HCLS$$ClinicalObservationsInteroperability$EMR
advertisement

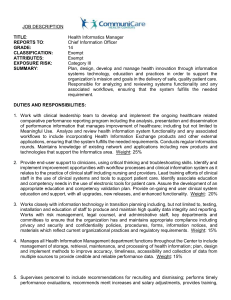
Medical Informatics Perspectives on Leveraging the Electronic Medical Record in Pharma November 8, 2006 Scot M. Silverstein, MD Assistant Professor of Healthcare Informatics and IT Director, Institute for Healthcare Informatics Drexel University, College of Information Science & Technology (Former Director of Published Information Resources & The Merck Index, MRL) Goals • Promote better understanding of Medical Informatics as a formal, cross-disciplinary clinical/IT specialty, lift veil of mystery that leads to misuse of term. • Raise awareness of national EMR initiatives on the provider side, and how these may be increasingly important to pharma in eClinical trials, post-marketing surveillance and other needs. • Raise awareness of difficulties in implementing largescale EMR, and how Medical Informatics professionals can help (interestingly, analogous “sociotechnical” issues are found in pharma). The iSchools Focus is on how people seek, use or interact with information using technology, not simply on technologic devices and computer programs. • University of California, Berkeley School of Information Management and Systems • University of California, Irvine The Don Bren School of Information and Computer Sciences • University of California, Los Angeles Graduate School of Education and Information Studies University of Michigan The School of Information University of North Carolina School of Information and Library Science The Pennsylvania State University School of Information Sciences and Technology • Drexel University College of Information Science and Technology • Florida State University College of Information • Georgia Institute of Technology College of Computing Rutgers, the State University of New Jersey School of Communication, Information, and Library Studies • University of Illinois Urbana-Champaign The Graduate School of Library and Information Science Syracuse University School of Information Studies • Indiana University School of Informatics University of Texas, Austin School of Information • Indiana University School of Library and Information Science • University of Maryland College of Information Studies University of Pittsburgh School of Information Sciences University of Toronto Faculty of Information Studies University of Washington Information School Guiding Principles of Medical Informatics: • Clinical IT will significantly benefit healthcare quality, efficiency and costs only if done well. • People issues are as critical towards success of clinical IT initiatives in the provider sector as well as in pharma. The challenge: • Deliver effective drug post-marketing surveillance in an increasingly “aggressive” marketplace. U.S. Government Accountability Office (GAO) • In a 2006 U.S. Government Accountability Office (GAO) report to Congress on drug safety requested after congressional hearings, a GAO investigation found that: – FDA lacks clear and effective processes for making decisions about, and providing management oversight of, postmarket safety issues. The process has been limited by a lack of clarity about how decisions are made and about organizational roles, insufficient oversight by management, and data constraints … There are weaknesses in the different types of data available to FDA, and FDA lacks authority to require certain studies and has resource limitations for obtaining data. Some of FDA's initiatives, such as the establishment of a Drug Safety Oversight Board, a draft policy on major postmarket decision making, and the identification of new data sources, may improve the postmarket safety decision-making process, but will not address all gaps … FDA is taking steps to identify additional data sources, but data constraints remain [1]. • [1] “Drug Safety: Improvement Needed in FDA’s Postmarket Decision-making and Oversight Process”, United States Government Accountability Office, Washington, D.C., March 2006, http://www.gao.gov/new.items/d06402.pdf , p. 5. Gartner “Predicts 2006” document: Life Science Manufacturers Adapt to Industry Transitions http://www.gartner.com/DisplayDocument?doc_cd=134309 • The swift and severe judgment in favor of the plaintiff in the first Merck Vioxx trial sent a shock wave through the biopharma industry. It shows that biopharma manufacturers must do more to ensure that healthcare providers and the public have an accurate, ongoing assessment of medication risks. Biopharmas must also ensure that information on these risks is communicated promptly in an open, understandable manner. Posting clinical trial information on a web site is one step towards greater transparency, but does not provide information in a way that [easily] enables ... comparisons of benefits and risks. • ... It is still well recognized that all the possible side effects of a medication cannot be uncovered using [only] a randomized sample of study subjects. The true test of [long-term] safety and efficacy can only be determined when trial data is combined with other sources of information such as clinical encounters, adverse events (MedWatch) or