CHP Direct Claims Submission Training
advertisement

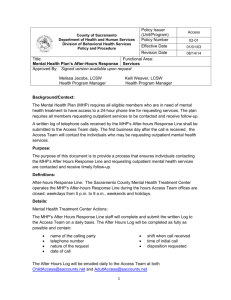
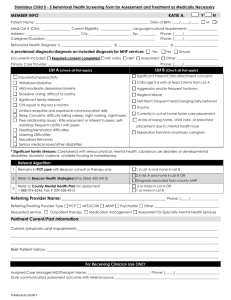
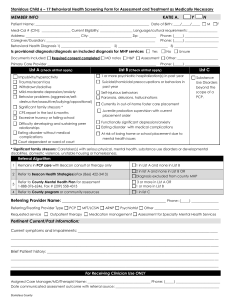
Illinois Department of Human Services / Division of Mental Health and Illinois Mental Health Collaborative Present CHP Direct Claims Submission Training January 2010 Claims Training Agenda 2 Overview of CHP Services Billing Guidelines Direct Claim Submission on ProviderConnect Claim Helpful Hints CHP Claims 3 Under the Collaborative IT system, all services are submitted as claims and all claims must be submitted electronically Community Health and Prevention Service claims may be submitted to the Collaborative for dates of service 8/1/2009 and after. Program Code: CHP CHP Service Codes New Modifier Order Service Name CPT HCPCS 1 4 2 Bill Unit (hrs) 3 H0031 AH Mental health assessment (LCP) 0.25 H0031 HN Mental health assessment (MHP) 0.25 H0031 HO Mental health assessment (QMHP, AM/MA) 0.25 H0032 HN Treatment plan development, review, modification (MHP) 0.25 H0032 HO Treatment plan development, review, modification (QMHP) 0.25 90862 52 Psychotropic medication monitoring 0.25 90862 SA Psychotropic medication monitoring (APN) 0.25 90862 UA Psychotropic medication monitoring (MD/DO/DC) 0.25 H0002 HE Case management - LOCUS H0004 HN Therapy/counseling--individual (MHP) 0.25 H0004 HO Therapy/counseling--individual (QMHP) 0.25 H0004 HQ HN Therapy/counseling--group (MHP) 0.25 H0004 HQ HO Therapy/counseling--group (QMHP) 0.25 H0004 HR HN Therapy/counseling--family (MHP) 0.25 H0004 HR HO Therapy/counseling--family (QMHP) 0.25 Event CHP Service Codes New Modifier Order Service Name CPT HCPCS 1 H0034 HN H0034 HQ H0034 2 Psychotropic medication training--Individual 0.25 Psychotropic medication training--group (APN) 0.25 HQ Psychotropic medication training--group 0.25 H0034 SA Psychotropic medication training--Individual (APN) 0.25 H0039 HQ Assertive community treatment, group 0.25 H0039 HT Assertive community treatment 0.25 Crisis intervention 0.25 SA H2011 5 Bill Unit (hrs) 3 H2011 HK Crisis intervention, state operated facility screening 0.25 H2011 HT Crisis intervention--multiple staff 0.25 H2015 HE HM Community support, residential, individual (RSA) 0.25 H2015 HE HN Community support, residential, individual (MHP) 0.25 H2015 HE HO Community support, residential, individual (QMHP) 0.25 H2015 HM Community support, individual (RSA) 0.25 H2015 HN Community support, individual (MHP) 0.25 H2015 HO Community support, individual (QMHP) 0.25 H2015 HQ HE HM Community support, residential, group (RSA) 0.25 H2015 HQ HE HN Community support, residential, group (MHP) 0.25 H2015 HQ HE HO Community support, residential, group (QMHP) 0.25 H2015 HQ HM Community support, group (RSA) 0.25 H2015 HQ HN Community support, group (MHP) 0.25 H2015 HQ HO Community support, group (QMHP) 0.25 CHP Service Codes New Modifier Order Service Name CPT HCPCS 1 3 Bill Unit (hrs) H2015 HT Community support, team 0.25 H2017 HM Psychosocial rehabilitation, individual (RSA) 0.25 H2017 HN Psychosocial rehabilitation, individual (MHP) 0.25 H2017 HO Psychosocial rehabilitation, individual (QMHP) 0.25 H2017 HQ HM Psychosocial rehabilitation, group (RSA) 0.25 H2017 HQ HN Psychosocial rehabilitation, group (MHP) 0.25 H2017 HQ HO Psychosocial rehabilitation, group (QMHP) 0.25 S9480 HA HO Mental health intensive outpatient--child 1.00 S9480 HO Mental health intensive outpatient--adult 1.00 T1016 HK HN Case management--mandated follow-up (MHP) 0.25 T1016 HK HO Case management- mandated follow-up (QMHP) 0.25 T1016 HM Case management--mental health (RSA) 0.25 T1016 HN Case management--transition linkage and aftercare (MHP) 0.25 T1016 HO Case management--transition linkage and aftercare (QMHP) 0.25 T1016 TF Case management--mental health (MHP) 0.25 T1016 TG Case management--client-centered consultation (MHP) 0.25 T1016 TG Case management--client-centered consultation (RSA) 0.25 T1502 6 2 T1502 SA HN Psychotropic medication administration (LPN/RN) Event Psychotropic medication administration (APN) Event Claims Submission and Billing Guidelines Registration Requirement Before claim is submitted, consumer must be registered by the agency performing the service 8 Consumer Information 9 Standardized claims transactions require certain consumer information to verify the individual’s identity The Collaborative has minimized the consumer information necessary for a claim to be submitted, while assuring that each service claim is correctly associated to the appropriate consumer Claim Level Information Consumer Information Required • RIN Consumer Name Date of Birth • Gender • All must match exactly to the registration information on file Consumer address is optional • • • 10 Claim Level Information (cont.) Provider Information required on each claim 11 10 digit NPI