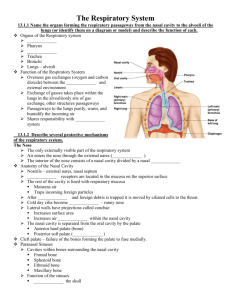
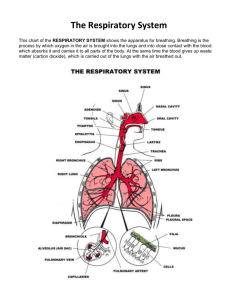
The Respiratory System
advertisement

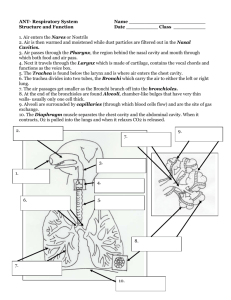
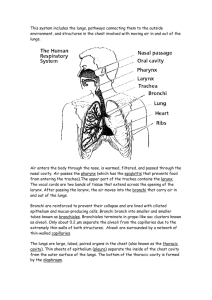
Chapter 13 Nose Pharynx Larynx Trachea Bronchi Lungs—alveoli Figure 13.1 Gas exchanges between the blood and external environment • Occurs in the alveoli of the lungs Passageways to the lungs conduct, purify, humidify, and warm the incoming air Only externally visible part of the respiratory system Air enters the nose through the external nostrils (nares) Interior of the nose consists of a nasal cavity divided by a nasal septum Figure 13.2 Olfactory receptors are located in the mucosa on the superior surface The rest of the cavity is lined with respiratory mucosa that • Moisten air • Trap incoming foreign particles In cold weather, cilia become “sluggish” and mucus tends to accumulate Lateral walls have projections called conchae • Increase surface area • Increase air turbulence within the nasal cavity – deflects foreign particles mucus-coated surfaces so they can’t enter lungs The nasal cavity is separated from the oral cavity by the palate • Anterior hard palate (bone) • Posterior soft palate (muscle) Bones of hard palate do not fuse properly difficulty in • breathing • chewing • speaking Causes, incidence, and risk factors • genetics, drugs, viruses, or other toxins can all cause such birth defects • may occur along with other syndromes or birth defects • risk factors include a family history of cleft lip or palate and other birth defect; ~ 1/ 2,500 people Symptoms • ≥ 1of these conditions @birth • small notch in the lip • complete split in the lip that goes all the way to the base of the nose • one or both sides of the roof of the mouth • may go the full length of the palate Cavities within bones surrounding the nasal cavity are called sinuses Sinuses are located in the following bones • Frontal bone • Sphenoid bone • Ethmoid bone • Maxillary bone Lighten skull Act as resonance chambers for speech Produce mucus • drains nasal cavity • suctioning effect from nose blowing will drain sinuses Nasolacrimal also ducts drain nasal cavity Sinuses are not fully developed until after age twelve. When people speak of sinus infections, they are most frequently referring to the maxillary and frontal sinuses. Figure 13.2 When the sinus openings become blocked or too much mucus builds up, bacteria and other germs can grow more easily. Sinusitis can occur from one of these conditions: • cilia in the sinuses - help move mucus out - do not work properly • colds and allergies: too much mucus , blockage of sinus openings • deviated nasal septum, nasal bone spur, or nasal polyps may block the opening of the sinuses. Sinusitis can be: • acute -- symptoms last up to 4 weeks; caused by bacterial infection in sinuses that results from URI • sub-acute -- symptoms last 4 - 12 weeks • chronic -- symptoms last 3 months or longer; long-term swelling/inflammation of the sinuses; caused by bacteria/fungus Muscular passage from nasal cavity to larynx (~13 cm.) Three regions of the pharynx • Nasopharynx—superior region behind nasal cavity • Oropharynx—middle region behind mouth • Laryngopharynx—inferior region attached to larynx The oropharynx and laryngopharynx are common passageways for air and food Pharyngotympanic tubes open into the nasopharynx Tonsils of the pharynx • Pharyngeal tonsil (adenoids) are located in the nasopharynx • Palatine tonsils are located in the oropharynx • Lingual tonsils are found at the base of the tongue Figure 13.2 Causes, incidence, and risk factors • strep throat • tonsils may become so overwhelmed by bacterial/viral infection that they swell and become inflamed • infection may also be present in throat and areas around it, causing inflammation of pharynx tube runs from middle ear back of throat Eustachian • drains fluid that is normally made in the middle ear • when blocked, fluid can build up • bacteria/viruses multiply infection (acute otitis media) Chronic ear infection may be caused by an acute ear infection that does not clear completely, or repeated ear infections • fluid in middle ear may become very thick • sometimes, tympanic membrane may stick to bones in middle ear Inferior to pharynx Routes air and food into proper channels Plays a role in speech Made of eight rigid hyaline cartilages and a spoon-shaped flap of elastic cartilage (epiglottis) Thyroid cartilage • largest of the hyaline cartilages • protrudes anteriorly (Adam’s apple) Epiglottis • protects superior opening of larynx • routes food to esophagus, air toward trachea • when swallowing, epiglottis rises and forms lid over the opening of the larynx • cough reflex is activated when anything other than air enters trachea; doesn’t work when unconscious Vocal folds (true vocal cords) • Vibrate with expelled air to create sound (speech) Glottis—opening between vocal cords In the past, thought to be caused by psychological problem Now - problem in brain/nervous system • vocal cord muscles spasm, causing the vocal cords to get too close or too far apart while people with the condition are using their voice Usually occurs ages 30 – 51 Women more likely to be affected than men Figure 13.2 4” tube - connects larynx w/bronchi Reinforced w/C-shaped hyaline cartilage Lined w/ciliated mucosa • Beat continuously in opposite direction of incoming air • Expel mucus loaded w/dust & other debris away from lungs Open part @ back allows expansion of esophagus Solid part @front supports trachea walls patent (open) despite pressure changes associated w/breathing If repeated attempts do not free airway, emergency cut in windpipe (tracheostomy or cricothyrotomy) may be necessary Huge amounts of mucus form due to tracheal irritation – must be suctioned Figure 13.3a Figure 13.3b Inhibits ciliary action; ultimately destroys cilia Coughing is only method of preventing mucus from accumulating in lungs Smokers should avoid cough suppressants Formed by division of the trachea Enters the lung at the hilum (medial depression) Right bronchus is wider, shorter, and straighter than left (more common site for object to become lodged) Bronchi subdivide into smaller and smaller branches * Air entering bronchi is warm, clean damp Figure 13.1 Figure 13.4b Occupy most of the thoracic cavity • Heart occupies central portion called mediastinum Apex is near the clavicle (superior portion) Base rests on the diaphragm (inferior portion) Each lung is divided into lobes by fissures • Left lung—two lobes • Right lung—three lobes Figure 13.4a Figure 13.4b Serosa covers outer surface of lungs • Pulmonary (visceral) pleura covers lung surface • Parietal pleura lines walls of thoracic cavity Pleural fluid fills area between layers of pleura to allow gliding These two pleural layers resist being pulled apart Figure 13.4a Symptoms • chest pain that most likely occurs when coughing or taking a deep breath in or out • some feel pain in shoulder • deep breathing, coughing, chest movements makes pain worse Pleurisy can cause fluid to collect inside chest cavity • • • • cyanosis coughing shortness of breath tachypnea (rapid breathing) Signs and tests • normally smooth pleura become rough • rub together with each breath • may produce a rough, grating sound called a "friction rub" • health care professional can hear this with stethoscope or by placing an ear against chest All but the smallest of these passageways have reinforcing cartilage in their walls • Primary bronchi • Secondary bronchi • Tertiary bronchi • Bronchioles • Terminal bronchioles conducting zone structures Figure 13.5a Structures • Respiratory bronchioles • Alveolar ducts • Alveolar sacs respiratory zone • Alveoli (air sacs) Site of gas exchange = alveoli only Figure 13.5a Respiratory membrane = alveolar walls + capillary walls + their fused basement membranes + occasional elastic membranes Thin squamous epithelial layer lines alveolar walls Alveolar pores connect neighboring air sacs • Provide alternative air pathway if there’s mucus blockage, etc Pulmonary capillaries cover external surfaces of alveoli On one side of the membrane is air and on the other side is blood flowing past Figure 13.6 (1 of 2) Figure 13.6 (2 of 2) Gas crosses the respiratory membrane by diffusion • Oxygen enters the blood • Carbon dioxide enters the alveoli Alveolar macrophages (“dust cells”) add protection by picking up bacteria, carbon particles, and other debris Surfactant (a lipid molecule) coats gasexposed alveolar surfaces (more later) Pulmonary ventilation—moving air in and out of the lungs (commonly called breathing) External respiration—gas exchange between pulmonary blood and alveoli • Oxygen is loaded into the blood • Carbon dioxide is unloaded from the blood Figure 13.6 (2 of 2) Respiratory gas transport—transport of oxygen and carbon dioxide via the bloodstream Internal respiration—gas exchange between blood and tissue cells in systemic capillaries Completely mechanical process that depends on volume changes in the thoracic cavity Volume changes lead to pressure changes, which lead to the flow of gases to equalize pressure Two phases • Inspiration = inhalation flow of air into lungs • Expiration = exhalation air leaving lungs Diaphragm and external intercostal muscles contract The size of the thoracic cavity increases External air is pulled into the lungs due to • Increase in intrapulmonary volume • Decrease in gas pressure Figure 13.7a Figure 13.8 Largely a passive process which depends on natural lung elasticity As muscles relax, air is pushed out of the lungs due to • Decrease in intrapulmonary volume • Increase in gas pressure Forced expiration can occur mostly by contracting internal intercostal muscles to depress the rib cage Figure 13.7b Figure 13.8 Normal pressure within the pleural space is always negative (intrapleural pressure) Differences in lung and pleural space pressures keep lungs from collapsing Can be caused by reflexes or voluntary actions Examples: • Cough and sneeze—clears lungs of debris • Crying—emotionally induced mechanism • Laughing—similar to crying • Hiccup—sudden inspirations • Yawn—very deep inspiration Table 13.1 Normal breathing moves about 500 mL of air with each breath • This respiratory volume is tidal volume (TV) Many factors that affect respiratory capacity • A person’s size • Sex • Age • Physical condition Inspiratory reserve volume (IRV) • Amount of air that can be taken in forcibly over the tidal volume • Usually between 2100 and 3200 mL Expiratory reserve volume (ERV) • Amount of air that can be forcibly exhaled • Approximately 1200 mL Residual volume • Air remaining in lung after expiration • About 1200 ml Vital capacity • The total amount of exchangeable air • Vital capacity = TV + IRV + ERV • Dead space volume Air that remains in conducting zone and never reaches alveoli About 150 mL Functional volume • Air that actually reaches the respiratory zone • Usually about 350 mL Respiratory capacities are measured with a spirometer Figure 13.9