observational studies (National Registry of Myocardial Infarction). • In the future, it is hoped that the EMR system will capture point-of-care information in a standardized format that can be used for drug surveillance. Today, biopharmas must be content with these other available, if imperfect, information stores. Gartner Predicts 2006 (cont.) • Biopharmas ... should look at risk from multiple perspectives ... they must also get actively involved in defining the electronic health and medical record so that it will contain the type of information required to make better safety assessments in the future. • Biopharmas that ignore the opportunity to use analytical tools to proactively review contradictory sources of study information (for example, pre- and post-approval clinical data sets, as well as registries) will miss essential signals regarding product safety. Yet today, only a small percentage of biopharmas routinely utilize personnel with medical informatics backgrounds to search for adverse events in approved drugs. Institute of Medicine weighs in • The Committee on the Assessment of the US Drug Safety System of the Institute of Medicine has written that: – … the committee believes there is an abundance of extraordinary research opportunities that could substantially enhance the [FDA’s] regulatory processes with respect to both the efficacy and safety of new therapeutics. Many of the opportunities involve the creation of new algorithms and methods to improve the processes of preclinical and clinical drug development and new processes to enable effective safety and efficacy monitoring and evaluation over the entire lifecycle of a therapeutic [1]. – [1] “The Future of Drug Safety: Promoting and Protecting the Health of the Public”, Committee on the Assessment of the US Drug Safety System, Alina Baciu, Kathleen Stratton, Sheila P. Burke, Editors, Board on Population Health and Public Health Practice (BPH), Institute of Medicine (IOM), 2006, Recommendation 4.6, p. 104-105, http://fermat.nap.edu/books/0309103045/html/104.html Institute of Medicine weighs in (cont.) • In its new 2007 report “Preventing Medication Errors: Quality Chasm Series”, the Committee on Identifying and Preventing Medication Errors of the Institute of Medicine has written that: – Informatics experts should track progress on the national health-information infrastructure, look for opportunities to gather information about drug safety and efficacy after approval, coordinate partnerships with external groups to study the use of electronic health records for [drug] adverse event surveillance, participate in FDA’s already strong role in setting national standards and track the development of tools for data analysis in industry and academe, and encourage the incorporation of the tools into FDA practice where appropriate [1]. – [1] “The Future of Drug Safety: Promoting and Protecting the Health of the Public”, Committee on the Assessment of the US Drug Safety System, Alina Baciu, Kathleen Stratton, Sheila P. Burke, Editors, Board on Population Health and Public Health Practice (BPH), Institute of Medicine (IOM), 2006, Recommendation 4.6, p. 102, http://fermat.nap.edu/books/0309103045/html/102.html What is Medical Informatics? • Medical Informatics studies the organization of medical information from fine-grained levels (e.g., biomedical data modeling) to macro levels (e.g., MedDRA, UMLS), the effective use, management and dissemination of information using computer technology (e.g., EMR, CDSS, CPOE), and the impact of such technology on medical research, education, and patient care. • Formal, NIH-sponsored field on which NIH has provided many millions of dollars in training grants for ~ the last two decades. • Has been nearly invisible to pharma for numerous reasons, largely due to misunderstanding of the field. Unfortunate. • e.g., My analysis in PIR ca. 2000 identified significant cheminformatics and biomedical informatics gaps, and through innovative use of technology and compelling arguments we increased funding and availability of targeted scientific information to MRL R&D at least tenfold by late 2003 over averages kept since ~ 1989. eJournals /Alertlink/ SciFinder / CrossFire etc. The Informatics Subspecialties NIH training programs in Medical Informatics http://www.nlm.nih.gov/ep/GrantTrainInstitute.html 1-Harvard-MIT Division of Health Sciences & Technology, 2-Yale University, 3-Columbia University, 4-University of Pittsburgh, 5Johns Hopkins University, 6-Medical University of South Carolina, 7-Vanderbilt University, 8-Indiana University - Purdue University at Indianapolis, 9-University of Wisconsin Madison,10-University of Minnesota Twin Cities, 11-University of Missouri Columbia, 12-Rice University, 13-University of Utah, 14-University of California Irvine, 15-University of California Los Angeles, 16-Stanford University, 17-Oregon Health & Science University,18-University of Washington (training is provided by other universities via internal funds as well). Medical Informatics: What it is not • • The increasingly common use of awkward expressions like "informatics technology" to refer to clinical