Analgésicos y coadyuvantes en la enfermedad
Analgesia en pacientes con
ERC
Francisco José de la Prada Alvarez
Servicio de Nefrología
Hospital Son Dureta
2
3
M01ANTIINFLAMATORIOS Y ANTIRREUMÁTICOS NO
ESTEROIDEOS
Ver en el grupo N02B otros analgésicos y antiinflamatorios no esteroideos disponibles en el hospital
NOMBRE
GENÉRICO
Diclofenac
Ibuprofeno
Indometacina
Isonixina
Piroxicam
PRESENTACIÓN
Amp 75 mg/3 ml
Comp 50 mg
Sup 100 mg
Jbe 100 mg/5ml
Comp 400 mg
Comp 600 mg
Sobres 200 mg
Caps 25 mg
Sup 100 mg
Sup inf 200 mg
Caps 20 mg
Comp 20 mg
VIA
IM, IV
OR
REC
OR
OR
OR
OR
OR
REC
REC
OR
OR
NOMBRE COMERCIAL
Voltaren
Dalsy jarabe
Neobrufen
Inacid, Artrinovo
Nyxin
Sasulen, Feldene 20,
Vitaxicam,
Feldene flas
Nota 1: Otros medicamentos del grupo de los AINEs como por ejemplo: Ketoprofeno ( Arcental, Fastum, Orudis ), Naproxeno
(Naprosyn), Aceclofenaco ( Airtal, Falcol, Gerbin ), Fenbufeno ( Cincopal), Flurbiprofeno ( Froben), Namebutona ( Dolsinal,, Relif ),
Tenoxicam ( Reutenox, Tilcotil ), Meloxicam (Movalis) y Tolmetin ( Artrocaptin) son medicamentos no incluidos en la Guía y se consideran equivalentes terapéuticos de los AINEs incluidos. Consultar programa de intercambio.
4
N02BAnalgésicos no narcóticos y antipiréticos
Ver en grupo M01 otros analgésicos no narcóticos y antipiréticos
NOMBRE GENÉRICO
Acetilsalicilato de lisina (1)(4)
Acido Acetilsalicílico
Ketorolaco
Metamizol (Dipirona)
(Noramidopirina)
Paracetamol
Paracetamol +Codeína
PRESENTACIÓN
Sobres 1,8 g
Vial 900 mg/5 ml
Comp 500 mg
Comp 300 mg
Comp 125 mg
Comp 10 mg
Amp 30 mg/1 ml
Amp 2000 mg/5 ml
Caps 575 mg
Sup 1 g
Sup 500 mg
Comp 500 mg
Gts 100 mg/ml (2)
Sup 150 mg
Sup 250 mg
Vial 1g/100ml
Comp 300mg +15mg
Comp 650 mg + 30 mg
Com
OR
IM,IV
OR
OR
OR
OR
OR
REC
REC
IV
OR
OR
OR
IV. IM
IV, IM, OR
OR
REC
REC
NOMBRE COMERCIAL
Inyesprin oral forte
Inyesprin iny(4)
Ácido Acetilsalicilíco, Adiro, Aspirina
Aspirina infantil
Droal, Toradol
Nolotil, Lasain
Termalgin, Dolgesic, Gelocatil (650 mg)
Apiretal
Febrectal Lactante
Melabon Infantil
Perfalgan
Termalgin Codeína;
Gelocatil Codeina
Nota 1: 1,8 g de Acetilsalicilato de lisina=1g de Acido Acetil Salicílico.
Nota 2: gota=4 mg
Nota 3: Propacetamol es un precursor del Paracetamol. Propacetamol 1 g libera
Paracetamol 500 mg.
5
Opioides
Los opiodes agonistas son aquellos que al fijarse al receptor mu dan lugar a una respuesta farmacológica, que en este caso es la eliminación del dolor.
6
Opioides
Los opiodes antagonistas son aquellos que también se unen al receptor mu, pero ello no va seguido de una respuesta farmacológica, es decir, en este caso no se produciría analgesia.
7
Opioides
Existe otro tipo de opioides denominados agonistasantagonistas , que son capaces de actuar como agonistas sobre un tipo de receptores y como antagonistas sobre otro tipo, por lo que producen respuestas imprevisibles.
En pacientes que reciben agonistas puros, los agonistas-antagonistas pueden precipitar reacciones de abstinencia.
8
Agonistas puros
Semivida corta Semivida larga
Morfina
Petidina
Para dolor moderado-severo
Metanol
Levorfanol
Heroina
Fentanilo
Sulfentanilo
Tramadol
Oxicodona
Oximorfona
Para dolor ligero-moderado
Codeina
Dihidrocodeina
Dextropropoxifeno
Tramadol
Oxicodona
9
Semivida corta
Agonistas-
Antagonistas
Agonistas parciales
Pentazosina
Nalbufina
Meperidina
Buprenorfina
Semivida larga
Butorfanol
Dezocina
10
Tratamientos de rescate potenciales para el dolor intercurrente o irruptivo en pacientes con cancer
Opioides utilizados para el dolor crónico de base:
Agonistas puros preferentemente en formas de liberación retardada
– Morfina de liberación lenta
– Fentanilo via transdermica
Tratamiento de rescate: Agonistas puros en forma de liberación rápida o vias de absorción rápida:
– Morfina por via parenteral.
– Fentanilo por via transmucosa oral.
11
Tratamientos de rescate potenciales para el dolor intercurrente o irruptivo en pacientes con cancer
Opioides utilizados para el dolor crónico de base:
Agonistas parciales:
– Buprenorfina de liberación transdermica.
Tratamiento de rescate:
– Agonistas parciales : buprenorfina sublingual .
– Agonistas puros :
Morfina por via parenteral.
Fentanilo por via transmucosa oral.
12
DOSIS EQUIANALGESICAS ENTRE LOS DISTINTOS OPIOIDES
ADMINSTRADOS POR VIA ORAL
Morfina
Meperidina
30-60 mg
300 mg
Metadona
Tramadol
Codeina
15-20 mg
300-600 mg
400 mg
Dihidrocodeina
Hidromorfona
Levorfanol
Oxicodona
240 mg
7,5 mg
4 mg
30 mg
13
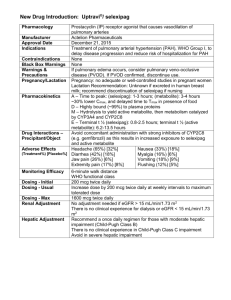
Equivalent opioid doses
Drug
Morphine sulfate parenteral
Time to onset
(minutes)
Morphine sulfate oral (MSIR, Roxanol) 15 to 60
Morphine sulfate controlled release
(MS contin, Oramorph)
Codeine 10 to 30
Oxycodone (Percocet, Percodan, Tylox) 15 to 30
15 to 30 Oxycodone controlled release
(Oxycontin)
Hydromorphone (Dilaudid)
Levorphanol (Levodromoran)
15 to 30
30 to 90
Meperidine (Demerol)
Methadone (Dolophine)
10 to 45
30 to 60
Oral dose
(mg)
Parenteral dose (mg)
10 q4 hr
30 q4 hr
90 q12 hr not available
200 q4 hr
15 to 20 q4 hr
45 to 60 q12 hr
8 q4 hr
4 q6 to q8 hr
300 q2 to q3 hr
20* q6 to q12 hr
100 to 120 q4 hr not available not available
1.5-3.0 q4 hr
2 q6 to q8 hr
100 q2 to q3 hr
10 q6 hr
* A dose ratio of 1:4 (1 mg of oral methadone = 4 mg of oral morphine) is used for patients receiving less than 90 mg of morphine. Patients receiving 90 to 300 mg/day receive methadone at a ratio of 1:8. Finally, a ratio of 1:12 is used for patients receiving morphine doses greater than 300 mg/day.
14
Opioid Analgesics - Initial Oral Dosing Commonly Used for
Severe Pain
Buprenorphine:
Equianalgesic Dose
– Oral: n/a
– Parenteral: 0.4 mg
– Initial Oral Dose
– Children: n/a
– Adults: n/a
Butorphanol:
Equianalgesic Dose
– Oral: n/a
– Parenteral: 2 mg
– Initial Oral Dose
– Children: n/a
– Adults: n/a
Levorphanol:
Equianalgesic Dose
– Oral: Acute: 4 mg; Chronic: 1 mg
– Parenteral: Acute: 2 mg;
Chronic: 1 mg
– Initial Oral Dose
– Children: 0.04 mg/kg
– Adults: 2-4 mg/kg
Meperidine:
Equianalgesic Dose
– Oral: 300 mg
– Parenteral: 75 mg
–
Initial Oral Dose
– Children: Not recommended
– Adults: Not recommended
15
Opioid Analgesics - Initial Oral Dosing Commonly Used for
Severe Pain
Hydromorphone:
Equianalgesic Dose
– Oral: 7.5 mg
– Parenteral: 1.5 mg
– Initial Oral Dose
– Children: 0.06 mg/kg
– Adults: 4-8 mg
Methadone:
Equianalgesic Dose
– Oral: 10 mg
– Parenteral: 5 mg
– Initial Oral Dose
– Children: 0.2 mg/kg
– Adults: 5-10 mg
Morphine:
Equianalgesic Dose
– Oral: 30 mg
– Parenteral: 10 mg
– Initial Oral Dose
– Children: 0.3 mg/kg
– Adults: 15-30 mg
Nalbuphine:
Equianalgesic Dose
– Oral: n/a
– Parenteral: 10 mg
– Initial Oral Dose
– Children: n/a
– Adults: n/a
16
Opioid Analgesics - Initial Oral Dosing Commonly Used for
Severe Pain
Pentazocine:
Equianalgesic Dose
– Oral: 50 mg
– Parenteral: 30 mg
– Initial Oral Dose
– Children: n/a
– Adults: n/a
Oxymorphone:
Equianalgesic Dose
– Oral: 1 mg
– Parenteral: n/a
– Initial Oral Dose
– Children: n/a
– Adults: n/a
From "Principles of Analgesic Use in the Treatment of Acute Pain and
Cancer Pain,"Am Pain Soc, Fifth
Ed.
