ADULT ECHOCARDIOGRAPHY ABBREVIATIONS
advertisement

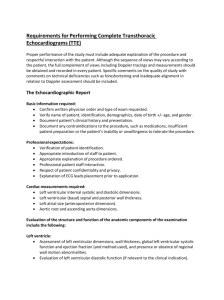
ADULT ECHOCARDIOGRAPHY COURSE Harry H. Holdorf PhD, MPA, RDMS (Ab, OB/Gyn, BR), RVT (VT), LRT(AS), N.P. INTRODUCTION Table of Contents Objectives Adult Echocardiography T of C 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. Abbreviations Anatomy and Hemodynamics Cardiac Physiology Technique and Patient Care The aortic valve The pulmonic valve The mitral valve The tricuspid valve Valvular heart disease Coronary Anatomy Prosthetic valves Cardiomyopathies Diastolic Dysfunction Table of contents cont… 14. The pericardium 15. Hypertensive Heart Disease 16. Ischemic Heart Disease 17. Adult Congenital Heart Disease 18. Foreign Bodies, Masses, and Myxomas 19. EKG-Electrocardiogram 20. Lectures on Adult Echocardiography 21. Final Exam prep 1 22. Final Exam prep 2 23. Final Exam Objectives Interact appropriately with the patient, physicians and staff. Identify the pertinent clinical questions and the goal of the examination. Recognize significant clinical information and historical facts from the patient and the medical records, which may impact the diagnostic examination. Review data from current and previous examinations to produce a written/oral summary of technical findings, including relevant interval changes, for the reporting physician’s reference. Select the correct transducer type and frequency for examination(s) being performed. Adjust instrument controls including examination presets, scale size, focal zone(s), overall gain, time gain compensation, and frame rate to optimize image quality. Demonstrate knowledge and understanding of Doppler ultrasound principles, spectral analysis, and color flow imaging relevant to and in the AE specialty. Demonstrate knowledge and understanding of anatomy, physiology, pathology and pathophysiology relevant to and in the AE specialty. Demonstrate the ability to perform sonographic examinations of the appropriate organs and areas of interest according to professional and employing institution protocols relevant to and in the AE specialty. Recognize, identify and document the abnormal sonographic patterns of disease processes, pathology, and pathophysiology of the organs and areas of interest. Modify the scanning protocol based on the sonographic findings and the differential diagnosis relevant to and in the AE specialty. Perform related measurements from sonographic images or data. Utilize appropriate examination recording devices to obtain pertinent documentation of examination findings. Lecture one ABBREVIATIONS Abbreviations • • • • • • • • • • • • • • AR Ao AoV ASD ASH AV BBB BP BPM BSA CHF CI CM CO Aortic Regurgitation (AI) Aorta Aortic valve Atrial Septal Defect Asymmetric Septal Hypertrophy Atrioventrical Bundle Branch Block Blood Pressure Beats Per Minute Body Surface Area Congestive Heart Failure Cardiac Index Cardiomyopathy Cardiac Output • • • • • • • • • • • • • • COPD Chronic Obstructive Pulmonary Disease CPI Cardiovascular Principles and Instrumentation CS Coronary Sinus CVA Cerebral Vascular Accident CW Continuous Wave Doppler DA Ductus Arteriosus DM Diastolic Murmur DOE Dyspnea and Exertion ed End Diastolic EF Ejection Fraction ECG Electorcardiogram (EKG) FO Foramen Ovale HCM Hypertrophic Cardiomyopathy HOCM Hypertrophic Obstructive Cardiomyopathy • • • • • • • • • • • • • • • • IHSS Idiopathic Hypertrophic Subaortic Stenosis IVC Inferior Vena Cava L Liter LA Left Atrium LAD Left Anterior Descending Coronary Artery LAX Long Axis View LSB Left Sternal Border LV Left Ventricle LVEDP Left Ventricular End Diastolic Pressure LVET Left ventricular Ejection Time LVH Left Ventricular Hypertrophy LVOT Left Ventricular Outflow Tract MHz Megahertz MAC Mitral Annular Calcification MI Myocardial Infarction ml Milliliter • • • • • • • • • • • • • • • mm Hg Millimeters of Mercury MR Mitral Regurgitation MS Mitral Stenosis MV