic understanding of common musculoskeletal injuries helps a personal trainer provide safe and effective exercise programming and make appropriate referrals. Muscle Strains Ligament Sprains Ligament sprains often occur with trauma. Of particular medical significance are injuries to the: – Anterior cruciate ligament (ACL) – Medial collateral ligament (MCL) The mechanism of an ACL injury often involves deceleration of the body, combined with a maneuver of twisting, pivoting, or sidestepping. Grading System for Ligament Sprains Overuse Conditions When the body is put through excessive demands during activity, it often results in overuse conditions such as: – Tendinitis – Bursitis – Fasciitis Knee Cartilage Damage Damage to the joint surface of the knee often involves damage to both the: – Hyaline cartilage – Menisci cartilage The most commonly reported knee injury is damage to the menisci. The cartilage under the patella can also become damaged, resulting in chondromalacia (degeneration of the cartilage of the knee). Bone Fractures The causes of bone fractures are classified as either low or high impact. – Low-impact trauma can result in a minor fracture or a stress fracture. – High-impact trauma injuries are often disabling and require immediate medical attention. Other medical conditions such as infection, cancer, or osteoporosis can weaken bone and increase the risks for fracture. Tissue Reaction to Healing When an injury occurs, the body goes through a systematic process with three distinct phases. Inflammatory phase – Can last for up to six days – The focus is to immobilize the injured area and begin the healing process. Fibroblastic/proliferation phase – Begins approximately at day 3 and lasts approximately until day 21 – Starts with the wound filling with collagen and other cells, which eventually forms a scar – Wound strength continues to build for several months Maturation/remodeling phase – Begins approximately at day 21, and can last up to two years – Remodeling of the scar, rebuilding of bone, and/or restrengthening of tissue into a more organized structure Signs and Symptoms of Inflammation The goal when training post-injury, post-rehabilitation, or post-surgery clients who have medical clearance to exercise is to give them a challenging exercise program that will not cause further damage. The signs and symptoms of tissue inflammation are: – Pain – Redness – Swelling – Warmth – Loss of function Managing Pre-existing Injuries It is important for a trainer to answer the most important question: – “Is the client appropriate for exercise or should he or she be cleared by a medical professional?” – With local injuries, the client should be able to exercise using the non-injured parts of the body. The program must be modified if symptoms of post-injury/postsurgery overtraining occur: – Soreness that lasts for more than 24 hours – Pain when sleeping or increased pain when sleeping – Soreness or pain that occurs earlier or is increased from the prior session – Increased stiffness or decreased ROM over several sessions – Swelling, redness, or warmth in healing tissue – Progressive weakness over several sessions – Decreased functional usage Acute Injury Management If an acute injury occurs, early intervention often includes medical management. The acronym P.R.I.C.E. describes a safe earlyintervention strategy for an acute injury. – Protection – Rest or restricted activity – Ice – Compression – Elevation Flexibility and Musculoskeletal Injuries When a muscle becomes shortened and inflexible, it cannot lengthen appropriately or generate adequate force. Relative contraindications for stretching to prevent injury: – Pain in the affected area – Restrictions from the client’s doctor – Prolonged immobilization of muscles and connective tissue – Joint swelling (effusion) from trauma or disease – Presence of osteoporosis or rheumatoid arthritis – A history of prolonged corticosteroid use Absolute contraindications for stretching: – A fracture site that is healing – Acute soft-tissue injury – Post-surgical conditions – Joint hypermobility (loose joint) – An area of infection Shoulder Strain/Sprain Shoulder strain/sprain occurs when the soft-tissue structures get abnormally stretched or compressed. Signs and symptoms – Local pain at the shoulder that radiates down the arm Medical management Contraindicated movements: – Overhead and across-the-body movements – Any movements that involve placing the hand behind the back Exercise Programming Following Shoulder Strain/Sprain Rehabilitation Focus on improving posture and body positioning. The exercise program should emphasize regaining strength and flexibility of the shoulder complex. Focus on stretching the major muscle groups around the shoulder to restore proper length. Overhead activities often need to be modified. Rotator Cuff Injuries Common among individuals who engage in activities that involve reaching the arms overhead repeatedly, as well as among middle-aged individuals Rotator cuff injury can be classified into two main categories. – Acute – Chronic Signs and symptoms – Acute tears result in a sudden “tearing” sensation followed by immediate pain and loss of motion. – Chronic tears show a gradual worsening, with increased pain at night or after increased activity. Medical management – The client is typically restricted from performing overhead activities and lifting heavy objects. – If there is no progress with physical therapy or the tear is too severe, surgery is indicated to repair the torn muscle. Exercise Programming Following Rehabilitation for Rotator Cuff Injuries The personal trainer must obtain specific exercise guidelines from the physical