Porcine Reproductive and Respiratory Syndrome Virus (PRRSV)
advertisement

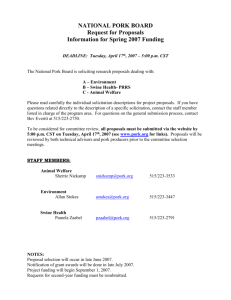
Models of infection: Porcine Reproductive and Respiratory Syndrome Virus (PRRSV) Dr. Amelia Woolums LAMS 5160 PRRSV • Family Arteriviridae – ss (+) RNA, enveloped – genome encodes 7 proteins • Clinical syndrome recognized in North Carolina in mid 1980’s • Virus isolated in Europe in 1991 – Isolated in N. America shortly thereafter PRRSV • Already significant genetic variability when European and NA types identified – Mathematical modeling suggests virus first appeared ~ 1980 • Jumped from another species? • Other family members: – equine arteritis virus (EAV) – LDH-elevating virus (LDV) • possible source of PRRSV?? PRRSV, clinical signs • Reproductive problems – late gestation most common • litters with normal, weak, stillborn, and mummies • anorexia, agalactia in sows – early gestation losses possible: abortions, return to service • Respiratory disease – Dyspnea and tachypnea, ill-thrift, poor growth – Interstitial pneumonia – Most common in grower/feeder – Rarely, severe fatal disease in in adults PRRSV, clinical signs • Cutaneous signs possible – Hyperemia or cyanosis of extremities • Neuro signs in sows rarely • Repro, respiratory, and cutaneous signs very similar to EAV in horses http://www.elsenburg.com/vets/prrs http://www.elsenburg.com/vets/prrs Courtesy Dr. D. Reeves • NOTE that inapparent infection is not unusual • Infection can be prolonged (“persistent”) – As long as 5 months post infection – Shedding is intermittent • Important contribution to epizootiology Pathogenic mechanisms • Virus targets macrophages – Alveolar macrophages, tissue macrophages – Primary sites in acute disease • Lung • Lymphoid tissue: lymphadenopathy common • Many other sites possible: kidney, spleen, heart, thymus, skin, reproductive tract, nervous system – In chronic phase, virus found in peripheral lymph nodes, TONSILS Consider: how could preferential targeting of macrophages contribute to disease? • Decreased (or increased?) production of proinflammatory cytokines (TNF-a, IL-1) • Decreased APC activity: decreased activation of CD4 TH cells • Decreased clearance of virus and cell debris PRRSV, effects on macrophages • Direct killing of macrophages • Decreased production of TNF-a – as compared to influenza, other viruses • Decreased phagocytosis • Induction of apoptosis of “bystanders” – Possibly related to dysfunctional cytokine or costimulatory molecule expression by MP? Effects on immune response • Humoral: – Rapid onset of non-neutralizing antibody – Neutralizing response surprisingly slow (3-4 wks) – Some in vitro evidence for antibody-enhanced disease • How could antibody enhance disease? Effects on immune response • Cell-mediated: – T cell responses following vaccination or infection are slow and weak – IFN-a production actively suppressed • Cells exposed to PRRSV then TGE virus (strong IFN-a inducer): no IFN-a – Why does IFN-a matter? From Janeway, 1999 IFN-gamma Cytotoxic T cell IL-2 MHC II presentation + IL-12 IFN-a T Helper 1 Macrophage IFN-a IL-12 IFN-gamma IFN-a Virus-infected host cell Natural killer cell A. Woolums, LAMS 5160 Effects on immune response • PRRSV suppresses TH1 response – Decreased IFN-a – Decreased TNF-a – Increased IL-10 • Suppresses TH1 response • Net effect: poor response to intracellular pathogen PRRSV, outcome of infection • Outcome of PRRSV infection in a herd of pigs is unpredictable “Why some infected herds apparently suffer no ill effects while others are constantly battling clinical PRRS is not known” Zimmerman, 2003 • Three factors have important impact on outcome of PRRSV infection: – Strain of infecting virus – Host factors – Management factors Disease severity: influence of virus • Genetic variability: major influence on pathogenesis – Two major types: European and North American – Only 60% concordance at genetic level • Innumerable subtypes with varying degrees of relatedness • Immunity to heterologous strains is incomplete to nonexistent Influence of viral genetic variability • PRRSV exists as quasispecies – Genetic variation occurs between farms, among pigs, and WITHIN individual pigs • Farm level diversity (nucleotide): 93% • Among pigs: 4% • Within a given pig: 3% – No two pigs on the same farm