Oxycodone:
Equianalgesic Dose
– Oral: 20 mg
– Parenteral: n/a
– Initial Oral Dose
– Children: 0.3 mg/kg
– Adults: 10-20 mg
17
18
N02AAnalgésicos narcóticos (Opioides)
NOMBRE GENÉRICO
Buprenorfina
Codeína
Dihidrocodeína (Hidrocodona)
Fentanilo (2)
Metadona
Morfina cloruro
PRESENTACIÓN
Comp 0,2 mg
Amp 0,3 mg/1 ml
VIA
SL
IM, IV
NOMBRE COMERCIAL
Buprex CE
Comp 28 mg OR Codeisan
Comp 60 mg
Parche 2,5 mg (3)
Parche 5 mg (3)
Parche 10 mg (3)
Amp 10 mg/1 ml
Comp 5 mg
Comp 40 mg
Amp 10 mg/1 ml
(sin conservantes)
Vial 400 mg/20 ml
(vial multidosis, sin conservantes)
Amp 10 ml.
OR
TOP
TOP
TOP
SC, IM
OR
OR
SC, IV, IM
SC
IV, IM
IV, IM
Contugesic
Durogesic 25
Durogesic 50
Durogesic 100
Metasedin CE
Cloruro Mórfico Braun 1 % CE
Morfina Braun 2 % s/c CE
Morfina Braun 4 % s/c CE
Morfina clorhidrato
Morfina sulfato
Morfina sulfato retard
Petidina (Meperidina)
Tramadol
Jbe 10 mg/ml
Comp 10 mg
Comp 20 mg
Comp 10 mg
Comp 30 mg
Comp 60 mg
Comp 100 mg
Amp 100 mg/2 ml
Caps 50 mg
Comp retard 200 mg
Comp retard 300 mg
Amp 100 mg/2 m
OR
OR
OR
OR
OR
OR
OR
SC, IM, IV
OR
OR
OR
SC, IM, IV
Brompton FM CE
Sevredol CE (1)
MST Continus CE
Dolantina CE
Adolonta, Tralgiol
Zytram
CE: Control de estupefacientes.
Nota 1: Comprimidos ranurados.
Nota 2: Uso restringido para tratamiento del dolor crónico.
Nota 3: Los parches de 2,5, 5 y 10 mg liberan respectivamente 25, 50 y 100 mcg/h durante 72 h.
19
N02BAnalgésicos no narcóticos y antipiréticos
Ver en grupo M01 otros analgésicos no narcóticos y antipiréticos
NOMBRE GENÉRICO
Acetilsalicilato de lisina (1)(4)
Acido Acetilsalicílico
Ketorolaco
Metamizol (Dipirona)
(Noramidopirina)
PRESENTACIÓN
Sobres 1,8 g
Vial 900 mg/5 ml
Comp 500 mg
Comp 300 mg
Comp 125 mg
Comp 10 mg
Amp 30 mg/1 ml
Amp 2000 mg/5 ml
Caps 575 mg
Sup 1 g
Sup 500 mg
Paracetamol Comp 500 mg
Gts 100 mg/ml (2)
Sup 150 mg
Sup 250 mg
Vial 1g/100ml
Paracetamol +Codeína
Comp 300mg +15mg
Comp 650 mg + 30 mg
Com
OR
IM,IV
OR
OR
OR
OR
IV. IM
IV, IM, OR
OR
REC
REC
OR
OR
REC
REC
IV
OR
OR
NOMBRE COMERCIAL
Inyesprin oral forte
Inyesprin iny(4)
Ácido Acetilsalicilíco, Adiro, Aspirina
Aspirina infantil
Droal, Toradol
Nolotil, Lasain
Termalgin, Dolgesic, Gelocatil (650 mg)
Apiretal
Febrectal Lactante
Melabon Infantil
Perfalgan
Termalgin Codeína;
Gelocatil Codeina
Nota 1: 1,8 g de Acetilsalicilato de lisina=1g de Acido Acetil Salicílico.
Nota 2: gota=4 mg
Nota 3: Propacetamol es un precursor del Paracetamol. Propacetamol 1 g libera
Paracetamol 500 mg.
20
Codeina
Opioide estructuralmente relacionada con la morfina.
Es un alcaloide presente en la
Papaver somniferum.
Estructuralmente es la metilmorfina y existen estudios que sugieren que sus efectos son, al menos en parte, consecuencia de la desmetilación en el organismo a morfina que sería el principio activo.
Sus propiedades analgésicas son similares a las de la morfina pero su potencia es sólo un 12%.
La codeína se comporta como un agonista opioide puro de los receptores Mu y, por esta razón, su mecanismo de acción y los efectos derivados de este son, en principio, similares a los de la morfina
21
Codeina
Los opioides que actúan sobre el receptor mu aminoran la transmisión en la médula espinal, mediante una inhibición relacionada con la dosis, de la actividad del tracto neural.
En los ganglios basales del cerebro, los opioides activan el sistema inhibidor descendente, que limita la transmisión del dolor a la altura de la médula espinal.
Los opioides también producen cambios en el cerebro, lo que provoca una alteración de las respuestas emocionales y aminoran en gran medida la percepción del dolor.
22
Properties of opioid receptors
Mu
Mu1
Supraspinal analgesia
Bradycardia
Sedation
Mu2
Respiratory depression
Euphoria
Physical dependence
Delta
Kappa
Spinal analgesia
Respiratory depression
Spinal Analgesia
Respiratory depression
Sedation
Sigma
Dysphoria, delirium
Hallucinations
Tachycardia, hypertension
23
Codeina
DOSING: ADULTS or ELDERLY
Doses >1.5 mg/kg body weight are not recommended.
Pain management (analgesic):
Oral, regular release: 30 mg every 4-6 hours as needed ; patients with prior opiate exposure may require higher initial doses. Usual range: 15-120 mg every 4-6 hours as needed
Oral, controlled release formulation (Codeine Contin®, not available in
U.S.): 50-300 mg every 12 hours.
I.M., SubQ: 30 mg every 4-6 hours as needed; patients with prior opiate exposure may require higher initial doses. Usual range: 15-120 mg every 4-6 hours as needed; more frequent dosing may be needed
Cough (antitussive): Oral (for nonproductive cough): 10-20 mg/dose every 4-6 hours as needed; maximum: 120 mg/day
24
25
Codeina
DOSING: PEDIATRIC —
Analgesic: Oral, I.M., SubQ:
– Children: 0.5-1 mg/kg/dose every 4-6 hours as needed; maximum: 60 mg/dose
Antitussive: Oral (for nonproductive cough):
– Children: 1-1.5 mg/kg/day in divided doses every 4-6 hours as needed:
– Alternative dose according to age:
2-6 years: 2.5-5 mg every 4-6 hours as needed; maximum: 30 mg/day
6-12 years: 5-10 mg every 4-6 hours as needed; maximum: 60 mg/day
26
Codeina
DOSING: HEPATIC IMPAIRMENT —
Dosing adjustment is probably necessary in hepatic insufficiency.
27
Codeina
Dosis de carga
Dosis de manteni miento
FG > 50 ml/min
FG 10-50 ml/min
FG < 10 ml/min
Dosis suplemta ria tras
HD
DPCA
100 % 75% 50%
TSCR
Descono
-cida
Desonocida
75%
Vida media de eliminación prolongada en pacientes en diálisis.
28
Codeina
ADVERSE REACTIONS SIGNIFICANT
Frequency not defined: AST/ALT increased
>10%:
Central nervous system: Somnolencia
Gastrointestinal: Estreñimiento
1% to 10%:
Cardiovascular: Tachycardia or bradycardia, hypotension
Central nervous system: Dizziness, lightheadedness, false feeling of well being, malaise, headache, restlessness, paradoxical CNS stimulation, confusion
Dermatologic: Rash, urticaria
Gastrointestinal: Dry mouth, anorexia, nausea, vomiting
Genitourinary: Urination decreased, ureteral spasm
Hepatic: LFTs increased
Local: Burning at injection site
Neuromuscular & skeletal: Weakness
Ocular: Blurred vision
Respiratory: Dyspnea
Miscellaneous: Histamine release
<1% (Limited to important or life-threatening): Convulsions, hallucinations, insomnia, mental depression, nightmares
29
Codeina
DRUG INTERACTIONS — Substrate of CYP2D6
(major), 3A4 (minor); Inhibits CYP2D6 (weak)
CYP2D6 inhibitors: May decrease the effects of codeine.
Example inhibitors include chlorpromazine, delavirdine, fluoxetine, miconazole, paroxetine, pergolide, quinidine, quinine, ritonavir, and ropinirole.
Decreased effect with cigarette smoking
Increased toxicity: CNS depressants, phenothiazines,
TCAs, other narcotic analgesics, guanabenz, MAO inhibitors, neuromuscular blockers
30
Codeina
Embarazo y Lactancia.
– Contraindicado.
31
Codeina
REFERENCE RANGE —
– Therapeutic: Not established;
– Toxic: >1.1 mcg/mL
Sobredosis:
– Symptoms include CNS and respiratory depression, gastrointestinal cramping, and constipation.