therapist/surgeon. Focus on improving posture and body positioning. The goal is to continue what has been done in physical therapy in a safe, progressive manner. Performing overhead activities or keeping the arm straight during exercise should be limited. Exercises with the elbows bent will create less torque on the healing muscles. Elbow Tendinitis Tendinitis of both the flexor and extensor muscle tendons of the elbow and wrist can occur with overuse. Lateral epicondylitis – Medial epicondylitis – Repetitive-trauma injury of the wrist flexor muscle tendons near their origin on the medial epicondyle Signs and symptoms – Repetitive-trauma injury of the wrist extensor muscle tendons near their origin on the lateral epicondyle Nagging elbow pain at the lateral or medial epicondyle Medical management – Conservative management for musculoskeletal injuries Exercise Programming Following Elbow Tendinitis Rehabilitation Focus on improving posture and body positioning. Regain strength and flexibility of the flexor/pronator and extensor/supinator muscle groups. Avoid high-repetition activity at the elbow and wrist. Full elbow extension when performing shoulder raises should be done with caution. Carpal Tunnel Syndrome Carpal tunnel syndrome is the result of repetitive wrist and finger flexion leading to a narrowing of the carpal tunnel due to inflammation. Signs and symptoms – Night or early-morning pain or burning – Loss of grip strength and dropping of objects – Numbness or tingling in the palm, thumb, index, and middle fingers – Long-standing effects may include atrophy of the thumb side of the hand, loss of sensations, and paresthesias (numbness). Medical management – Conservative management for musculoskeletal injuries, with the exception of cortisone injections to treat inflammation – May be prescribed wrist splints to wear during activity Exercise Programming Following Carpal Tunnel Syndrome Rehabilitation Focus on improving posture and body positioning. Emphasize regaining strength and flexibility of the elbow, wrist, and finger flexors and extensors. Avoid movements that involve full wrist flexion or extension. Low-back Pain Causes of low-back pain are commonly categorized into: – Mechanical problems – Degenerative disc disease (DDD) and sciatica Exercise precautions – Avoid repeated bending and twisting of the spine – Clients should learn how to stabilize the trunk with a moderate lordosis or “neutral” position and also use back support during overhead activities. Greater Trochanteric Bursitis Greater trochanteric bursitis is characterized by inflammation of the greater trochanteric bursa. – May be due to an acute incident or repetitive (cumulative) trauma – More common in female runners, cross-country skiers, and ballet dancers Signs and symptoms – Trochanteric pain and/or parasthesias – Symptoms are most often related to an increase in activity or repetitive overuse. – The client may walk with a limp Medical management – Conservative management for musculoskeletal injuries – Clients should use an assistive device such as a cane as needed. Exercise Programming Following Rehabilitation for Greater Trochanteric Bursitis The program should focus on regaining flexibility and strength at the hip and include proper posture awareness. Stretching focus: – Iliotibial band complex – Hamstrings – Quadriceps Strengthening focus: – Gluteals – Deep rotators of the hip Proper gait mechanics in walking and running should be a priority. Aquatic exercise is well-tolerated. Contraindicated movements: – Side-lying positions that compress the lateral hip – Higher-loading activity such as squats or lunges Iliotibial Band Syndrome Iliotibial band syndrome (ITBS) is a repetitive overuse condition. – Occurs when the distal portion of the iliotibial band rubs against the lateral femoral epicondyle Primarily caused by training errors. Signs and symptoms – Radiating or sharp “stabbing” pain at the lower lateral knee – Aggravating factors may include any repetitive activity Medical management – Conservative management for musculoskeletal injuries – Clients should use an assistive device such as a cane as needed. Exercise Programming Following ITBS Rehabilitation Focus on improving posture and body positioning. The exercise program should focus on regaining flexibility and strength at the hip and lateral thigh. Aquatic exercise is well-tolerated. Contraindicated movements: – Higher-loading activities such as lunges or squats Lunges and squats limited to 45 degrees of knee flexion can be introduced with a progression to 90 degrees and beyond, if tolerated. Patellofemoral Pain Syndrome Patellofemoral pain syndrome (PFPS) is often called “anterior knee pain” or “runner’s knee.” The cause of PFPS can be classified into three primary categories: – Overuse – Biomechanical – Muscle dysfunction Signs and symptoms – Pain with running, ascending or descending stairs, squatting, or prolonged sitting – A gradual “achy” pain that occurs behind or underneath the patella – Knee stiffness, giving way, clicking, or a popping sensation during movement Medical Management of PFPS Avoid aggravating activities: – Prolonged sitting – Deep squats – Running (particularly downhill running) Modify training variables Proper footwear Physical therapy Patellar taping Knee bracing Foot orthotics Client education Oral anti-inflammatory medication Modalities Exercise Programming Following PFPS Rehabilitation Restoring proper flexibility and strength is the key with PFPS. Stretching – IT band complex – Hamstrings – Calves Exercise should focus on restoring proper strength throughout the hip, knee, and ankle with closed-chain movements. Open-chain knee