had identical PRRSV – Multiple variants coexist in individual animals (Goldberg et al, 2003) Influence of viral genetic variability • PRRSV mutates at an unusually rapid rate, even for an RNA virus – 10-2/amino acid site/year, as compared to 10-3 to 10-5 for HIV, hepatitis C virus – Data suggests this is due to more rapid replication, rather than higher error rate, than other RNA viruses (Hanada et al, 2005) How does the rapid generation of genetic variants contribute to the disease caused by PRRSV? • Frequent opportunity for virus to evade host immune response – New variants could lead to disease in susceptible subgroups within a supposedly resistant herd – Theoretically, persistent virus could “outstrip” host immunity and lead to recurrent disease in previously infected individual – Very difficult to come up vaccines effective in every situation • Viral strain impacts virulence • Genetic variability could allow opportunity for improved virulence: how? – Change in receptor: better attachment/invasion? – Change in proteins that impair host immunity? – Change in proteins that promote inter-pig transmission? • At this time, almost nothing is known about how viral proteins relate to virulence Disease severity: influence of host • Many anecdotal reports of variation in disease severity among different breeds, families • Research supports differential susceptibility among purebreds and commercial lines • Factors that contribute to breed-related susceptibility not known Disease severity: influence of host • Coinfection with other agents makes disease due to PRRSV worse – Influenza, porcine circovirus-2, TGE, Mycoplasma hyopneumoniae, Strep. suis –among others—lead to enhanced PRRSV – Does PRRSV-induced immunosuppression enhance secondary disease? Data mixed • Likely important in at least some cases – PRRSV + M. hyopneumoniae: currently considered leading cause of respiratory disease in growing/finishing pigs Disease severity: influence of management • Clear farm effect on PRRSV severity – More research needed to determine relevant factors – SIZE of farm consistently associated with PRRSV problems • Larger farms more likely to have disease, persistent/recurrent infection • Smaller farms: less problems, even if no efforts made to prevent disease Disease severity: influence of management • Although some farms can have inapparent infection, overall, PRRSV is associated with decreased productivity • Choice for management: try to eradicate, or live with it? Disease severity: influence of management • Problem: strategies that have worked to maintain herds free of other pathogens have not worked well for PRRSV • Herds cleared of PRRSV infection can become reinfected despite all efforts to prevent reintroduction Disease severity: influence of management • Important sources of infection: – New introductions – Infected semen • Possible sources of infection: – Fomites: trucks, boots, coolers (for transporting semen), lunchboxes (!) • Fomite transport a bigger problem when cool (~34° F) – Flies, mosquitoes, mallard ducks – Airborne from neighboring farms Disease severity: influence of management • Other factors that impact maintenance of PRRSV-free status – Long-term, low-level infection with inapparent shedding – Imperfect diagnostic tests • No test yet discovered with 100% sensitivity and 100% specificity • At level of discrimination needed to keep 1000’s of pigs permanently virus-free, this matters • Some general recommendations: – If you’re going to live with the virus • Maintain immunity to endogenous strains by vaccination or planned exposure – Ensure herd-wide immunity: don’t let susceptible subgroups develop • Prevent introduction of new strains that could circumvent herd immunity – Screen new introductions, semen, watch out for fomites • Some general recommendations: – If you’re going to try to be PRRSV-free • Consider depopulation/repopulation • Undertake regular serologic and virologic testing to identify and segregate/remove infected animals • Once infected animals cleared, regularly monitor – Consider using multiple diagnostic tests to maximize sensitivity/specificity » Screening test: high sensitivity » Confirmatory test: suitable sensitivity, higher specificity • Exercise extreme vigilance to prevent introduction via new arrivals, semen, fomites