information systems is an example of semantic blur. Medical informatics is a formal field of study and a scientific discipline. Computers in medicine is not the equivalent of medical informatics. Yet, position descriptions such as in these employments ads, with requirements for neither clinical nor medical informatics training or experience, are often seen. From the Philadelphia Inquirer: – Medical informatics analyst. [Company name] seeks a Medical Informatics Analyst to support resource management and medical affairs in their data analysis needs. Through downloading of MCS database, PC-based analysis of clinical and clinically-relevant financial data will be performed. Qualifications: BA/BS in computer science or related discipline, 3-5 years experience in PC-based data analysis of health care information, knowledge of SAS or similar analysis software, knowledge of mainframe DB2 database architectures, working knowledge of CPT-4 and ICD-9-CM coding." – From an Internet biomedical employment service, Medzilla.com: [Company name] seeks a Director of Clinical Informatics. Overall coordination of design specifications, implementation and support for all internet/browser based systems. Assurance of continued, reliable and consistent resources and applications to all corporate personnel and external users who may rely upon these systems. Documentation and control of said software systems including package systems and license control if necessary. Provide ongoing maintenance oversight and management support for said systems. Organize and train personnel, both internal and external, who will be using said products. Client contact and development and assist Sales and Marketing as necessary in client presentations. Minimum of a BA. MBA preferred. Medical Informatics: what it is not • Blur in usage of the term "medical informatics" is highly ironic. One major area of study in medical informatics research is language (e.g., controlled terminologies, computation linguistics) and data modeling. • In applied efforts in that area, exhaustive attention to lexical and semantic issues and intense thinking about precision and imprecision in language have led to excellent tools such as the National Library of Medicine's Unified Medical Language System. Now, it seems the medical informatics field is often finding its own name used in an imprecise way. • Imagine impact of similar difficulty with, say, Medicinal Chemistry… Why is Medical Informatics Important to EMR and other healthcare IT initiatives? • A number of very expensive healthcare IT project difficulties and failures have appeared in the literature in recent years in large part due to organizational change resistance, internal political struggles, lack of expertise in IT implementation processes most suitable for clinical environments, and other sociotechnical issues. – – – – – – Cedars-Sinai Hospital in Los Angeles [Doctors pull plug on paperless system. American Medical News, Feb. 17, 2003] Hospital of the University of Pennsylvania [Role of computerized physician order entry systems in facilitating medication errors. Koppel et al., JAMA 2005;293(10):1197-203] VA hospital CoreFLS failure - $472 million [http://www.usmedicine.com/article.cfm?articleID=932&issueID=66] United Kingdom NHS initiative [Doctors fear £6bn IT project will be a fiasco. The Guardian, February 8, 2005. [http://society.guardian.co.uk/internet/story/0,8150,1407903,00.html] Others [website Sociotechnical Issues in Health IT: Common Examples of Health IT Failure] Pharma examples – CRISP project - In the 1990s, [pharma] struggled to erect a modernized clinical data system known as CRISP (Clinical and Regulatory Information Strategic Program), a project that current and former information systems workers came to regard as a $100 million loss. "This project ran into a lot of problems," says one former manager who was involved near the beginning of the CRISP project. [http://www.baselinemag.com/article2/0,1397,1608582,00.asp] Why is Medical Informatics important? (cont.) • Healthcare IT and its environment are core competence • Recognition that organizations are simultaneously social (people, values, norms, cultures) and technical (tools, equipment, technology). These elements are deeply interdependent and interrelated. Good design and implementation is not just a technology issue but also one of jointly optimizing the combined sociotechnical systems. • Medical Informatics training recognizes these issues and trains crossdisciplinary specialists accordingly. Curriculum example: – Fundamental of computer science Medical language and terminology systems Modeling of medical observations and data Medical coding systems Medical knowledge structures Information organization and flows in medical practice Quantitative models for medical decision making Clinical decision support Medical image processing User interfaces and ergonomics in healthcare Health information systems architecture Security and confidentiality Ethical and legal issues in electronic medical records Organizational and sociological issues in clinical IT projects Metrics and methods for evaluating healthcare information