– Treatment includes naloxone 2 mg I.V
. (0.01 mg/kg for children), with repeat administration as necessary, up to a total of 10 mg.
32
Codeina
PHARMACODYNAMICS / KINETICS
Onset of action: Oral: 0.5-1 hour ; I.M.: 10-30 minutes
Peak effect: Oral: 1-1.5 hours ; I.M.: 0.5-1 hour
Duration: 4-6 hours
Absorption: Oral: Adequate
Las propiedades farmacocinéticas de la codeína le confieren una aceptable biodisponibilidad oral (50%), lo que permite su administración (casi exclusiva) por esta vía.
Distribution: Crosses placenta; enters breast milk
Protein binding: 7%
Metabolism: Hepatic to morphine (active) 10% de codeina se metaboliza a morfina .
Half-life elimination: 2.5-3.5 hours .
Su baja semivida de eliminación obliga a la administración cada 4-6 h, lo que ha llevado a la comercialización de algunos derivados, como la dihidrocodeína
, en forma de preparados de liberación sostenida , especialmente indicadas en situaciones de dolor crónico
Excretion: Urine (3% to 16% as unchanged drug, norcodeine, and free and conjugated morphine)
33
N02AAnalgésicos narcóticos (Opioides)
NOMBRE GENÉRICO
Buprenorfina
Codeína
Dihidrocodeína
(Hidrocodona)
Fentanilo (2)
PRESENTACIÓN
Comp 0,2 mg
Amp 0,3 mg/1 ml
Comp 28 mg
VIA
SL
IM, IV
OR
NOMBRE COMERCIAL
Buprex CE
Codeisan
Comp 60 mg OR Contugesic
Metadona
Morfina cloruro
Morfina clorhidrato
Morfina sulfato
Morfina sulfato retard
Petidina (Meperidina)
Tramadol
Parche 2,5 mg (3)
Parche 5 mg (3)
Parche 10 mg (3)
Amp 10 mg/1 ml
Comp 5 mg
Comp 40 mg
Amp 10 mg/1 ml
(sin conservantes)
Vial 400 mg/20 ml
(vial multidosis, sin conservantes)
Amp 10 ml.
Jbe 10 mg/ml
Comp 10 mg
Comp 20 mg
Comp 10 mg
Comp 30 mg
Comp 60 mg
Comp 100 mg
Amp 100 mg/2 ml
Caps 50 mg
Comp retard 200 mg
Comp retard 300 mg
Amp 100 mg/2 m
TOP
TOP
TOP
SC, IM
OR
OR
SC, IV, IM
SC
IV, IM
IV, IM
OR
OR
OR
OR
OR
OR
OR
SC, IM, IV
OR
OR
OR
SC, IM, IV
Durogesic 25
Durogesic 50
Durogesic 100
Metasedin CE
Cloruro Mórfico Braun 1 % CE
Morfina Braun 2 % s/c CE
Morfina Braun 4 % s/c CE
Brompton FM CE
Sevredol CE (1)
MST Continus CE
Dolantina CE
Adolonta, Tralgiol
Zytram
CE: Control de estupefacientes.
Nota 1: Comprimidos ranurados.
Nota 2: Uso restringido para tratamiento del dolor crónico.
Nota 3: Los parches de 2,5, 5 y 10 mg liberan respectivamente 25, 50 y 100 mcg/h durante 72 h.
34
35
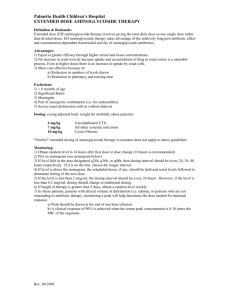
Tramadol
Análogo sintético de codeina.
Analgésico no narcótico de acción periférico y central.
36
Tramadol
Mecanismo de acción:
– Inhibición de la recaptación de NA y serotonina por las celulas nerviosas.
– Actúa sobre los receptores opioides Mu.
37
N02AAnalgésicos narcóticos (Opioides)
NOMBRE
GENÉRICO
Tramadol
PRESENTACIÓN VIA NOMBRE
COMERCIAL
Caps 50 mg
Comp retard 200 mg
Comp retard 300 mg
Amp 100 mg/2 ml
OR
OR
OR
SC,
IM,
IV
Adolonta, Tralgiol
Zytram
38
Tramadol
PRESENTACIONES:
– Adolonta amp de 100 mg en 2 ml
– Tralgiol amp de 100 mg en 2 ml
ADMINISTRACION:
– INYECCION IV DIRECTA : SI
– Administrar lentamente.
– INFUSION INTERMITENTE : SI
Diluir la dosis prescrita en 50-100 ml de SF o SG5%. Administrar en 30-60 minutos.
– INFUSION CONTINUA : SI
Diluir la dosis prescrita, ejemplo 2 amp en 500 ml de SF o SG5%. El ritmo de infusión adecuado es de
1020 gotas/min ó 30-60 ml/h que equivalen a 12-44 mg/h de Tramadol.
– INYECCION IM : SI
– INYECCION SUBCUTANEA : SI
SUEROS COMPATIBLES : SF, SG5%.
OBSERVACIONES:
– La dosificacion máxima diaria en adultos por cualquier vía es de 400 mg/día.
– También se dispone de estudios de administración vía epidural.
39
Tramadol
DOSING: ADULTS — Moderate-to-severe chronic pain: Oral:
– Caps 50 mg
50-100 mg every 4-6 hours (not to exceed 400 mg/day)
For patients not requiring rapid onset of effect, tolerability may be improved by starting dose at 25 mg/day and titrating dose by 25 mg every 3 days, until reaching 25 mg 4 times/day. Dose may then be increased by 50 mg every 3 days as tolerated, to reach dose of 50 mg 4 times/day.
– Comp retard 200 mg. Comp retard 300 mg
100 mg once daily; titrate every 5 days (maximum: 300 mg/day)
40
Tramadol
DOSING: ELDERLY — Oral: >75 years:
– Caps 50 mg
50 mg every 6 hours (not to exceed 300 mg/day
– Comp retard 200 mg. Comp retard 300 mg
100 mg once daily; titrate every 5 days (maximum:
300 mg/day). Use with great caution.
41
Tramadol
DOSING: RENAL IMPAIRMENT
– Clcr <30 mL/minute: 50 -100 mg dose every 12 hours
(maximum: 200 mg/day).
– Should not be used in patients with Clcr < 30 mL/minute.
DOSING: HEPATIC IMPAIRMENT
– Cirrhosis: Recommended dose: 50 mg every 12 hours.
– Should not be used in patients with severe (Child-
Pugh Class C) hepatic dysfunction.
42
43
Tramadol
Efectos secundarios:
>10%:
Cardiovascular: Flushing (8% to 16%)
Central nervous system: mareos (16% to
33%), headache (8% to 32%), insomnia (7% to
11%), somnolence (7% to 25%)
Dermatologic: Pruritus (6% to 12%)
Gastrointestinal: Constipation (12% to 46%), nausea (15% to 40%)
Neuromuscular & skeletal: Weakness (4% to
12%)
44
Tramadol
Efectos secundarios:
1% to 10%:
Cardiovascular: Chest pain (1% to <5%), postural hypotension (2% to 5%), vasodilation (1% to <5%)
Central nervous system: Agitation, anxiety (1% to <5%), confusion (1% to <5%), coordination impaired (1% to <5%), depression (1% to <5%), emotional lability, euphoria, hallucinations, hypoesthesia, lethargy, malaise, nervousness (1% to <5%), pain, pyrexia, restlessness
Dermatologic: Dermatitis, rash
Endocrine & metabolic: Hot flashes (2% to 9%), menopausal symptoms (1% to
<5%)
Gastrointestinal: Abdominal pain, anorexia (<6%), diarrhea (5% to 10%), dry mouth
(5% to 10%), dyspepsia, flatulence, vomiting (5% to 9%), weight loss
Genitourinary: Urinary frequency (1% to <5%), urinary retention (1% to <5%), urinary tract infection (1% to <5%)
Neuromuscular & skeletal: Arthralgia (1% to <5%), hypertonia (1% to <5%), rigors
(<4%), paresthesia (1% to <5%), spasticity (1% to <5%), tremor (1% to <5%), creatinine phosphokinase increased
Ocular: Blurred vision (1% to <5%), miosis (1% to <5%)
Respiratory: Bronchitis (1% to <5%), cough (1% to <5%), dyspnea (1% to <5%), pharyngitis (1% to <5%), rhinorrhea (1% to <5%), sinusitis (1% to <5%)
Miscellaneous: Diaphoresis (2% to 6%), flu-like syndrome (<2%)
45
Tramadol
El tramadol presenta una baja o nula capacidad para causar cuadros de farmacodependencia.
Epileptógeno en situaciones con disminución del umbral de epilepsia
(uremia , tumores cerebrales)
46
Tramadol
DRUG INTERACTIONS — Substrate of CYP2B6 (minor), 2D6 (major), 3A4 (minor)
Carbamazepine: Tramadol metabolism is increased by carbamazepine. Avoid concurrent use; increases risk of seizures.
Cyclobenzaprine: May enhance the neuroexcitatory and/or seizure-potentiating effect of tramadol.
CYP2D6 inhibitors: May decrease the effects of tramadol. Example inhibitors include chlorpromazine, delavirdine, fluoxetine, miconazole, paroxetine, pergolide, quinidine, quinine, ritonavir, and ropinirole.
Ethanol: Tramadol may enhance the CNS depressant effect of ethanol.
MAO inhibitors: May increase the neuroexcitatory effects or risk of seizures .
Examples of inhibitors include isocarboxazid, linezolid, phenelzine, selegiline, and tranylcypromine.
