Echocardiography in Pulmonary Embolism
advertisement
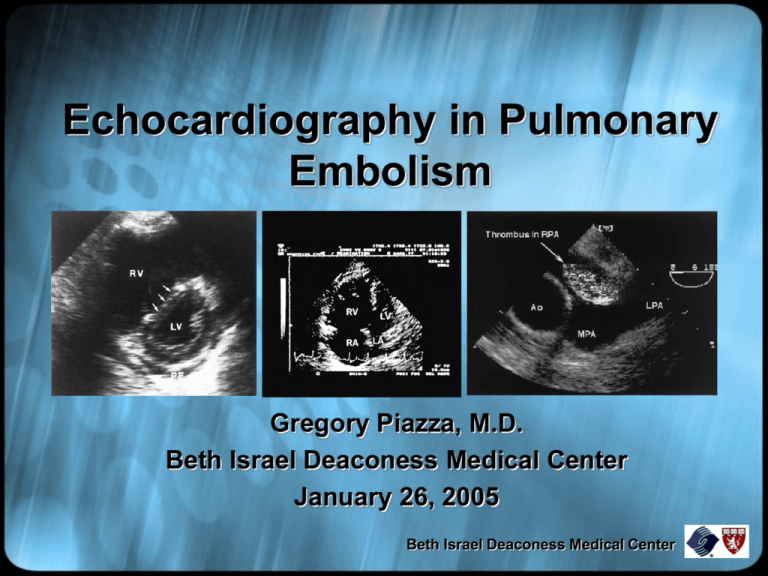
Echocardiography in Pulmonary Embolism Gregory Piazza, M.D. Beth Israel Deaconess Medical Center January 26, 2005 Beth Israel Deaconess Medical Center Objectives • To present a brief overview of the epidemiology, pathophysiology, diagnosis, and management of acute pulmonary embolism (PE). • To review the role of echocardiography in the diagnosis of PE. • To highlight the role of echocardiography in risk stratification of patients with PE. Beth Israel Deaconess Medical Center Epidemiology • The incidence of PE in the U.S. is approximately 1 per 1000 per year. • Only 1 out of every 3 cases of venous thromboembolism (VTE), including DVT and PE, is diagnosed. • With approximately 450,000 cases detected per year, a staggering 900,000 VTE cases may go undiagnosed annually. Lancet 1999;353:1386-1389 Lancet 2004;363:1295-1305 Beth Israel Deaconess Medical Center Epidemiology • In the Olmsted County registry, 30-day mortality after PE or DVT has been reported as high as 28%. • The International Cooperative Pulmonary Embolism Registry (ICOPER) estimates a 3-month mortality of 17.4%. • These data suggest PE is possibly as deadly as acute myocardial infarction. Arch Intern Med 1999;159:445-453 Circulation 2003;108:2726-2729 Beth Israel Deaconess Medical Center Pathophysiology • The most common sources of PE are the deep veins of the lower extremities and pelvis. • Thrombi dislodge from these veins and embolize to the pulmonary arterial tree where they trigger pathophysiologic changes in hemodynamics and gas exchange. • The size of the embolus, underlying cardiopulmonary status, and neurohumoral adaptations determine the hemodynamic response to PE. Circulation 2003;108:2726-2729 Beth Israel Deaconess Medical Center Pathophysiology www.benlovejoy.com/ pulmonary_embolism_main.html Beth Israel Deaconess Medical Center Pathophysiology • Physical obstruction, release of vasoconstrictors, and hypoxia lead to increased pulmonary vascular resistance (PVR) and right ventricular (RV) afterload. • RV pressure overload leads to chamber dilatation and hypokinesis, tricuspid regurgitation, and eventual RV failure. • RV pressure overload also causes interventricular septal flattening during systole and deviation towards the left ventricle (LV) during diastole leading to impaired LV filling. • As RV pressure overload worsens, RV wall stress and ischemia develop secondary to increased myocardial oxygen demand and decreased supply. Am Heart J 1995;130:1276-1282 Beth Israel Deaconess Medical Center Pathophysiology Pulmonary embolism ↑ PA pressure ↑ RV afterload ↑ RV wall tension ↑ RV O2 demand RV dilatation and dysfunction RV ischemia +/infarction ↓ RV O2 supply ↓ RV cardiac output Septal shift toward the LV ↓ coronary perfusion ↓ LV preload ↓ LV cardiac output Am Heart J 1995;130:1276-1282 Hypotension Beth Israel Deaconess Medical Center Spectrum of Disease • 1. 2. 3. 