Mitral Valve MVA Mitral Valve Area MVP Mitral Valve Prolapse O2 Oxygen OS Opening Snap PA Pulmonary Artery PDA Patient Ductus Arteriosus PE Pericardial Effusion PEP Pre-Ejection Period PHTN Pulmonary Hypertension PR Pulmonic Regurgitation PS Pulmonic Stenosis • • • • • • • • • • • • • • PV Pulmonary Valve (or vein) PVC Premature Ventricular Contraction PVD Peripheral Vascular Disease PW Pulsed Wave Doppler Q Flow RA Right Atrium RAP Right Arterial Pressure RCA Right Coronary Artery RUSBRight Upper Sternal Border RV Right Ventricle RVH Right Ventricular Hypertrophy RVOTRight Ventricular Outflow Tract RVSPRight Ventricular Systolic Pressure SA Sinoatrial • • • • • • • • • • • • • • SAM Systolic Anterior Motion SAX Short Axis View SBE Subacute Bacterial Endocarditis SBP Systolic Blood Pressure SV Stroke Volume SVC Superior Vena Cava TGV Transposition of the Great Vessels TR Tricuspid Regurgitation TS Tricuspid Stenosis TV Tricuspid Valve UA Umbilical Artery UV Umbilical Vein VSD Ventricular Septal Defect WPW Wolf-Parkinson-White Syndrome Aortic Regurgitation AR Aorta Aortic Valve ASD Asymmetric Septal Hypertrophy Atrioventricular AV Bundle Branch Block BBB Blood Pressure Beats per minute Body surface area In simple terms Body Surface Area is the area covered by one’s skin the largest organ of the body 1.It is often a clinical measure used by physicians 2. to calculate the drug dosages and for administration of intravenous fluids Congestive heart failure Cardiac Index • • • A large person has a higher cardiac output than a small person. The cardiac index represents cardiac output that has been adjusted to a person's size. Dividing cardiac output by the person's body surface area, or BSA, will provide the cardiac index. Cardiac output correlates better with body surface area than weight. Cardiac output that is expressed per square meter of body surface area is termed cardiac index. Cardiomyopathy Cardiac Output Chronic Obstructive Pulmonary Disease (COPD) Cardiovascular Principles and Instrumentation Coronary Sinus Cerebral Vascular Accident Continuous Wave Doppler Ductus Arteriosus Diastolic Murmur Dyspnea and Exertion End Diastolic Ejection Fraction Electrocardiogram (EKG) Foramen Ovale PFO Hypertrophic Cardiomyopathy Hypertrophic Obstructive Cardiomyopathy Idiopathic Hypertrophic Subaortic Stenosis Inferior Vena Cava Liter = heart pumps 5-7 liters of blood per minute Left Atrium Left Anterior Descending Coronary Artery Long Axis View Left Sternal Border Left Ventricle Left Ventricular End Diastolic Pressure • Left Ventricular end-diastolic pressure (LVEDP): • The pressure in the Left ventricle at the end of diastole, (usually measured in the left ventricle) as an approximation of the enddiastolic volume, or preload. Left Ventricular Ejection Time The time for the ejection of blood from the left ventricle, beginning with aortic valve opening and ending with aortic valve closure. Left Ventricular Hypertrophy Left Ventricular Outflow Tract Megahertz Mitral Annular Calcification Myocardial Infarction Milliliter Millimeters of Mercury Mitral Regurgitation Mitral Stenosis Mitral Valve Mitral valve area • Aortic Annulus Size cm Mitral Annulus Size cm Aortic VTI Mitral VTI 1.8-2.3 3.0-3.5 18-25 cm 10-13 cm Mitral Valve Prolapse MVP: Mitral valve prolapse is a condition in which the two valve flaps of the mitral valve do not close smoothly or evenly. Mitral valve prolapse is also known as click-murmur syndrome, Barlow's syndrome or floppy valve syndrome. When the heart contracts, part of one or both flaps collapse backward into the left atrium. In some cases, the prolapsed valve lets a small amount of blood leak backward through the valve, which may cause a heart murmur. Oxygen Opening snap Pulmonary Artery Patient Ductus Arteriosus • • • Patent ductus arteriosus (PDA) is a condition in which the ductus arteriosus does not close. The ductus arteriosus is a blood vessel