systems Cost and investment issues in healthcare IT National EMR Initiatives: U.S. • Transforming Health Care: The President’s Health Information Technology Plan – http://www.whitehouse.gov/infocus/technology/economic_policy200404/chap3.html – President Bush has outlined a plan to ensure that most Americans have electronic health records within the next 10 years. The President believes that better health information technology is essential to his vision of a health care system that puts the needs and the values of the patient first and gives patients information they need to make clinical and economic decisions – in consultation with dedicated health care professionals. • Office of the National Coordinator for Healthcare IT (ONCHIT)established April 2004 – http://www.hhs.gov/healthit/ National EMR Initiatives: U.K. • National Programme for IT in the NHS (described as “the world’s biggest government IT project”) – – • http://www.connectingforhealth.nhs.uk/ The National Programme for IT, delivered by the new Department of Health agency NHS Connecting for Health, is bringing modern computer systems into the NHS to improve patient care and services. Over the next ten years, the National Programme for IT will connect over 30,000 GPs in the U.K. to almost 300 hospitals and give patients access to their personal health and care information, transforming the way the NHS works. The infrastructure will include new components integrated into existing national reporting databases: – – A centralized national database, called the NHS Care Record, to include all patient electronic health records. This data will likely be useful for epidemiological studies and drug surveillance on a national scale (!) A Patient Demographics Services operation that will act as an enterprise master patient index (EMPI) for the entire country, based on the patient's NHS number, a national patient identifier, and demographic and patient encounter information. Pharma takes notice: Integrating Patient Information with Drug Development Nov. 2005: “Merging Electronic Health Records & Electronic Data Capture: Integrating Patient Information with Drug Development” http://exlpharma.com/events/ev_brochure.php?ev_id=17 • Exploring the Opportunity for Collaboration with Drug & Device Firms in Accelerating IT Adoption by Hospitals & Physicians: The government’s 10-year plan to automate healthcare information exchange by creating the National Healthcare Information Network presents an undeniable opportunity to synchronize patient information with drug development and increase the overall quality of patient care. • Drug & device companies have been struggling for years to successfully and efficiently move away from paper data collection towards electronic data capture and automated trials. Without a unifying body behind this push, data standards, interoperability and infrastructure compatibility have not been achieved. By piggy-backing on this government-lead initiative to automate healthcare, drug and device firms can reap the benefits of the increased efficiency IT adoption at the hospital and physician level will offer and utilize this data for more streamlined drug development [and other uses – ed.] • ExL Pharma’s Merging EHR & EDC Conference is the “first opportunity for drug & device firms to gather with hospitals, physicians and vendors to discuss strategies for accelerating IT adoption and achieving cross-functional data interoperability to streamline processes, improve communication and maximize patient care.” KEYNOTE PRESENTATION Improving Patient Care while Optimizing Efficiency: Outlining the Potential Benefits from Merging Patient Care and Drug Development Efforts Barbara Tardiff, MD, MBA Executive Director, Research Information Services, Clinical & Regulatory Information Services MERCK & CO., INC. HOSPITAL PERSPECTIVE: The Challenges and Limitation of Merging Electronic Health Information Robert N. Hotchkiss, MD Director, Clinical Research HOSPITAL FOR SPECIAL SURGERY STANDARDIZATION EFFORTS: Interchange Standards: The Key to Linking Healthcare and Clinical Research Information Rebecca Kush, PhD, President, CDISC Landen Bain, Healthcare Liaison, CDISC Sue Dubman, Director of Applications for the Center of Bioinformatics, NCI Upcoming DIA-sponsored conference • “The Quest to Enable the Electronic Clinical Trial: Finding Clarity in a Confusing World” (Dec. 2006, http://www.diahome.org/product/11116/06029.pdf ) • Learning objectives: – Discuss medical informatics opportunities to improve the benefit-risk assessment of drugs – Explain standard controlled terminology and its current and future use – Summarize how changes in the drug development industry impact people and processes – Discuss how clinical research can help drive the adoption of healthcare IT standards – Describe how increasing data transparency can benefit the public interest EMR for post-market surveillance: possible? • Use of EMR for drug surveillance has begun to be studied. There have been exploratory studies on this topic and related areas: – – – – – Murff et. al. reviewed current methodologies for detection of clinical adverse events including