4. A variety of clinical syndromes may be seen: Normotensive with normal RV function Normotensive with RV dysfunction (submassive PE) Cardiogenic shock (massive PE) Cardiac arrest (massive PE) Beth Israel Deaconess Medical Center Diagnosis: History and Physical History: • Dyspnea (most frequent symptom) • Pleuritic chest pain • Cough • Hemoptysis • Syncope Physical: • Tachypnea (most frequent sign) • Anxious appearance • Tachycardia • Fever • Elevated JVD (most specific sign) • Loud P2 • Tricuspid regurgitation • Paradoxical bradycardia Beth Israel Deaconess Medical Center The Diagnostic Armamentarium • • • • • Arterial blood gases Electrocardiography Chest X-ray Plasma D-dimer Lower extremity ultrasound • Echocardiography (TTE and TEE) • Ventilation-perfusion lung scanning • Spiral chest CT • Magnetic resonance (MR) angiography • Contrast pulmonary angiography Beth Israel Deaconess Medical Center Diagnosis: An Integrated Approach History and Physical Eval. clinical likelihood Patient in ED Electrocardiogram Chest radiograph Patient already in hospital D-dimer Normal No PE Normal High V/Q if dye allergy or renal insufficiency Chest CT Positive Equivocal Normal Ultrasonography Positive No PE Lancet 2004;363:1295-1305 Treat for PE Negative Consider PA-gram No PE Beth Israel Deaconess Medical Center Diagnosis: Transthoracic Echocardiography • Transthoracic echocardiography (TTE) is insensitive in the diagnosis of acute PE. • In a prospective study, TTE failed to diagnose 50% of patients with angiographically proven PE. • However, in the appropriate clinical setting, findings of right ventricular pressure overload may help suggest acute PE as a diagnosis. Lancet 2004;363:1295-1305 Am J Med 2001;110:528-535 Beth Israel Deaconess Medical Center Diagnosis: Transthoracic Echocardiography Apical 4- chamber Parasternal short-axis Parasternal long-axis Am J Respir Crit Care Med 2002;166:1310-1319 Beth Israel Deaconess Medical Center Echocardiographic Findings In Acute PE • RV dilatation and hypokinesis • Interventricular septal flattening and paradoxical motion • Alteration of transmitral gradients with A wave > or = E wave • Tricuspid regurgitation (TR) • Pulmonary artery (PA) hypertension as estimated by the modified Bernoulli equation • RA dilatation • Loss of respiratory-phasic IVC collapse with inspiration • Patent foramen ovale • RA, RV, or pulmonary artery thrombus Ann Intern Med 2002;136:691-700 Beth Israel Deaconess Medical Center RV Dilatation • In the apical 4 chamber view, a ratio RVEDA (area) to LVEDA > 0.6 correlates with moderate RV dilatation. • A ratio > or = 1.0 correlates with major RV dilatation. Am J Respir Crit Care Med 2002;166:1310-1319 Beth Israel Deaconess Medical Center RV Hypokinesis • RV hypokinesis is frequently diagnosed in a qualitative fashion. • Quantitative methods, such as RV fractional area contraction, have not proven more accurate. • McConnell et al. noted a specific qualitative finding in patients with RV dysfunction and acute PE compared to patients with other causes of RV failure. • The McConnell sign is noted when RV free-wall hypokinesis in observed in the setting of relatively normal RV apical contraction. Am J Respir Crit Care Med 2002;166:1310-1319 Ann Intern Med 2002;136:691-700 Am J Cardiol 1996;78:469-473 Beth Israel Deaconess Medical Center RV Hypokinesis • • • Am J Cardiol 1996;78:469-473 The RV free-wall endocardium was traced in the apical 4-chamber view from base to apex at endsystole and end-diastole. Tracings from patients with RV dysfunction from acute PE were compared to those with RV dysfunction from pulmonary arterial hypertension. For PE, the McConnell sign had a sensitivity of 77%, specificity of 94%, PPV of 71%, and NPV of 96%. Beth Israel Deaconess Medical Center RV Hypokinesis Courtesy of A. Rosen Beth Israel Deaconess Medical Center Interventricular septal flattening and paradoxical motion • Right ventricular pressure