Naloxone: May increase the risk of seizures (if administered in tramadol overdose).
Quinidine: May increase the tramadol serum concentrations and decrease serum concentrations of M1
SSRIs: May increase the neuroexcitatory effects or risk of seizures with tramadol. Examples of SSRIs include citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, sertraline.
Serotonin modulators: May enhance the adverse/toxic effects of tramadol. The development of serotonin syndrome may occur.
Sibutramine: May enhance the serotonergic effects of tramadol. Avoid concurrent use.
Tricyclic antidepressants: May increase the risk of seizures.
47
Tramadol
Embarazo y lactancia.
– Contraindicado.
– Atraviesa la placenta.
– Aparece en la leche materna.
48
Tramadol
Rango terapéutico:
– 100-300 ng/mL
49
Tramadol
Sobredosis:
– Clínica: Depresión del SNC, depresion respiratoria, letargia, coma, miosis, convulsiones, fallo cardíaco y muerte.
– Tratamiento sintomático.
– La administración de naloxona no revierte completamente los efectos del tramadol, y puede aumentar el riesgo de convulsiones.
– No se elimina mediante Hemodiálisis.
50
Tramadol
Farmacocinética:
– Inicio de acción en 1 horas.
– Duración de acción 9 horas.
– Absorción oral rápida y completa.
– VD 2,5-3 l/kg.
– Unión aproteinas plasmáticas: 20%.
– Metabolismo: Hepatico (demethylation, glucuronidation, and sulfation)
Metabolito activo (O-desmethyl tramadol)
Vida media de eliminación: Prolongada en ancianos, daño hepático y renal (en esta última X2).
– Tramadol: 6-8 horas.(obliga a su administración varias veces al día).
– O-desmethyl tramadol: 7-9 horas.
Excreccion: Urinaria (30% como fármaco; 60% como metabolito)
51
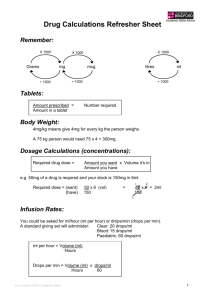
Tramadol
Dosis de carga
Dosis de manteni miento
FG > 50 ml/min
FG 10-50 ml/min
FG < 10 ml/min
Dosis suplemta ria tras
HD
DPCA TSCR
Clcr <30 mL/minute:
50
-100 mg dose every 12 hours (maximum: 200 mg/day).
Should not be used in patients with Clcr < 30 mL/minute.
52
53
Oxicodona
Agonista puro .
Se comercializa como medicamento de liberación controlada ( OxyContin
) o de liberación rápida (
OxyIR,
OxyNorm ).
– El OxyContin se presenta en comprimidos de 10, 20, 40 y 80 mg, y debido a su mecanismo de liberación lenta, es efectivo durante unas doce horas.
– Oxynorm caps. 5, 10 y 20 mg
– OXYNORM Concentrado 10 mg/ml solución oral
– OXYNORM Líquido 1 mg/ 1 ml sol.oral
54
Oxicodona
DOSING: ADULTS — Management of pain: Oral:
Regular or immediate release formulations: 2.5-5 mg every 6 hours
Controlled release:
Opioid naive (not currently on opioid): 10 mg every 12 hours
Currently on opioid/ASA or acetaminophen or NSAID combination:
1-5 tablets: 10-20 mg every 12 hours
6-9 tablets: 20-30 mg every 12 hours
10-12 tablets: 30-40 mg every 12 hours
May continue the nonopioid as a separate drug.
Currently on opioids: Use standard conversion chart to convert daily dose to oxycodone equivalent. Divide daily dose in 2 (for every
12-hour dosing) and round down to nearest dosage form.
Note: 80 mg or 160 mg tablets are for use only in opioid-tolerant patients. Special safety considerations must be addressed when converting to OxyContin® doses 160 mg every 12 hours. Dietary caution must be taken when patients are initially titrated to 160 mg tablets.
55
Oxicodona
DOSING: PEDIATRIC — Oral: Regular or immediate release formulations:
– 6-12 years: 1.25 mg every 6 hours as needed
– >12 years: 2.5 mg every 6 hours as needed
56
Oxicodona
DOSING: HEPATIC IMPAIRMENT —
Reduce dosage in patients with severe liver disease.
DOSING: RENAL IMPAIRMENT –
Se prolonga la vida media de eliminación.
Relacionado con casos de GNF fibrilar
57
Oxicodona
ADVERSE REACTIONS SIGNIFICANT
>10%:
Central nervous system: Fatigue, drowsiness, dizziness, somnolence
Dermatologic: Pruritus
Gastrointestinal: Nausea, vomiting, constipation
Neuromuscular & skeletal: Weakness
1% to 10%:
Cardiovascular: Postural hypotension
Central nervous system: Nervousness, headache, restlessness, malaise, confusion, anxiety, abnormal dreams, euphoria, thought abnormalities
Dermatologic: Rash
Gastrointestinal: Anorexia, stomach cramps, xerostomia, biliary spasm, abdominal pain, dyspepsia, gastritis
Genitourinary: Ureteral spasms, decreased urination
Local: Pain at injection site
Respiratory: Dyspnea, hiccups
Miscellaneous: Diaphoresis
<1% (Limited to important or life-threatening): Anaphylaxis, anaphylactoid reaction, dysphagia, exfoliative dermatitis, hallucinations, histamine release, hyponatremia, ileus, intracranial pressure increased, mental depression, paradoxical CNS stimulation, paralytic ileus, physical and psychological dependence, SIADH, syncope, urinary retention, urticaria, vasodilation, withdrawal syndrome (may include seizure)
Note: Deaths due to overdose have been reported due to misuse/abuse after crushing the sustained release tablets.
58
Oxicodona
CONTRAINDICATIONS —
Hypersensitivity to oxycodone or any component of the formulation;
Significant respiratory depression; hypercarbia; acute or severe bronchial asthma;
OxyContin® is also contraindicated in paralytic ileus (known or suspected); pregnancy
(prolonged use or high doses at term)
59
Oxicodona
Use with caution in the elderly, debilitated, severe hepatic or renal function.
Hemodynamic effects (hypotension, orthostasis) may be exaggerated in patients with hypovolemia, concurrent vasodilating drugs, or in patients with head injury .
Respiratory depressant effects and capacity to elevate CSF pressure may be exaggerated in presence of head injury, other intracranial lesion, or pre-existing intracranial pressure. Some preparations contain sulfites which may cause allergic reactions.
60
Oxicodona
DRUG INTERACTIONS — Substrate of
CYP2D6 (major)
CNS depressants, MAO inhibitors, general anesthetics, and tricyclic antidepressants: May potentiate the effects of opiate agonists; dextroamphetamine may enhance the analgesic effect of opiate agonists
CYP2D6 inhibitors: May decrease the effects of oxycodone. Example inhibitors include chlorpromazine, delavirdine, fluoxetine, miconazole, paroxetine, pergolide, quinidine, quinine, ritonavir, and ropinirole.
61
Oxicodona
Embarazo:
– Contraindicado.
Lactancia:
– Pasa a la leche materna. Usar con precaución.
62
Oxicodona
PHARMACODYNAMICS / KINETICS
Onset of action: 10-15 minutes.
Peak effect: 0.5-1 hour
Duration: 3-6 hours;
– Controlled release: 12 hours
Metabolism: Hepatic (noroxycodona y oxymorfona)
Half-life elimination: 2-3 hours
Excretion: Urine (10% como fármaco)
63
Oxicodona
Dosis de carga
Dosis de manteni miento
FG > 50 ml/min
FG 10-50 ml/min
FG < 10 ml/min
Dosis suplemta ria tras
HD
DPCA TSCR
64
65
N02AAnalgésicos narcóticos (Opioides)
NOMBRE
GENÉRICO
PRESENTACIÓN VIA NOMBRE
COMERCIAL
Fentanilo (2) Parche 2,5 mg (3)
Parche 5 mg (3)
Parche 10 mg (3)
TOP
TOP
TOP
Durogesic 25
Durogesic 50
Durogesic 100
Actiq®: 200 mcg, 400 mcg, 600 mcg, 800 mcg, 1200 mcg, 1600 mcg
CE: Control de estupefacientes.
Nota 2: Uso restringido para tratamiento del dolor crónico.
Nota 3: Los parches de 2,5, 5 y 10 mg liberan respectivamente 25, 50 y 100 mcg/h durante 72 h.
66
Fentanilo
Mecanismo de acción: Agonistas de los tres receptores opioides.
Se caracteriza por su elevada potencia farmacológica , muy por encima de la morfina, su elevada liposolubilidad , y su escasa biodisponibilidad tras la administración oral .
Inidicaciones:
– Parche transdérmico (Duragesic®): Tratamiento del dolor crónico moderado o severo.
– Transmucosal (Actiq®): Tratamiento del dolor irruptivo. (evita el primer paso hepático)
67
Fentanilo
Chronic pain management:
– Dosis inicial 25 mcg/h si el paciente no toma morfina o toma menos de 90 mg/dia.
68
Fentanilo
Dose conversion guidelines for transdermal fentanyl 1.