electronic methods that can detect events using coded data, free-text clinical narratives, or a combination of techniques [1] Gandhi et. al conducted a similar review specifically aligned to drug safety issues and believe computerized monitoring for adverse drug events using rules or “triggers” is a high yield and relatively inexpensive strategy that should be adopted by healthcare organizations [2]. Nebeker et. al. described prospective daily reviews of EMR data performed by pharmacists as an effective way to detect adverse drug events [3]. Honigman et. al. reported on an automated, computer-based retrospective analysis for adverse drug events of one year of data from an EMR, including records on over 23,000 patients. The conclusion was that computerized search programs can detect adverse drug events in such data and that such detefction programs demonstrate “value added” for the EMR [4]. Efforts in using EMR’s for drug post-marketing surveillance can also serve as a test bed for identifying and resolving issues in broader uses of national EMR of even greater significance, such as syndromic surveillance for early epidemic detection or detection of chemical terrorism or bioterrorism. Syndromic surveillance refers to using health-related data that precede diagnosis and signal a sufficient probability of a case or an outbreak to warrant further public health response. Hegmann et. al. described a system to detect possible bioterrorist attacks during the 2002 Olympic Games using an EMR-based bioterrorism surveillance system. The system implemented 50 different analyses that examine a range of symptoms to detect and track infectious diseases [5]. • • • • • [1] “Detecting adverse events for patient safety research: a review of current methodologies”, Murff HJ, Patel VL, Hripcsak G, Bates DW, Journal of Biomedical Informatics, 36(1-2):131-143, Feb-Apr 2003. [2] “Identifying drug safety issues: from research to practice”, Gandhi TK, Seger DL, Bates DW, International Journal for Quality in Health Care, 12(1):6976, Feb. 2000. [3] “High rates of adverse drug events in a highly computerized hospital”, Nebeker JR, Hoffman JM, Weir CR, Bennett CL, Hurdle JF, Archives of Internal Medicine 165 (10): 1111-1116, May 23 2005. [4] “Using computerized data to identify adverse drug events in outpatients.” J Am Med Inform Assoc. 2001 May-Jun;8(3):254-66. [5] “Computer model developed at U. Utah monitors bioterrorism”, Daily Utah Chronicle (U. Utah), Feb. 4, 2002 EMR for postmarket surveillance (cont.) • Utilizing large quantities of EMR data, innovative statistical models and methods for analysis of extremely large datasets (large number of observations or large number of dimensions), an active area of research, will be necessary to supplement and replace more simplistic methodologies (e.g., adverse event frequency comparisons) for leveraging EMR data. Research in computational statistics, for example, involves the development of visualization and computationally intensive methods for mining large, nonhomogeneous, multi-dimensional datasets so as to discover knowledge in the data [1]. • Research has been done specifically in the application of data mining techniques in drug surveillance. The authors of one study describe knowledge discovery in databases (KDD), a technique to detect potential adverse drug events involving the selection of data variables and databases, data preprocessing, data mining and data interpretation and utilization. They describe data mining as encompassing a number of statistical techniques including cluster analysis, link analysis, deviation detection and “disproportionality” assessment which can be utilized to determine the presence of and to assess the strength of adverse drug event signals. The authors concluded that in view of the importance of adverse drug events and the development of massive data storage systems and powerful computer systems, the use of data mining techniques in knowledge discovery in medical databases is likely to be of increasing importance in the process of drug surveillance as they are likely to be able to detect signals earlier than more common methods currently in use [2]. • • [1] Computational Statistics in the Data Sciences, George Mason University, http://www.scs.gmu.edu/~jgentle/compstat/index.html [2] “Application of data mining techniques in pharmacovigilance.” Wilson AM, Thabane L, Holbrook A., Br J Clin Pharmacol. 