number that matches the NPI on file with the Collaborative Tax ID Number (FEIN) Service Location Taxonomy Codes are optional Service code and modifier combinations will identify staff level Claim Level Information (cont.) Program Codes Submit the Program Code for the service provided: Program Code: CHP 12 Claim Line Level Information Service Codes Service codes must be valid HCPCS or CPT codes as shown on Service Matrix found at http://www.illinoismentalhealthcollaborative.com/ 13 Claim Line Level Information (cont.) Modifiers 14 Staff Level Modifiers drive the allowable amount applied to a service – If no staff level modifier is submitted, the claim will be denied unless the service does not require a Staff Level Modifier Modifier Position is very important – Staff Level Modifier should always be in the last modifier position when multiple modifiers are submitted Claim Line Level Information (cont.) Staff Level Modifiers 15 AH – LCP - Licensed Clinical Psychologist HN – MHP - Mental Health Professional HO – QMHP - Qualified Mental Health Professional SA – APN -Advanced Practice Nurse HM – RSA - Rehabilitative Services Associate UA – MD, DO, DC Claim Line Level Information (cont.) Diagnosis Codes 16 Must be ICD-9 and include 4th and 5th digit according to ICD-9 guidelines Only Mental Health diagnoses that are DMH/DHS defined will be accepted. Claim Line Level Information (cont.) Line Notes For all services, the following are required: Delivery method Service start time Service duration Staff ID Situational Requirements: For group based services show the group id, # clients in group, and # of staff in the group 17 DMH considers these data elements to be important and necessary components of billing and service reporting Review Services Matrix The Service Matrix is posted on the Collaborative Website in an Excel Spreadsheet that you may download. http://www.illinoismentalhealthcollaborative.com/ 18 Direct Claim Submission 20 21 ProviderConnect 22 23 24 25 26 27 28 29 30 31 32 Submitting Corrected/Replacement Claims When an original claim was incorrectly billed, send a corrected or replacement claim by indicating the Claim Frequency Type Code – 6=Corrected – 7=Replacement 33 Enter the Collaborative’s original Claim Number Questions? 34 Claims Helpful Hints Helpful Hints to Faster Claim Processing Submit the correct Consumer RIN in the Consumer ID field – 36 if the RIN doesn’t match the DHS assigned number, the claim will be uploaded to our claims processing system identifying the Consumer as “UNKNOWN” Helpful Hints to Faster Claim Processing (cont.) Multiple units of service rendered by the same practitioner staff level, on the same day, for the same client, must be submitted on one claim. – – 37 All units for one service code must be submitted on one line. If claims are submitted separately, claims will be denied as a duplicate service. Helpful Hints to Faster Claim Processing (cont.) 38 Example: H2015 HN Community support, individual (MHP) For Consumer RIN 123456789 – 10 AM 4 units, noon 2 units, 6PM 3 units – Submit H2015 HN on one line, with 9 units. Start time is 9999, duration: 135 minutes Helpful Hints to Faster Claim Processing (cont.) A separate claim must be submitted for every different staff level rendering services (except for multiple disciplinary groups) 39 Most Common Reasons for Claim Denial Consumer Information: – – – – 40 RIN doesn’t match the RIN assigned by DHS or registration Service code on the claim is not on the list of covered services Service code billed is not one the provider is contracted to render (the service is not on the provider’s fee schedule). Consumer is not eligible/registered on the date of service. Most Common Reasons for Claim Denial (cont.) Codes/Modifiers – – – – – 41 Place of service code on the claim is not a valid place of service code for the service rendered Modifier code billed on the claim is not valid with the CPT or HCPCS code Staff level modifier is not billed on the claim Diagnosis code is not an ICD-9 code Diagnosis code does not contain a required 4th or 5th digit Most Common Reasons for Claim Denial (cont.) Billing - Duplicate/Non-Rolled Services - Third Party Liability - TPL not billed with claim - TPL information on claim incomplete 42 Timely Filing of Claims 43 Claims for all services must be received by the Collaborative within 365 days of the date of service Claims Involving Third Party Liability (TPL) must be received by the Collaborative within 365 days of the date of the other carrier’s Explanation of Benefits (EOB), or notification of payment / denial. Timely filing limit applies to replacement claims as well as original claims; claims must be received by the Collaborative within 365 days from date of service. Questions and Answers 44 Thank you! Illinois Mental Health Collaborative for Access and Choice