Recommended Initial Duragesic® Dose Based Upon Daily Oral
Morphine Dose1
– 60-134 mg morphine oral/day = 25 mcg/hour Duragesic®
– 135-224 mg morphine oral/day = 50 mcg/hour Duragesic®
– 225-314 mg morphine oral/day = 75 mcg/hour Duragesic®
– 315-404 mg morphine oral/day = 100 mcg/hour Duragesic®
– 405-494 mg morphine oral/day = 125 mcg/hour Duragesic®
– 495-584 mg morphine oral/day = 150 mcg/hour Duragesic®
– 585-674 mg morphine oral/day = 175 mcg/hour Duragesic®
– 675-764 mg morphine oral/day = 200 mcg/hour Duragesic®
– 765-854 mg morphine oral/day = 225 mcg/hour Duragesic®
– 855-944 mg morphine oral/day = 250 mcg/hour Duragesic®
– 945-1034 mg morphine oral/day = 275 mcg/hour Duragesic®
– 1035-1124 mg morphine oral/day = 300 mcg/hour Duragesic®
69
Dosing Conversion Guidelines1,2
Morphine (I.M./I.V.):
10-22 mg/day: recommended fentanyl transdermal dose: 25 mcg/hour
23-37 mg/day: recommended fentanyl transdermal dose: 50 mcg/hour
38-52 mg/day: recommended fentanyl transdermal dose: 75 mcg/hour
53-67 mg/day: recommended fentanyl transdermal dose: 100 mcg/hour
Oxycodone (oral):
30-67 mg/day: recommended fentanyl transdermal dose: 25 mcg/hour
67.5-112 mg/day: recommended fentanyl transdermal dose: 50 mcg/hour
112.5-157 mg/day: recommended fentanyl transdermal dose: 75 mcg/hour
157.5-202 mg/day: recommended fentanyl transdermal dose: 100 mcg/hour
Oxycodone (I.M./I.V.):
15-33 mg/day: recommended fentanyl transdermal dose: 25 mcg/hour
33.1-56 mg/day: recommended fentanyl transdermal dose: 50 mcg/hour
56.1-78 mg/day: recommended fentanyl transdermal dose: 75 mcg/hour
78.1-101 mg/day: recommended fentanyl transdermal dose: 100 mcg/hour
Codeine (oral):
150-447 mg/day: recommended fentanyl transdermal dose: 25 mcg/hour
448-747 mg/day: recommended fentanyl transdermal dose: 50 mcg/hour
748-1047 mg/day: recommended fentanyl transdermal dose: 75 mcg/hour
1048-1347 mg/day: recommended fentanyl transdermal dose: 100 mcg/hour
70
Dosing Conversion Guidelines1,2
Hydromorphone (oral):
8-17 mg/day: recommended fentanyl transdermal dose: 25 mcg/hour
17.1-28 mg/day: recommended fentanyl transdermal dose: 50 mcg/hour
28.1-39 mg/day: recommended fentanyl transdermal dose: 75 mcg/hour
39.1-51 mg/day: recommended fentanyl transdermal dose: 100 mcg/hour
Hydromorphone (I.M./I.V.):
1.5-3.4 mg/day: recommended fentanyl transdermal dose: 25 mcg/hour
3.5-5.6 mg/day: recommended fentanyl transdermal dose: 50 mcg/hour
5.7-7.9 mg/day: recommended fentanyl transdermal dose: 75 mcg/hour
8-10 mg/day: recommended fentanyl transdermal dose: 100 mcg/hour
Meperidine (I.M.):
75-165 mg/day: recommended fentanyl transdermal dose: 25 mcg/hour
166-278 mg/day: recommended fentanyl transdermal dose: 50 mcg/hour
279-390 mg/day: recommended fentanyl transdermal dose: 75 mcg/hour
391-503 mg/day: recommended fentanyl transdermal dose: 100 mcg/hour
71
Dosing Conversion Guidelines1,2
Methadone (oral):
20-44 mg/day: recommended fentanyl transdermal dose: 25 mcg/hour
45-74 mg/day: recommended fentanyl transdermal dose: 50 mcg/hour
75-104 mg/day: recommended fentanyl transdermal dose: 75 mcg/hour
105-134 mg/day: recommended fentanyl transdermal dose: 100 mcg/hour
Methadone (I.M.):
10-22 mg/day: recommended fentanyl transdermal dose: 25 mcg/hour
23-37 mg/day: recommended fentanyl transdermal dose: 50 mcg/hour
38-52 mg/day: recommended fentanyl transdermal dose: 75 mcg/hour
53-67 mg/day: recommended fentanyl transdermal dose: 100 mcg/hour
1The table should NOT be used to convert from transdermal fentanyl (eg,
Duragesic®) to other opioid analgesics. Rather, following removal of the patch, titrate the dose of the new opioid until adequate analgesia is achieved.
72
Fentanilo
Breakthrough cancer pain: Transmucosal:
Actiq® dosing should be individually titrated to provide adequate analgesia with minimal side effects. For patients who are tolerant to and currently receiving opioid therapy for persistent cancer pain. Initial starting dose: 200 mcg ; the second dose may be started 15 minutes after completion of the first dose. Consumption should be limited to 4 units/day or less . Patients needing more than 4 units/day should have the dose of their long-term opioid re-evaluated.
73
Fentanilo
DOSING: PEDIATRIC
– Breakthrough cancer pain: Children 16 years:
Transmucosal: Refer to adult dosing.
– Chronic pain management: Children 2 years (opioidtolerant patients): Transdermal patch: Refer to adult dosing.
74
Fentanilo
DOSING: ELDERLY —
– Elderly have been found to be twice as sensitive as younger patients to the effects of fentanyl .
– A wide range of doses may be used. When choosing a dose, take into consideration the following patient factors: age, weight, physical status, underlying disease states, other drugs used, type of anesthesia used, and the surgical procedure to be performed.
– Transmucosal: Dose should be reduced to 2.5-5 mcg/kg . Suck on lozenge vigorously approximately
20-40 minutes before the start of procedure.
75
Fentanilo
Transdermal patch (eg, Duragesic®):
– Apply to nonirritated and nonirradiated skin , such as chest, back, flank, or upper arm.
– Do not shave skin; hair at application site should be clipped .
– Prior to application, clean site with clear water and allow to dry completely.
– Do not use damaged or cut patches ; a rapid release of fentanyl and increased systemic absorption may occur. Firmly press in place and hold for 30 seconds.
– Change patch every 72 hours.
– Do not use soap, alcohol, or other solvents to remove transdermal gel if it accidentally touches skin; use copious amounts of water.
– Avoid exposing application site to external heat sources (eg, heating pad, electric blanket, heat lamp, hot tub).
76
Fentanilo
Transmucosal:
Foil overwrap should be removed just prior to administration.
Place the unit in mouth and allow it to dissolve. Do not chew . Actiq® units may be moved from one side of the mouth to the other.
The unit should be consumed over a period of 15 minutes . Unit should be removed after it is consumed or if patient has achieved an adequate response and/or shows signs of respiratory depression.
For patients who have received transmucosal product within 6-12 hours, it is recommended that if other narcotics are required, they should be used at starting doses 1/4 to 1/3 those usually recommended.
77
Fentanilo
ADVERSE REACTIONS SIGNIFICANT
>10%:
Cardiovascular: Hypotension, bradycardia
Central nervous system: CNS depression, confusion, drowsiness, sedation
Gastrointestinal: Nausea, vomiting, constipation, xerostomia
Local: Application-site reaction (iontophoretic system
14%)
Neuromuscular & skeletal: Chest wall rigidity (high dose
I.V.), weakness
Ocular: Miosis
Respiratory: Respiratory depression
Miscellaneous: Diaphoresis
78
Fentanilo
ADVERSE REACTIONS SIGNIFICANT
1% to 10%:
Cardiovascular: Cardiac arrhythmia, edema, orthostatic hypotension, hypertension, syncope, tachycardia
Central nervous system: Abnormal dreams, abnormal thinking, agitation, amnesia, anxiety, dizziness, euphoria, fatigue, fever, hallucinations, headache, insomnia, nervousness, paranoid reaction
Dermatologic: Erythema, papules, pruritus (iontophoretic system 6%), rash
Gastrointestinal: Abdominal pain, anorexia, biliary tract spasm, diarrhea, dyspepsia, flatulence, ileus
Genitourinary: Urinary retention (iontophoretic transdermal system 3%)
Hematologic: Anemia
Neuromuscular & skeletal: Abnormal coordination, abnormal gait, back pain, paresthesia, rigors, tremor
Respiratory: Apnea, bronchitis, dyspnea, hemoptysis, hypoxia, pharyngitis, rhinitis, sinusitis, upper respiratory infection
Miscellaneous: Hiccups, flu-like syndrome, speech disorder
<1% (Limited to important or life-threatening): Amblyopia, anorgasmia, aphasia, bradycardia, bronchospasm, circulatory depression, CNS excitation or delirium, convulsions, dental caries
(Actiq®), depersonalization, dysesthesia, ejaculatory difficulty, exfoliative dermatitis, gum line erosion (Actiq®), hyper-/hypotonia, laryngospasm, paradoxical dizziness, physical and psychological dependence with prolonged use, stertorous breathing, stupor, tachycardia, tooth loss (Actiq®), urinary tract spasm, urticaria, vertigo
79
Fentanilo
CONTRAINDICATIONS — Hypersensitivity to fentanyl or any component of the formulation; increased intracranial pressure; severe respiratory disease or depression including acute asthma
(unless patient is mechanically ventilated); paralytic ileus; severe liver or renal insufficiency ; pregnancy (prolonged use or high doses near term)
Transmucosal lozenges (Actiq®) or transdermal patches (eg,
Duragesic®) must not be used in patients who are not opioid tolerant. Patients are considered opioid-tolerant if they are taking at least 60 mg morphine/day, 30 mg oral oxycodone/day, 8 mg oral hydromorphone/day, 25 mcg transdermal fentanyl/hour, or an equivalent dose of another opioid for 1 week.