2004 Feb;57(2):119-20. False assumption and underestimations: implementing EMR not as easy as it seems • Medical informaticists study the issues that impede EMR adoption in clinical settings. • What you didn’t want to know about clinical information technology in large medical centers: (compare issues to your own project difficulties in pharma or CRO settings): – See “Sociotechnologic issues in clinical computing: Common examples of healthcare IT failure” at http://www.ischool.drexel.edu/faculty/ssilverstein/medinfo.htm Access Patterns to a Website on Healthcare IT Failure Scot M. Silverstein MD, Yunan Chen, Christine Wania College of Information Science & Technology, Drexel University Visitor types Background 3000 Organizational and human factors (sociotechnical) issues associated with healthcare IT have led to project difficulties and failures. Detailed case accounts might improve knowledge sharing between healthcare organizations on lessons learned and best implementation practices. Based on an online search for web-based resources, there appears to be few relevant sites containing either high-level or case-level information regarding healthcare IT difficulty and failure. Case-level accounts describing issues at a fine level of granularity, such as detailed accounts of interactions among clinicians, IT personnel and healthcare executives, are potentially useful learning resources. Knowledge sharing via the Web on best practices for management of sociotechnical impediments to healthcare IT is thus suboptimal. 2842 2500 2000 1500 1000 564 332 500 239 149 97 93 11 0 ISP Note: The terms in this diagram represent our categorization of the concepts used by Web searchers to find our website. For example: “healthcare IT” might have been expressed as “medical computing” or “clinical information technology.” University / Other Healthcare Educational Organization Organization Institution Unknown Government Organization Healthcare Related Industry Other Individual Visitor Countries distribution Case Study Results Research Questions We studied access patterns to our website on healthcare IT difficulties. The distribution of countries, website visitor types and query types are shown in the following charts: To illustrate the level of interest and knowledge sharing about Healthcare IT difficulties, we explored two research questions: What case-level information about healthcare IT project difficulty and failure is available via the Web? Who is seeking this information? Visitor Input Types 2500 2252 2000 Methods 1500 Conclusion 1000 We used our website, entitled “Sociotechnologic Issues in Clinical Computing: Common Examples of Healthcare IT Failure”, online since 1999, as a representative information resource. We first conducted a detailed Web search on various search phrases representing the concept “healthcare IT failure” using three major search engines (Google, Yahoo, and MSN). The results showed that our website was nearly unique. We then tracked views of our website from Sep 27th, 2005 to June 30th, 2006 with a free public tracking service, eXTReMe Tracking (http://extremetracking.com). 206 500 166 132 0 Search Engine Healthcare IT Site Other Non Healthcare IT Site Visitor Search Engine Referrer Input 774 800 700 600 423 500 Our website “Sociotechnologic Issues in Clinical Computing: Common Examples of Healthcare IT Failure” is at URL: 389 400 We examined the access logs to determine viewer IP and referrer (primarily search engine query, or link from another site) to identify viewer demographics including country and organization type, where available. No personally-identifiable information was sought or obtained. It appears there is an ongoing interest in information about healthcare IT difficulty among searchers of varied demographics, as evidenced by searches on these issues and resultant “hits” on our website, one of the few websites that specifically addresses these issues. At present such material is uncommon. We believe Medical Informatics specialists can contribute significantly to filling this information gap, and that doing so would be very helpful to the healthcare IT community. 227 300 193 200 116 100 0 Healthcare OR IT OR Failure Healthcare AND IT IT Failure Healthcare IT Failure Unrelated Project Management http://www.ischool.drexel.edu/faculty/ssilverstein/medinfo.htm It was created by our first author via an informal collaboration of AMIA clinical information systems working group members (CISWG) during 1998-2001. Why is good clinical IT difficult? • Lindberg: “Computer Failures and Successes”, Southern Medical Bulletin 1969;57:18-21 – • Nemeth & Cook: “Hiding in Plain Sight”, Journal of Biomedical Informatics 38 [2005], 262–263 – • Computer experts per se have virtually no idea of the real problems of medical or even hospital practice, and furthermore have consistently underestimated the complexity of the problems…in no cases can [building appropriate clinical information systems] be done, simply because they have not been defined with the physician as the continuing major contributor and user of the information. Just beneath the apparently smooth-running operations [of healthcare] is a complex, poorly bounded, conflicted, highly variable, uncertain, and high-tempo work domain. The technical work that clinicians perform resolves these complex and conflicting elements into a productive work domain. Occasional visitors to this setting see the smooth surface that clinicians have created and remain unaware of the conflicts that lie beneath it. The technical work that clinicians perform is hiding in plain sight. Those who know how to do research in this domain can see through the smooth surface and understand its complex and challenging reality. Occasional visitors cannot fathom this demanding work, much less create IT systems to support it. Wears & Berg: “Still Waiting for Godot”, JAMA