overload leads to deviation of the interventricular septum towards the LV in diastole. • Interventricular septal flattening is seen during systole creating a socalled D-shaped LV. Diastole Systole Am J Respir Crit Care Med 2002;166:1310-1319 Ann Intern Med 2002;136:691-700 J Am Coll Cardiol 1987;10:1201-1206 Beth Israel Deaconess Medical Center Interventricular septal flattening and paradoxical motion Normal (diastole) Acute PE (diastole) Am J Respir Crit Care Med 2002;166:1310-1319 Beth Israel Deaconess Medical Center Alteration of Transmitral Gradients • In the setting of pericardial constraint, interventricular septal motion towards the LV during diastole leads to impaired LV filling. • Diastolic impairment leads to an A wave that is > or = to the E wave, signifying increased dependence on atrial contraction for LV filling. Normal PE Am J Respir Crit Care Med 2002;166:1310-1319 Beth Israel Deaconess Medical Center Alteration of Transmitral Gradients Courtesy of A. Rosen Beth Israel Deaconess Medical Center Tricuspid Regurgitation • RV pressure overload frequently results in tricuspid regurgitation detected on color flow and Doppler. RV RA LA Ann Intern Med 2002;136:691-700 www.geocities.com/SouthBeach/ Cove/2045/echo55.htm Beth Israel Deaconess Medical Center Pulmonary Hypertension • PA systolic pressure is estimated by using the modified Bernoulli equation: P = 4V2 where P = peak pressure gradient V = peak velocity of the TR jet • Estimated RA pressure is added to the gradient to approximate PA systolic pressure. Courtesy of A. Rosen Am J Respir Crit Care Med 2002;166:1310-1319 Ann Intern Med 2002;136:691-700 Beth Israel Deaconess Medical Center Thrombus In The Right Main PA Ann Intern Med 2002;136:691-700 Beth Israel Deaconess Medical Center Diagnosis: Transesophageal Echocardiography • Transesophageal echocardiography (TEE) can diagnose PE by direct visualization of the proximal pulmonary arteries. • Because the left main bronchus obstructs the view of the middle portion of the left pulmonary artery, PE is more difficult to detect in the left PA. • TEE may play a unique role in the diagnosis of PE in patients with unexplained cardiac arrest (especially pulseless electrical activity). Ann Intern Med 2002;136:691-700 Beth Israel Deaconess Medical Center Diagnosis: Transesophageal Echocardiography Long-axis transesophageal Short-axis transgastric Oblique transgastric Am J Respir Crit Care Med 2002;166:1310-1319 Beth Israel Deaconess Medical Center Diagnosis: Transesophageal Echocardiography Ann Intern Med 2002;136:691-700 Beth Israel Deaconess Medical Center Case Study • A 67 year old male with history of CAD, HTN, and prostate cancer presents with acute onset dyspnea and dull chest pressure. • On exam, he is tachycardic, tachypneic, hypoxic, but normotensive. He has elevated neck veins and new lower extremity edema. • His EKG reveals sinus tachycardia. • His chest X-ray is read as “no pneumonia, no CHF.” • Because of high clinical suspicion for PE, he undergoes chest CT. Beth Israel Deaconess Medical Center Case Study Beth Israel Deaconess Medical Center Case Study • The patient is started on a weight-based protocol of intravenous unfractionated heparin and admitted to a telemetry floor. • That evening, the patient’s roommate calls the nurses station to report that the patient has “slumped over in his chair.” • The patient is found unresponsive and a code is called. • The patient is found to be in