Transdermal patches are not for use in acute pain, mild pain, intermittent pain, or postoperative pain management.
80
Fentanilo
Transdermal patches (eg, Duragesic®):
Serious or life-threatening hypoventilation may occur , even in opioid-tolerant patients.
Serum fentanyl concentrations may increase approximately onethird for patients with a body temperature of 40ºC secondary to a temperature-dependent increase in fentanyl release from the patch and increased skin permeability .
Avoid exposure of application site to direct external heat sources.
Patients who experience adverse reactions should be monitored for at least 24 hours after removal of the patch. Transdermal patch does not contain any metal-based compounds; the printed ink used to indicate strength on the outer surface of the patch does contain titanium dioxide but the amount is minimal; adverse events have not been reported while wearing during an MRI.
Safety and efficacy of transdermal patch have been limited to children 2 years of age who are opioid tolerant.
81
Fentanilo
Actiq®:
For patients who have received transmucosal product within 6-12 hours, it is recommended that if other narcotics are required, they should be used at starting doses 1/4 to 1/3 those usually recommended.
Actiq® preparations contain an amount of medication that can be fatal to children . Keep all units out of the reach of children and discard any open units properly. Patients and caregivers should be counseled on the dangers to children including the risk of exposure to partially-consumed units. Safety and efficacy have not been established in children <16 years of age.
82
Fentanilo
DRUG INTERACTIONS
— Substrate of CYP3A4 (major); Inhibits CYP3A4 (weak)
Antipsychotic agents (phenothiazines): May enhance the hypotensive effect of analgesics (narcotic).
CNS depressants : Increased sedation with CNS depressants.;
CYP3A4 inhibitors: May increase the levels/effects of fentanyl. Potentially fatal respiratory depression may occur when a potent inhibitor is used in a patient receiving chronic fentanyl (eg, transdermal patch). Example inhibitors include azole antifungals, clarithromycin, diclofenac, doxycycline, erythromycin, imatinib, isoniazid, nefazodone, nicardipine, propofol, protease inhibitors, quinidine, telithromycin, and verapamil.
MAO inhibitors: Not recommended to use Actiq® within 14 days . Severe and unpredictable potentiation by MAO inhibitors has been reported with opioid analgesics.
Pegvisomant: Analgesics (narcotic) may diminish the therapeutic effect of pegvisomant.
Protease inhibitors: May decrease the metabolism, via CYP isoenzymes, of fentanyl.
Selective serotonin reuptake inhibitors (SSRIs): Analgesics (narcotic) may enhance the serotonergic effect of SSRIs. This may cause serotonin syndrome.
Sibutramine: Fentanyl may enhance the serotonergic effect of sibutramine.
83
Fentanilo
Embarazo:
– Su uso de forma crónica puede producir dependencia en el recien nacido.
– De forma aguda cruza la placenta pero se ha utilizado de forma segura durante el trabajo del parto.
Lactancia: Pasa a la leche materna. No recomendado.
84
Fentanilo
MONITORING PARAMETERS — Control de la función respiratoria y cardiovascular,
Tensión arterial y frecuencia cardíaca.
Transdermal patch: Monitorizar a las 24 horas de la aplicación del parche.
85
Fentanilo
Sobredosis:
Síntomas: depresión del SNC, depresión respiratoria, miosis.
Tratamiento:
– De soporte.
– Naloxone, 2 mg I.V
. with repeat administration as necessary up to a total of 10 mg, can also be used to reverse toxic effects of the opiate.
Los pacientes que presentan reacciones adversas durante el uso del parche transdérmico deben ser monitorizados durante
24 horas tras la retirada del parche .
86
Fentanilo
Farmacocinética:
Onset of action:
– Transmucosal: 5-15 minutes
– Peak effect: Transmucosal: Analgesic: 20-30 minutes
– Time to peak: Transdermal patch: 24-72 hours
Absorption:
Transmucosal: Rapid, ~25% from the buccal mucosa; 75% swallowed with saliva and slowly absorbed from GI tract
Actiq® contains 2 g sugar per unit.
Distribution: Highly lipophilic, redistributes into muscle and fat
Metabolism: Hepatic, primarily via CYP3A4
Bioavailability: Transmucosal: ~50% (range: 36% to 71%)
Half-life elimination: 2-4 hours
Transdermal patch: 17 hours (half-life is influenced by absorption rate)
Transmucosal: 6.6 hours (range: 5-15 hours)
Excretion: Urine (primarily as metabolites, 10% as unchanged drug)
87
Fentanilo
Dosis de carga
Dosis de manteni miento
FG > 50 ml/min
FG 10-50 ml/min
FG < 10 ml/min
Dosis suplemta ria tras
HD
DPCA
100% 75% 50%
TSCR
No aplicable
No aplicable
No aplicable
Su aclaramiento se reduce en pacientes con ERC avanzada, pudiendo aparecer sedación prologada y depresion respiratoria en pacientes con ERC avanzada.
(sobre todo en administración parenteral).
88
89
Morfina
Alcaloide de la Papaver somniferum.
Sigue constituyendo el analgésico más potente del que se dispone para tratar todo tipo de dolores agudos y muchos de los crónicos.
Modelo de agonista puro de los receptores opioides. Actúa activando los tres receptores opioides.
90
N02AAnalgésicos narcóticos (Opioides)
NOMBRE GENÉRICO
Morfina cloruro
Morfina clorhidrato
Morfina sulfato
Morfina sulfato retard
PRESENTACIÓN
VIA
Amp 10 mg/1 ml
(sin conservantes)
Vial 400 mg/20 ml
(vial multidosis, sin conservantes)
Amp 10 ml.
SC, IV,
IM
SC
IV, IM
IV, IM
Jbe 10 mg/ml
Comp 10 mg
Comp 20 mg
Comp 10 mg
Comp 30 mg
Comp 60 mg
Comp 100 mg
OR
OR
OR
OR
OR
OR
OR
NOMBRE COMERCIAL
Cloruro Mórfico Braun 1 %
CE
Morfina Braun 2 % s/c CE
Morfina Braun 4 % s/c CE
Brompton FM CE
Sevredol CE (1)
MST Continus CE
CE: Control de estupefacientes.
Nota 1: Comprimidos ranurados.
Nota 2: Uso restringido para tratamiento del dolor crónico.
Nota 3: Los parches de 2,5, 5 y 10 mg liberan respectivamente 25, 50 y 100 mcg/h durante 72 h.
91
Morfina
ADMINISTRACION:
INYECCION IV DIRECTA : SI
– Administrar la dosis precrita muy lentamente . Diluir la dosis en 4-5 ml de agua p.i. antes de administrar. La administración rápida aumenta el riesgo de aparición de efectos secundarios (depresión respiratoria, apnea, hipotensión).
INFUSION INTERMITENTE : SI
– Diluir la dosis prescrita en 50-100 ml de SF ó SG5%.
INFUSION CONTINUA : SI
– Diluir la dosis prescrita en 500-1000 ml de SF ó SG5%.
INYECCION IM : SI
– Esta vía es preferible sobre la vía subcutánea cuando deben administrarse dosis repetidas. Aunque la absorción es más irregular y la duración de acción menor que si se usa la vía sc.
INYECCION SUBCUTANEA : SI
– La absorción es más lenta que por vía IM, pero la analgesia suele ser más constante y duradera .
SUEROS COMPATIBLES : SF, SG5%
OBSERVACIONES :
– El preparado sin conservante también se puede administrar via epidural e intratecal.
92
Morfina
DOSING: ADULTS —
Acute pain (moderate-to-severe):
Oral: Prompt release formulations: Opiate-naive: Initial: 10 mg every 3 to
4 hours as needed; patients with prior opiate exposure may require higher initial doses: usual dosage range: 10-30 mg every 3-4 hours as needed
I.M., SubQ:.
Initial: Opiate-naive: 5-10 mg every 3-4 hours as needed ; patients with prior opiate exposure may require higher initial doses; usual dosage range:
5-20 mg every 3-4 hours as needed
Rectal: 10-20 mg every 3-4 hours
I.V.: Initial: Opiate-naive: 2.5-5 mg every 3 to 4 hours ; patients with prior opiate exposure may require higher initial doses. Note: Repeated doses
(up to every 5 minutes if needed) in small increments (eg, 1-4 mg) may be preferred to larger and less frequent doses.
93
94
Morfina
DOSING: PEDIATRIC —
– Acute pain (moderate-to-severe): Children >6 months and <50 kg:
Oral (prompt release): 0.15-0.3 mg/kg every 3-4 hours as needed
I.M.: 0.1 mg/kg every 3-4 hours as needed
I.V.: 0.05-0.1 mg/kg every 3-4 hours as needed
I.V. infusion: Range: 10-30 mcg/kg/hour
– Sedation/analgesia for procedures: Adolescents >12 years: I.V.: 3-4 mg and repeat in 5 minutes if necessary
95
Morfina
DOSING: ELDERLY — Refer to adult dosing. Use with caution; may require reduced dosage in the elderly and debilitated patients .
DOSING: RENAL IMPAIRMENT
– Clcr 10-50 mL/minute: Administer 75% of normal dose.
– Clcr <10 mL/minute: Administer 50% of normal dose.
DOSING: HEPATIC IMPAIRMENT — Unchanged in mild liver disease; substantial extrahepatic metabolism may occur. Excessive sedation may occur in cirrhosis.
96
Morfina
ADVERSE REACTIONS SIGNIFICANT —
>10%:
Cardiovascular: Palpitations, hypotension, bradycardia
Central nervous system: Somnolencia (48%, tolerance usually develops to drowsiness with regular dosing for 1-2 weeks); mareos (20%), confusion , headache (following epidural or intrathecal use)
Dermatologic: Pruritus (may be secondary to histamine release)
Note: Pruritus may be dose-related, but not confined to the site of administration.