activity such as leg extensions should be done with caution. http://www.youtube.com/watch?v=9AZHU_WEypI Infrapatellar Tendinitis Infrapatellar tendinitis, or “jumper’s knee,” is an overuse syndrome characterized by inflammation of the distal patellar tendon. Potential causes include: – Improper training methods – Sudden change in training surface – Lower-extremity inflexibility – Muscle imbalance Signs and symptoms – Pain at the distal kneecap – Pain has also been reported with running, walking stairs, squatting, or prolonged sitting. Medical Management of Infrapatellar Tendinitis Avoid aggravating activities: – Plyometrics – Prolonged sitting – Deep squats – Running Modify training variables Proper footwear Physical therapy Patellar taping Knee bracing Arch supports Foot orthotics Client education Oral anti-inflammatory medication Modalities Exercise Programming Following Rehabilitation for Infrapatellar Tendinitis The program focus is to restore proper flexibility and strength in the lower extremity. Stretching – Quadriceps – Iliotibial band – Hamstrings – Calves Exercise should focus on restoring strength throughout the hip, knee, and ankle. High-impact activities such as running or plyometrics are contraindicated. Shin Splints Shin splints are typically classified as one of two specific conditions: – Medial tibial stress syndrome (MTSS), also called posterior shin splints – Anterior shin splints Signs and symptoms – MTSS sufferers complain of a “dull ache” along the distal posterior medial tibia. – Anterior shin splint sufferers complain of the same type of pain along the distal anterior shin. Medical management – Modifying training with lower-impact/lower-mileage conditioning and cross-training – However, the best intervention may just be to rest. Exercise Programming Following Rehabilitation for Shin Splints Cross-training to maintain adequate levels of fitness is indicated in the early stages. Stretching – Pain-free stretching of the calf muscles, especially the soleus, for MTSS – Stretching of the anterior compartment for anterior shin splints Rest and modified activity are the primary interventions for symptom relief. These clients may be sensitive to a rapid return to activity or an extreme change in surfaces. Ankle Sprains Lateral, or inversion, ankle sprains are the most common type. Medial, or eversion, ankle sprains are relatively rare. Signs and symptoms – With lateral ankle sprains, the individual can often recall hearing a “pop” or “tearing” sound and experiences swelling over the lateral ankle. – With medial sprains, there may be medial swelling with tenderness over the deltoid ligament. Medical management – Immobilization and physical therapy Exercise Programming Following Rehabilitation for Ankle Sprains The client can return to exercise for non-injured regions, such as the upper body. Restoring proper proprioception, flexibility, and strength is the key. Stretching and strengthening of the lower limb is indicated, along with training for balance. Targeting the peroneal muscle group for inversion ankle sprains is important for prevention of re-injury. Progress clients first with straight-plane motions, then side-to-side motions, and then multidirectional motions. Achilles Tendinitis Achilles tendinitis can eventually lead to a partial tear or rupture of the Achilles tendon if not addressed appropriately. A multifactorial condition that includes a combination of intrinsic and extrinsic factors. Signs and symptoms – Pain that is 2 to 6 cm (0.8 to 2.3 inches) above the tendon insertion into the calcaneus – Initial morning pain that is “sharp” or “burning” and increases with more vigorous activity Medical management – Controlling pain and inflammation with modalities and anti-inflammatory medication – Proper training techniques – Losing weight – Proper footwear – Orthotics – Strengthening and stretching Exercise Programming Following Rehabilitation for Achilles Tendinitis Controlled eccentric strengthening of the calf complex Restore proper length to the calf muscles. – However, overstretching of the Achilles tendon can cause irritation. – When stretching the calf in a standing position, the client should wear supportive shoes. – The client should be taught to properly position the back foot to point straight ahead. Plantar Fasciitis Plantar fasciitis is an inflammatory condition of the plantar aponeurosis. – Intrinsic factors: • Pes planus (e.g., flat feet) • Pes cavus (e.g., high arch) – Extrinsic factors: • Overtraining • Improper footwear • Obesity • Unyielding surfaces Signs and symptoms – Pain on the plantar, medial heel at its calcaneal attachment – Excessive pain during the first few steps in the morning Management and Exercise Programming Following Rehabilitation for Plantar Fasciitis Conservative management of this condition may include: – Modalities (i.e., treatment) – Oral anti-inflammatory medication – Heel pad or plantar arch – Stretching – Strengthening exercises A doctor may prescribe physical therapy, a night splint, or orthotics, or inject the area with cortisone. The goal is to design a program that challenges the client but does not excessively load the foot. – Stretch the gastrocnemius, soleus, and plantar fascia. – Strengthen the foot’s intrinsic muscles and the calf complex. Summary The key when working with injured or post-injury clients is avoiding exercises that aggravate pre-existing conditions. This session covered: – Types of tissue and common tissue injuries – Tissue reaction to healing – Managing musculoskeletal injuries – Flexibility and musculoskeletal injuries – Upper-extremity injuries – Low-back pain – Lower-extremity injuries – Record keeping