Blood Pressure
advertisement

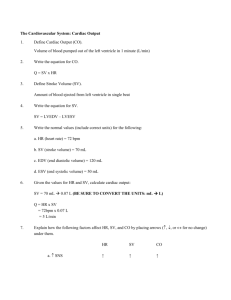
ivyanatomy.com Blood Pressure section 5, chapter 15 CATALYST #3 1) Define systole and diastole 1) Define cardiac cycle 1) What fibers and nodes are a part of the cardiac conduction system? (starts on pg. 332) 1) What is an ECG? Blood Pressure •Blood pressure is the force the blood exerts against the inner walls of the blood vessels •Usually refers to pressure in systemic arteries Arterial blood pressure: •Rises with ventricular contractions and falls as ventricles relax •Systolic pressure is the maximum pressure during ventricular contraction •Diastolic pressure is the minimum pressure when the ventricles relax Factors that influence blood pressure 1. Cardiac Output- volume of blood ejected from one ventricle per minute • Product of heart rate and stroke volume Stroke Volume • Volume of blood expelled from ventricle with each contraction • Average = 70 milliliters per beat (mL/beat) for adult male Heart Rate • Average = 72 beats per minute Example: 70 mL/beat Stroke Volume 70 beats/minute X Heart Rate 5040mL/minute = Cardiac Output Factors that influence blood pressure Cardiac output (and blood pressure) increases with an increase in stroke volume or heart rate. Factors that influence blood pressure 2. Blood Volume • Average blood volume in adults = 5 Liters (1.3 gallons) • As blood volume increases, blood pressure initially increases 3. Peripheral Resistance • Peripheral resistance = friction between blood and blood vessels • Vasoconstriction increases resistance and increases blood pressure • Vasodilation decreases blood pressure 4. Viscosity of blood • Viscosity = resistance of a fluid to flow (thickness of a fluid). • Blood cells and some plasma proteins increase the viscosity of blood. • Anemia (deficiency of red blood cells) reduces viscosity & lowers blood pressure Factors that influence blood pressure Figure 15.24. Some of the factors that influence arterial blood pressure Control of blood pressure A combination of factors control blood pressure. These include stroke volume, heart rate, and peripheral resistance: Figure 15.36 Controlling cardiac output and peripheral resistance regulates blood pressure Control of blood pressure Factors that affect stroke volume •End-diastolic volume (EDV) •Volume of blood in ventricles at the end of ventricular diastole •Ventricles are filled with blood •End-systolic volume (ESV) •Volume of blood in ventricles at the end of ventricular systole •Only 60% of blood is expelled from heart during a normal contraction •Increasing the force of ventricular contractions decreases ESV •Stroke volume = EDV– ESV •Increase stroke volume by increasing EDV or decreasing ESV stroke volume Stroke Volume is directly related to the force of ventricular contraction. Two events that occur in the ventricles coincide with stroke volume: 1. End-diastolic volume (EDV) Volume of blood in ventricles at the end of ventricular diastole As ventricles fill with blood, muscle fibers are mechanically stretched - preload 2. End-systolic volume (ESV) Volume of blood in ventricles at the end of ventricular systole A normal health heart expels 60% of blood present in ventricle. stroke volume Stroke Volume is the difference between end diastolic volume (EDV) and end systolic volume (ESV): Stroke Volume = EDV - ESV Frank-Starling Principle: • The ability of a heart muscle to generate force depends on the original stretch of a muscle prior to contraction (similar to stretching a rubber band) • The degree of stretch (preload) of the myocardial fibers before contraction determines the stroke volume • A greater end diastolic volume results in a greater force of contraction, leading to a greater stroke volume. Venous Return •Blood pressure rapidly decreases as the blood moves through the arterial system and into the capillary network. •Little pressure remains in the veins, therefore heart actions contribute very little to venous return. Figure 15H Blood pressure decreases as blood moves away from the heart. Venous Return •Venous return depends on: •Skeletal muscle contractions – massaging actions push blood towards heart •Respiratory movements – generates pressure in abdominal and thoracic cavities •Changes in pressure pushes blood along veins •Vasoconstriction – contraction of smooth muscles in tunica media •Sympathetic reflexes vasoconstrict the smooth muscles in veins, which can propel additional blood from venous reservoir towards the heart. Systemic Arteries Aorta - Main trunk of the systemic circulation. Divisions of the aorta •Aortic root = attachment to heart •Ascending Aorta •Aortic arch •Thoracic aorta •Abdominal aorta Structures at the root of the aorta 1. Aortic Valve 2. Aortic Sinus • Swelling at aortic root 3. Right and left coronary arteries • Supply blood to myocardium of the heart • Myocardial infarction = blocked coronary artery 3. Aortic Bodies • Chemoreceptors - monitor CO2 & O2 levels in blood arteries of the aortic arch 1. Brachiocephalic Artery Brachiocephalic artery divides into: • Right common carotid artery -Supplies blood to right side of face and head • Right subclavian artery - Supplies blood to right arm 2. Left common carotid artery – supplies blood to left side of face and head 3. Left subclavian artery – supplies blood to left arm Figure 15.42 The major branches of the aortic arch are highlighted in yellow. end of section 5, chapter 15