that allows blood to go around the baby's lungs before birth. Soon after the infant is born and the lungs fill with air, the ductus arteriosus is no longer needed. It usually closes in a couple of days after birth. If the vessel doesn't close, it is referred to as a PDA. PDA leads to abnormal blood flow between the aorta and pulmonary artery, two major blood vessels that carry blood from the heart. Pericardial Effusion Pre-Ejection Period The period between ventricular contraction the semilunar valves blood ejection into commences. when the occurs and open and the aorta Pulmonary Hypertension Pulmonic Regurgitation Pulmonic Stenosis Pulmonary Valve (or vein) Premature Ventricular Contraction Peripheral Vascular Disease Pulsed Wave Doppler Flow (Q) Right Atrium Right Atrial Pressure Right Coronary Artery Right Upper Sternal Border Right Ventricle Right Ventricular Hypertrophy Right Ventricular Outflow Tract Right Ventricular Systolic Pressure Sinoatrial Systolic Anterior Motion (SAM) • Systolic anterior motion (SAM) of the mitral valve (MV) can be a lifethreatening condition. The SAM can result in severe left ventricular outflow tract obstruction and/or mitral regurgitation and is associated with an up to 20% risk of sudden death. • Systolic anterior motion (SAM) describes the dynamic movement of the mitral valve (MV) during systole anteriorly towards the left ventricular outflow tract (LVOT). Short Axis View Bicuspid Aortic Valve Subacute Bacterial Endocarditis • Subacute Bacterial Endocarditis (SBE) is a bacterial infection that produces growths on the endocardium (the cells lining the inside of the heart). Subacute bacterial endocarditis usually (but not always) is caused by a type of bacteria; it occurs on damaged valves, and, if untreated, can become fatal within six weeks to a year. Systolic Blood Pressure Stroke Volume Superior Vena Cava Transposition of the Great Vessels Tricuspid Regurgitation Tricuspid Stenosis Tricuspid Valve Umbilical Artery • The umbilical vein is a vein present during fetal development that carries oxygenated blood from the placenta to the growing fetus. Umbilical Vein Ventricular Septal Defect Wolf-Parkinson-White Syndrome • WPW is caused by the presence of an abnormal accessory electrical conduction pathway between the atria and the ventricles. • Electrical signals traveling down this abnormal pathway (known as the bundle of Kent) may stimulate the ventricles to contract prematurely, resulting in a unique type of supraventricular tachycardia referred to as an atrioventricular reciprocating tachycardia. Most cardiac output is reduced because of: Restrictive physiology (Hypertrophy of the ventricles) In the typical 4 chamber view, why can an inter-atrial septum appear so fat? AMYLOID DEPOSITS • Color flow Doppler can demonstrate… – Normal tricuspid regurgitation – Moderate tricuspid regurgitation – Mild tricuspid regurgitation – Hint: Moderate regurgitation on Doppler takes up more than one-half of the chamber Prosthetic mitral valves • Tilting disk • Ball and cage • St. Jude The ball and cage is not put in anymore. (Makes too much noise) They last for 30-40 years, though. Wire on the image? Probably a pace-maker wire Q: One of the best features of the ball and cage prosthetic valve is: A. B. C. D. A. Durability Low gradient No need for blood thinners Low chance of infection • Sometimes, the degree of mitral regurg is indeterminate because of: • Noise • Artifact • Reverberation • An asymptomatic 36 y/o male has which common associated defect? • ASD Expect to see a wide variety of Pathology Dilated CM Carcinoid Amyloid CM Ao Dissection Tetralogy of Fallot Ischemic CM Apical HCM Effusions Ebstein’s Marfan 2 HOCM Flail MV VSD Non Compacted LV Pseudoaneurysm MV vege (TEE) Stress Cases Pulmonary HTN Bicuspid Ao LA myxoma (TEE) PDA MVR – Ball/cage RV Vol. overload Sub Ao Membrane Cleft MV Finished with lecture one NEXT: ANATOMY REVIEW