Gastrointestinal: Nausea (28%, tolerance usually develops to nausea and vomiting with chronic use); constipation (40%, tolerance develops very slowly if at all); xerostomia (78%)
Genitourinary: Urinary retention (16%; may be prolonged, up to 20 hours, following epidural or intrathecal use)
Local: Pain at injection site
Neuromuscular & skeletal: Weakness
Miscellaneous: Histamine release
97
Morfina
DRUG INTERACTIONS — Substrate of CYP2D6 (minor)
Antipsychotic agents: May increase hypotensive effects of morphine; monitor.
CNS depressants : May increase the effects/toxicity of morphine; monitor.
MAO inhibitors : May increase the effects/toxicity of morphine; some manufacturers recommend avoiding use within 14 days of MAO inhibitors
Pegvisomant: Therapeutic efficacy may be decreased by concomitant opiates, possibly requiring dosage adjustment of pegvisomant.
Rifamycin derivatives: May decrease levels/effects of morphine; monitor.
Selective serotonin reuptake inhibitors (SSRIs) and meperidine:
Serotonergic effects may be additive, leading to serotonin syndrome.
98
Morfina
PREGNANCY IMPLICATIONS — Morphine crosses the placenta.
The frequency of congenital malformations has not been reported to be greater than expected in children from mothers treated with morphine during pregnancy. Reduced growth and behavioral abnormalities in offspring have been observed in animal studies. Neonates born to mothers receiving chronic opioids during pregnancy should be monitored for neonatal withdrawal syndrome.
LACTATION — Enters breast milk
99
Morfina
REFERENCE RANGE —
– Therapeutic: Surgical anesthesia: 65-80 ng/mL (SI: 227-280 nmol/L);
– Toxic: 200-5000 ng/mL (SI: 700-17,500 nmol/L)
TOXICOLOGY / OVERDOSE COMPREHENSIVE —
Symptoms include respiratory depression, miosis, hypotension, bradycardia, apnea, and pulmonary edema.
Treatment includes
– airway support,
– establishment of an I.V. line, and
– administration of naloxone 2 mg I.V
. (0.01 mg/kg for children), with repeat administration as necessary, up to a total of 10 mg.
– Primary attention should be directed to ensuring adequate respiratory exchange.
100
Morfina
PHARMACODYNAMICS / KINETICS
Onset of action:
– Oral (immediate release): ~30 minutes;
– I.V.: 5-10 minutes
Duration: Pain relief:
Immediate release formulations: 4 hours
Extended release epidural injection (DepoDur™): >48 hours
Absorption: Variable
Distribution: Vd: 3-4 L/kg; binds to opioid receptors in the CNS and periphery (eg, GI tract)
Protein binding: 30% to 35%
101
Morfina
PHARMACODYNAMICS / KINETICS
Metabolism: Hepatic via conjugation with glucuronic acid to morphine-3-glucuronide (inactive), morphine-6-glucuronide
(active), and in lesser amounts, morphine-3-6-diglucuronide; other minor metabolites include normorphine (active) and the 3-ethereal sulfate
Bioavailability: Oral: 17% to 33% (first-pass effect limits oral bioavailability oral; parenteral effectiveness reportedly varies from
1:6 in opioid naive patients to 1:3 with chronic use)
Half-life elimination: Adults: 2-4 hours (immediate release forms)
Time to peak, plasma: Kadian®: ~10 hours
102
Morfina
PHARMACODYNAMICS / KINETICS
Excretion: Urine (primarily as morphine-3-glucuronide, ~2% to 12% excreted unchanged); feces (~7% to 10%).
It has been suggested that accumulation of morphine-6glucuronide might cause toxicity with renal insufficiency.
All of the metabolites (ie, morphine-3-glucuronide, morphine-6glucuronide, and normorphine) have been suggested as possible causes of neurotoxicity (eg, myoclonus).
103
Morfina
Dosis de carga
Dosis de manteni miento
FG > 50 ml/min
FG 10-50 ml/min
FG < 10 ml/min
Dosis suplemta ria tras
HD
DPCA
100% 75% 50%
TSCR
Ninguna Desconocida
Dosis FG
10-50%
104
Buprenorfina
Agonista parcial . Ello significa que la activación del receptor opioide mu por la buprenorfina a dosis máximas no consigue alcanzar los efectos máximos de la morfina.
Presenta una intensa unión al receptor opioide , lo que tiene repercusiones en el tratamiento de la intoxicación aguda
Efecto máximo inferior al de morfina o fentanilo, pero difícil de revertir con antagonistas puros.
105
Buprenorfina
Cuando se administra buprenorfina a pacientes que están recibiendo agonistas puros, puede producirse un cierto grado de antagonismo funcional que, incluso, puede producir un cierto síndrome de abstinencia.
106
N02AAnalgésicos narcóticos (Opioides)
NOMBRE GENÉRICO PRESENTACIÓN
Buprenorfina
Metadona
Petidina (Meperidina)
Comp 0,2 mg
Amp 0,3 mg/1 ml
Amp 10 mg/1 ml
Comp 5 mg
Comp 40 mg
Amp 100 mg/2 ml
VIA NOMBRE
COMERCIAL
Buprex CE SL
IM, IV
SC, IM
OR
OR
Metasedin CE
SC, IM, IV Dolantina CE
CE: Control de estupefacientes.
Nota 1: Comprimidos ranurados.
Nota 2: Uso restringido para tratamiento del dolor crónico.
Nota 3: Los parches de 2,5, 5 y 10 mg liberan respectivamente 25, 50 y 100 mcg/h durante 72 h.
107
Buprenorfina
DOSING: ADULTS —
Long-term use is not recommended
Acute pain (moderate to severe):
I.M.: Initial: Opiate-naive: 0.3 mg every 6-8 hours as needed; initial dose (up to 0.3 mg) may be repeated once in 30-60 minutes after the initial dose if needed; usual dosage range: 0.15-
0.6 mg every 4-8 hours as needed
Slow I.V.: Initial: Opiate-naive: 0.3 mg every 6-8 hours as needed; initial dose (up to 0.3 mg) may be repeated once in 30-60 minutes after the initial dose if needed
108
Buprenorfina
Heroin or opiate withdrawal (unlabeled use): I.M., slow I.V.: Variable;
0.1-0.4 mg every 6 hours
Opioid dependence : Sublingual:
Induction: Range: 12-16 mg/day (doses during an induction study used 8 mg on day 1, followed by 16 mg on day 2; induction continued over 3-4 days). Treatment should begin at least 4 hours after last use of heroin or short-acting opioid, preferably when first signs of withdrawal appear. Titrating dose to clinical effectiveness should be done as rapidly as possible to prevent undue withdrawal symptoms and patient drop-out during the induction period.
Maintenance: Target dose: 16 mg/day; range: 4-24 mg/day; patients should be switched to the buprenorphine/naloxone combination product for maintenance and unsupervised therapy
109
Buprenorfina
DOSING: PEDIATRIC
Acute pain (moderate to severe):
Children 2-12 years: I.M., slow I.V.: 2-6 mcg/kg every 4-
6 hours
Children 13 years: Refer to adult dosing.
DOSING: ELDERLY — Moderate to severe pain: I.M., slow I.V.: 0.15 mg every 6 hours; elderly patients are more likely to suffer from confusion and drowsiness compared to younger patients. Long-term use is not recommended.
110
Buprenorfina
DRUG INTERACTIONS
— Substrate of CYP3A4 (major); Inhibits CYP1A2 (weak),
2A6 (weak), 2C19 (weak), 2D6 (weak)
Cimetidine : May increase sedation from narcotic analgesics; however, histamine blockers may attenuate the cardiovascular response from histamine release associated with narcotic analgesics.
CNS depressants : May produce additive respiratory and CNS depression; includes benzodiazepines, barbiturates, ethanol, and other sedatives. Respiratory and CV collapse was reported in a patient who received diazepam and buprenorphine.
CYP3A4 inducers: CYP3A4 inducers may decrease the levels/effects of buprenorphine. Example inducers include aminoglutethimide, carbamazepine, nafcillin, nevirapine, phenobarbital, phenytoin, and rifamycins.
CYP3A4 inhibitors: May increase the levels/effects of buprenorphine. Example inhibitors include azole antifungals, clarithromycin, diclofenac, doxycycline, erythromycin, imatinib, isoniazid, nefazodone, nicardipine, propofol, protease inhibitors, quinidine, and verapamil.
Naltrexone: May antagonize the effect of narcotic analgesics; concurrent use or use within 7-10 days of injection for pain relief is contraindicated.
111
Buprenorfina
PREGNANCY IMPLICATIONS —
Withdrawal has been reported in infants of women receiving buprenorphine during pregnancy. Onset of symptoms ranged from day 1 to day 8 of life, most occurring on day 1.
LACTATION — Enters breast milk. Not recommended
112
Buprenorfina
TOXICOLOGY / OVERDOSE
COMPREHENSIVE —
Symptoms include CNS depression, pinpoint pupils, hypotension, and bradycardia.
Treatment is supportive.
– Naloxone may have limited effects in reversing respiratory depression ;
– Doxapram has also been used to stimulate respirations
113
Buprenorfina
PHARMACODYNAMICS / KINETICS
Onset of action: Analgesic: 10-30 minutes
Duration: 6-8 hours
Absorption: I.M., SubQ: 30% to 40%
Distribution: Vd: 97-187 L/kg
Protein binding: High
Metabolism: Primarily hepatic ; extensive first-pass effect
Half-life elimination: 2.2-3 hours
Excretion: Feces (70%); urine (20% as unchanged drug)
114
Meperidina
Existe otro tipo de opioides denominados agonistasantagonistas , que son capaces de actuar como agonistas sobre un tipo de receptores y como antagonistas sobre otro tipo, por lo que producen respuestas imprevisibles.