pulseless electrical activity (PEA) and expires after resuscitative efforts are unsuccessful. Beth Israel Deaconess Medical Center Risk Stratification Risk Stratification Tools: • History and physical • Clinical prognostic scores • Cardiac biomarkers including cardiac troponin and brain-type natriuretic peptide (BNP) • Chest CT • Echocardiography Beth Israel Deaconess Medical Center History and Physical • ICOPER reported several independent clinical predictors of increased mortality at 3 months. Variable Hazard Ratio (95% CI) Age > 70 years 1.6 (1.1-2.3) Cancer 2.3 (1.5-3.5) CHF 2.4 (1.5-3.7) COPD 1.8 (1.2-2.7) SBP <90 mmHg 2.9 (1.7-5.0) Lancet 1999;353:1386-9 Beth Israel Deaconess Medical Center Cardiac Biomarkers • Cardiac troponins and BNP have been extensively studied in the evaluation of patients with acute PE. • Cardiac troponins and BNP accurately identify lowrisk PE patients with negative predictive values for inhospital death ranging from 97 to 100%. • Patients presenting with acute PE and elevated cardiac biomarkers should undergo transthoracic echocardiography to assess RV function. • In patients with acute PE and normal levels of cardiac biomarkers, echocardiography is not routinely required as RV function will most often be normal. Circulation 2003;108:2191-2194 Beth Israel Deaconess Medical Center Cardiac Biomarkers Reference n Biomarker Assay Cut-off level Test +,% NPV,% PPV,% Konstantinides et al19 106 cTnI Centaur (Bayer) 0.07 ng/ml 41 98 14 Konstantinides et al19 106 cTnT Elecsys (Roche) 0.04 ng/ml 37 97 12 Giannitsis et al20 56 cTnT TropT (Roche) 0.10 ng/ml 32 97 44 Janata et al21 106 cTnT Elecsys (Roche) 0.09 ng/ml 11 99 34 Pruszczyk et al23 64 cTnT Elecsys (Roche) 0.01 ng/ml 50 100 25 ten Wolde et al27 110 BNP Shionoria (CIS Bio) 21.7 pmol/L 33 99 17 Kucher et al26 73 Pro-BNP Elecsys (Roche) 500 pg/ml 58 100 12 Kucher et al25 73 BNP Triage (Biosite) 50 pg/ml 58 100 12 Pruszczyk et al22 79 Pro-BNP Elecsys (Roche) 153-334 pg/ml* 66 100 23 *Age and gender adjusted cut-off levels according to manufacturer. Abbreviations: n, number; NPV, negative predictive value; PPV, positive predictive value; cTnI, cardiac troponin I; cTnT, cardiac troponin T; BNP, brain-type natriuretic peptide; pro-BNP, pro-brain-type natriuretic peptide Accuracy of cardiac biomarkers for the prediction of in-hospital death in acute pulmonary embolism. Circulation 2003;108:2191-2194 Beth Israel Deaconess Medical Center Cardiac Biomarkers ↑ PVR ↑ RV pressure Circulation 2003;108:2191-2194 RV microinfarction ↑ RV shear stress Myofibril degradation ↑ Natriuretic peptide mRNA ↑ Troponins ↑ BNP Beth Israel Deaconess Medical Center Chest CT Scan • Although chest CT is used primarily for the diagnosis of PE, RV dilatation may also be observed. • In a study of 431 patients with acute PE diagnosed by chest CT, multiplanar reformats of axial CT data into CT 4-chamber views were performed. • Right and left ventricular dimensions (RVD and LVD) were measured. RV enlargement was defined as RVD /LVD > 0.9. • RV enlargement predicted 30-day death (hazard ratio, 5.17, p = 0.005) after adjusting for pneumonia, cancer, chronic lung disease, and age. Circulation 2004;110:3276-3280 Beth Israel Deaconess Medical Center Chest CT Scan Circulation 2004;109:2401-2404 Beth Israel Deaconess Medical Center Echocardiography • • RV dysfunction on echocardiography has been reliably established as a predictor of adverse outcomes in PE. The most commonly