Vol. 294 No. 2, July 13, 2005 – Throwing IT at a health care system to remedy high medication error rates will not be effective unless the organizational reasons for those failures also are addressed. These reasons are hidden in the "messy details" of clinical work: complexity; uncertainty; conflicting goals; gaps in supplies, procedures, and coordination; brittleness of tools and organizational routines. The often divergent goals of three main groups within a medical center From Sittig DF, Sengupta S, al-Daig H, Payne TH, Pincetl P. The role of the information architect at King Faisal Specialist Hospital and Research Centre. Proc Annu Symp Comput Appl Med Care. 1995;:756-60 The Three Stakeholder Groups in More Detail Administration (purchasers) • CEO • COO • CFO • Gen Counsel • CIO • IT staff • Consultant Information Technology (implementers) • Clin leaders (SVP, COS, Dept. Chairs) • Clinicians • Service Mgr. Medicine (users) Observed Drivers: Health System Administration Chief Executive Officer (CEO) Chief Financial Officer (CFO) Chief Operating Officer (COO) General Counsel Institutional reputation Board issues Internal relationships Financial issues Up-front costs (capital & expense) Secondary dollars (longer-term clinical revenue/technologic expense) “Return on investment” Skepticism Operational changes (in processes) Managerial control Staffing Costs Liability / litigation on: Clinical issues Information security Observed Drivers: Information Technology (MIS) Chief Information Officer (CIO) IT Staff Consultants Budget - effects on other projects, especially MIS (management information systems) “Plug and Play” - ease of implementation, human resource s IT control - territoriality IT reputation - insecurity in new clinical domain Fear - clinical environments are alien to MIS Hands-on technology issue s Job stability Revenue Client satisfaction Future engagements Observed Drivers: Clinicians Clinical Leadership (Chief of Staff, VP for Medical Affairs, Department Chairs, Nursing VP) Clinicians (primary users) Service Line Administrator Change to clinician workflow Complaints Care issue s Usefulne ss of system (dataset issue s, adaptability - opposite of plug and play) Work changes / time issue s Effects on care quality Liability “Grading” & physician practice reporting Income Effects on busine ss development Institutional reputation Clinician relations The undesired dynamics Administration • CEO • COO • CFO • Gen Counsel • CIO • IT staff • Consultant Information Technology • Clin leaders (SVP, COS, Dept. Chairs) • Clinicians • Service Mgr. Medicine Medical Informatics as Intermediary Administration • CEO • COO • CFO • Gen Counsel MI • CIO • IT staff • Consultant Information Technology • Clin leaders (SVP, COS, Dept. Chairs) • Clinicians • Service Mgr. Medicine The desirable dynamics Administration • CEO • COO • CFO • Gen Counsel MI • CIO • IT staff • Consultant Information Technology • Clin leaders (SVP, COS, Dept. Chairs) • Clinicians • Service Mgr. Medicine Medical Informatics role • Responsible for helping these three groups understand they are all working toward the same goal, and ensuring medical center personnel collaborate efficiently and productively. • Understanding and work with the stakeholder drivers (motivators) and dynamics (interactions) in detail will help the MI proactively intervene and avoid retrospective correction after problems have arisen. Take-away points • The emerging national EMR’s will provide a useful resource for postmarketing drug surveillance activities and research. • Clinical IT projects are complex social endeavors that happen to involve computers, as opposed to information technology projects that happen to involve doctors. • An understanding of the internal dynamics by the medical informaticist is an important asset towards facilitating success of EMR initiatives and optimal leveraging of its capabilities for healthcare providers – and for pharma. • This understanding and experience relative to clinical IT is portable to pharma and can be of great value in other eClinical initiatives and in collaborations with the provider side. Additional Reading • Managing Technological Change: Organizational Aspects of Health Informatics. Nancy M. Lorenzi, Robert T. Riley (Springer-Verlag, 2nd edition, 2004, http://www.amazon.com/ManagingTechnological-Change-Organizational-Informatics/dp/0387985484 ). • Advance for Health Information Executives: “Medical Informatics, Friend or Foe”, R. Gianguzzi, May 1, 2002, p. 37-38 Dean Sittig, Director of the national Clinical Informatics Research Network (CIRN) for Kaiser Permanente: "There are many different constituencies, and hence views, which must be considered when attempting to develop an integrated clinical information management system in any large medical center ... we believe that without a full-time, on-site [medical informaticist], the difficulty of the task increases to the point of becoming nearly impossible." Questions? SAYGR Registry Yale-Saudi Arabia Collaboration in Clinical Genetics & Birth Defects Dec. 1995 Informatics can take us to esoteric places: Red Sand Dunes area, ~ 50 km w. of Riyadh