En pacientes que reciben agonistas puros, los agonistas-antagonistas pueden precipitar reacciones de abstinencia.
115
Meperidina
Agonistas-antagonista.
Estos fármacos tienen afinidad, variable de unos a otros, por los diferentes subtipos de receptores. En general se comportan como agonistas totales de kappa, pero como agonistas parciales, e incluso antagonistas, de receptores mu.
Las consecuencias, dependen de si se ha administrado previamente un agonista total o no. En ausencia de éstos, el resultado es un efecto analgésico, resultado de la activación de receptores mu (parcial) y kappa (total). Ahora bien, si los pacientes están recibiendo un agonista total (morfina, fentanilo), el resultado será un desplazamiento del receptor y una activación parcial de éste por los agonistas-antagonistas .
En consecuencia, los pacientes sentirán un grado menor de analgesia , lo que se interpreta como un antagonismo, cuando con frecuencia realmente no lo es desde un punto farmacológico estricto.
116
N02AAnalgésicos narcóticos (Opioides)
NOMBRE GENÉRICO PRESENTACIÓN
Buprenorfina
Metadona
Comp 0,2 mg
Amp 0,3 mg/1 ml
Amp 10 mg/1 ml
Comp 5 mg
Comp 40 mg
Petidina (Meperidina) Amp 100 mg/2 ml
VIA NOMBRE
COMERCIAL
Buprex CE SL
IM, IV
SC, IM
OR
OR
Metasedin CE
SC, IM, IV Dolantina CE
CE: Control de estupefacientes.
Nota 1: Comprimidos ranurados.
Nota 2: Uso restringido para tratamiento del dolor crónico.
Nota 3: Los parches de 2,5, 5 y 10 mg liberan respectivamente 25, 50 y 100 mcg/h durante 72 h.
117
Meperidina
INYECCION IV DIRECTA : SI
Administrar la dosis prescrita en forma de inyección IV lenta, para ello disolver con
SF de forma que la concentración final sea 5 o 10 mg/ml. Ejemplo tomar 1 o 2 ml de la ampolla con una jeringa y completar el volumen hasta 10 ml. Administrar en 1 a 2 minutos.
INFUSION INTERMITENTE : SI
Diluir la dosis prescrita en 50100 ml de SF ó SG5%. Administrar según pauta médica.( Ejemplo 0,3 mg/Kg/hora).
INFUSION CONTINUA : SI
En ocasiones, para mantener a un paciente sedado se utiliza el llamado "coctel lítico", éste está compuesto por: Meperidina (Dolantina), Clorpromazina (Largactil) y
Prometacina (Frinova). se administra en forma de infusión continua, en SF ó SG5%.
INYECCION IM : SI
Administrar la dosis prescrita en forma de inyección IM profunda. Es de elección especialmente en dosis múltiples se prefiere a la vía SC
INYECCION SUBCUTANEA : SI
Cuando deban administrarse dosis repetidas, es preferible la vía IM, ya que la vía SC es irritante de los tejidos.
SUEROS COMPATIBLES : SF, SG5% 118
Meperidina
DOSING: ADULTS —
– Not recommended for chronic pain.
– In patients with normal renal function, doses of 600 mg/24 hours and use for 48 hours are recommended
(American Pain Society, 1999).
Pain (analgesic):
I.M., SubQ: Initial: Opiate-naive: 50-75 mg every 3-4 hours as needed ; patients with prior opiate exposure may require higher initial doses.
119
Meperidina
DOSING: PEDIATRIC —
– Oral, I.M., I.V., SubQ: Children: 1-1.5 mg/kg/dose every 3-4 hours as needed; 1-2 mg/kg as a single dose preoperative medication may be used; maximum 100 mg/dose. (Oral route is not recommended for acute pain.)
DOSING: ELDERLY —
– Oral: 50 mg every 4 hours
– I.M.: 25 mg every 4 hours
120
Meperidina
DOSING: RENAL IMPAIRMENT
– Clcr 10-50 mL/minute: Administer 75% of normal dose.
– Clcr <10 mL/minute: Administer 50% of normal dose.
– Repeated use in renal impairment should be avoided due to potential accumulation of neuroexcitatory metabolite .
DOSING: HEPATIC IMPAIRMENT — Increased narcotic effect in cirrhosis; reduction in dose is more important for oral than I.V. route.
121
Meperidina
ADVERSE REACTIONS SIGNIFICANT —
Cardiovascular: Hypotension
Central nervous system: Fatigue, drowsiness, dizziness, nervousness, headache, restlessness, malaise, confusion, mental depression, hallucinations, paradoxical CNS stimulation, increased intracranial pressure, seizure (associated with metabolite accumulation), serotonin syndrome
Dermatologic: Rash, urticaria
Gastrointestinal: Nausea, vomiting, constipation, anorexia, stomach cramps, xerostomia, biliary spasm, paralytic ileus, sphincter of Oddi spasm
Genitourinary: Ureteral spasms, decreased urination
Local: Pain at injection site
Neuromuscular & skeletal: Weakness
Respiratory: Dyspnea
Miscellaneous: Histamine release, physical and psychological dependence
122
Meperidina
PRECAUTIONS —
Meperidine is not recommended for the management of chronic pain.
When used for acute pain (in patients without renal or CNS disease), treatment should be limited to 48 hours and doses should not exceed 600 mg/24 hours.
Normeperidine (an active metabolite and CNS stimulant) may accumulate and precipitate anxiety, tremors, or seizures; risk increases with renal dysfunction and cumulative dose.
123
Meperidina
DRUG INTERACTIONS
Substrate (minor) of CYP2B6, 2C19, 3A4
Acyclovir: May increase meperidine metabolite concentrations. Use caution.
Barbiturates: May decrease analgesic efficacy and increase sedative and/or respiratory depressive effects of meperidine.
Cimetidine: May increase meperidine metabolite concentrations; use caution.
CNS depressants (including benzodiazepines): May potentiate the sedative and/or respiratory depressive effects of meperidine.
MAO inhibitors: May enhance the serotonergic effect of meperidine, which may cause serotonin syndrome. Concurrent use with or within 14 days of an MAO inhibitor is contraindicated.
Phenothiazines: May potentiate the sedative and/or respiratory depressive effects of meperidine; may increase the incidence of hypotension.
Phenytoin: May decrease the analgesic effects of meperidine
Ritonavir: May increase meperidine metabolite concentrations; use caution.
Serotonin agonists: Serotonin agonists and meperidine may enhance serotonin levels in the brain.
Serotonin syndrome may occur.
Serotonin reuptake inhibitors: May potentiate the effects of meperidine, increasing serotonin levels in the brain. Serotonin syndrome may occur.
Sibutramine: May enhance the serotonergic effect of meperidine. Serotonin syndrome may occur.
Tricyclic antidepressants: May potentiate the sedative and/or respiratory depressive effects of meperidine. In addition, potentially may increase the risk of serotonin syndrome.
124
Meperidina
PREGNANCY IMPLICATIONS —
– Meperidine is known to cross the placenta , which may result in respiratory or CNS depression in the newborn.
LACTATION —
– Enters breast milk. contraindicated
125
Meperidina
REFERENCE RANGE — Therapeutic: 70-500 ng/mL
(SI: 283-2020 nmol/L); Toxic: >1000 ng/mL (SI: >4043 nmol/L)
TOXICOLOGY / OVERDOSE COMPREHENSIVE —
Symptoms include CNS depression, respiratory depression, mydriasis, bradycardia, pulmonary edema, chronic tremors, CNS excitability, and seizures.
Treatment of overdose includes airway support, establishment of an I.V. line, and administration of naloxone 2 mg I.V. (0.01 mg/kg for children), with repeat administration as necessary, up to a total of 10 mg.
Naloxone should not be used to treat meperidineinduced seizures. Naloxone does not reverse the adverse effects of normeperidine.
126
Meperidina
PHARMACODYNAMICS / KINETICS
Onset of action: Analgesic: Oral, SubQ: 10-15 minutes; I.V.: ~5 minutes
Peak effect: SubQ.: ~1 hour; Oral: 2 hours
Duration: Oral, SubQ.: 2-4 hours
Absorption: I.M.: Erratic and highly variable
Distribution: Crosses placenta; enters breast milk
Protein binding: 65% to 75%
Metabolism: Hepatic; hydrolyzed to meperidinic acid (inactive) or undergoes
N-demethylation to normeperidine (active; has 1/2 the analgesic effect and
2-3 times the CNS effects of meperidine)
Bioavailability: ~50% to 60%; increased with liver disease
Half-life elimination:
Parent drug: Terminal phase: Adults: 2.5-4 hours, Liver disease: 7-11 hours
Normeperidine (active metabolite): 15-30 hours; can accumulate with high doses or with decreased renal function
Excretion: Urine (as metabolites)
127
Meperidina
Dosis de carga
Dosis de manteni miento
FG > 50 ml/min
FG 10-50 ml/min
FG < 10 ml/min
Dosis suplemta ria tras
HD
DPCA
75% 50%
TSCR
Clcr 10-50 mL/minute: Administer 75% of normal dose.
Clcr <10 mL/minute: Administer 50% of normal dose.
Repeated use in renal impairment should be avoided due to potential accumulation of neuroexcitatory metabolite .
128