accepted quantitative standards are: 1. RV to LV end-diastolic diameter ratio > 1 in the apical 4-chamber view 2. RV end-diastolic diameter > 30 mm 3. Paradoxical interventricular septal systolic motion Ann Intern Med 2002;136:691-700 Beth Israel Deaconess Medical Center Echocardiography • At the Karolinska Institute in Sweden, 126 consecutive patients with PE were examined with TTE on the day of diagnosis. • After multivariate analysis, RV dysfunction emerged as the most powerful predictor of inhospital death. • A 6-fold increase in relative risk was noted in the patients with RV dysfunction compared to those with normal RV function. Am Heart J 1997;134:479-487 Beth Israel Deaconess Medical Center Echocardiography • In a cohort of 209 consecutive patients with PE, 31% presented with a combination of normal blood pressure and echocardiographic evidence of RV dysfunction. • Of these patients, 10% developed cardiogenic shock within 25 hours and 5% died in hospital. • None of the patients with normal RV function died from PE. Circulation 2000;101:2817-2822 Beth Israel Deaconess Medical Center Echocardiography • In ICOPER, 90-day mortality rate was increased in patients with RV dysfunction. • After multiple regression analysis, RV dysfunction was found to be an independent predictor of death at 90 days. Lancet 1999;353:1386-1389 Beth Israel Deaconess Medical Center Risk Stratification Algorithm No shock BNP ↓ Troponin ↓ Shock BNP ↑ Troponin ↑ Echocardiography No RV dysfunction Anticoagulation alone Circulation 2003;108:2191-2194 RV dysfunction Consider thrombolysis or embolectomy Beth Israel Deaconess Medical Center Management Primary therapy: • Thrombolysis • Open surgical embolectomy • Catheter-assisted embolectomy Secondary therapy: • IV unfractionated heparin • Low-molecular weight heparin (LMWH) • Fondaparinux • Warfarin • IVC filter Beth Israel Deaconess Medical Center Management • In patients with massive PE, primary therapy with thrombolytics is considered a lifesaving intervention. • Surgical or catheter-assisted embolectomy may be considered for massive PE if thrombolysis is contraindicated. • For submassive PE, thrombolysis remains controversial as no mortality benefit has been shown in this patient population. • However, MAPPET-3 demonstrated a reduction in need for escalation of therapy in patients receiving up-front t-PA (alteplase) for submassive PE. • Normotensive patients with normal RV function are considered low-risk and receive standard anticoagulation. J Thromb Thrombolysis 1995;2:227-229 N Engl J Med 2002;347:1143-1150 Beth Israel Deaconess Medical Center Thrombolysis in PE: Pre-Lytics *Following echo loops are courtesy of A. Kothavale Beth Israel Deaconess Medical Center Beth Israel Deaconess Medical Center Beth Israel Deaconess Medical Center Beth Israel Deaconess Medical Center Beth Israel Deaconess Medical Center Thrombolysis in PE: Post-Lytics Beth Israel Deaconess Medical Center Beth Israel Deaconess Medical Center Beth Israel Deaconess Medical Center Beth Israel Deaconess Medical Center Beth Israel Deaconess Medical Center Conclusions • Pulmonary embolism is a common and potentially life-threatening disorder. • Echocardiography is insensitive in the diagnosis of acute PE. • In conjunction with cardiac biomarkers, echocardiography plays a important role in risk stratification of patient with PE. Beth Israel Deaconess Medical Center The End… Beth Israel Deaconess Medical Center