Pneumonia - cnhsa.com
advertisement

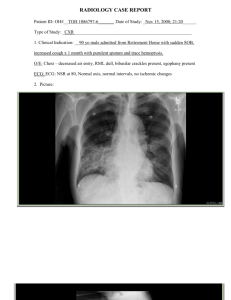
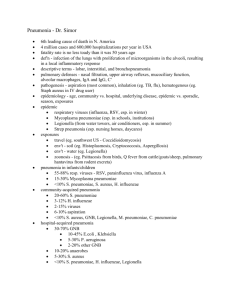
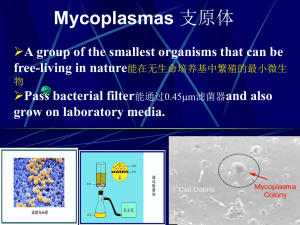
Pneumonia Community acquired Pneumonia ( CAP ) Hospital acquired Pneumonia ( HAP) ( Ventilator associated Pneumonia (VAP) ) is the most serious form of HAP… Health care Associated Pneumonia (HCAP) 2005 • Community acquired Pneumonia( CAP) • Pneumonia in a Community Resident outside the hospital setting • Hospital acquired (Nosocomial) Pneumonia( HAP ) • Pneumonia that occurs 48 hours or more after admission • Ventilator associated Pneumonia (VAP) • HAP that develops more than 48 hours after intubation. • Health care Associated Pneumonia (HCAP) • • • • • • In 2005 ATA /IDSA Introduced HCAP ( previously CAP ) (Multidrug Resistance Pathogens ) Residence in a Nursing Home or other long-term care facility Attend at a Hospital or Hemodialysis clinic within prior 30 days IV therapy, wound care, or IV chemotherapy within the prior 30 days Pneumonia that occurs in a non-hospitalized patient with extensive healthcare contact… Hospitalization in an acute care hospital for two or more days within the prior 90 days Community Acquired Pneumonia • Pneumonia is a lower respiratory infection involving the lungs especially affecting the Alveoli characterized by filling of the alveolar space with inflammatory cells and fluids …. • Clinically characterized by respiratory symptoms , cough, sputum , dyspnea , pleuritic chest pain with fever, chills , tachypnea , tachycardia and the appearance of a new infiltrate / opacity on CXR • In the elderly symptoms differ ( with fewer respiratory symptoms ) confusion, failure to thrive, fall, and worsening of chronic underlying illness e.g. CHF • Severity ranges from mild to life threatening Etiology : Pathogens differ in different continents or geographic areas. Outpatients are different from Inpatients , ICU and from Nursing Home Microbiology Pathogens : • Bacteria : Strept Pneumoniae , H. Influenzae , Chlamydia , Mycoplasma and Legionella • Viruses : Adenovirus, Influenza and Para influenza, …RSV • Fungal : Histoplasmosis , Coccidomycosis, Blastomycosis, Pneumocystis Jiroveci in HIV , or other immune suppressed patients • Rare causes are Fungi and Parasite . • • • • • • • Majority are caused by Bacteria S. Pneumoniae ( GPC) H. Influenzae (GNR ) Chlamydia Mycoplasma Other : Staph, Legionella, Moraxella, Gram negative bacilli 1/3 of CAP are caused by viruses Streptococcus pneumoniae is the most common cause worldwide. Epidemiology • • • • • • • • • In the US more than 5 million / year 20 % ~ more than a Million Hospitalized In 2005 > 60 000 died Cost ~ 10 billon /year Age : Highest at extreme of ages , Elderly More in Males More in African and Native Americans More in Winter Mortality highest in hospitalized patients and those with risk factors Pathogenesis • Bacteria enter the lung through several routes: • 1. Micro Aspiration the most common way. (From previously colonized oropharynx) • 2. Macro ( Aspiration ) (stroke, seizure, CVA) Loss of neurologic protection of the upper airway • 3. Inhalation of Legionella or TB ( airborne) • 4. Hematogenous: from extra pulmonary sites of infection • 5. Direct extension / spread from nearby (e.g., liver abscess). • 6. Critically ill / ICU / Ventilator: Retrograde spread from a colonized stomach to the oropharynx • The lungs are exposed to invading pathogens and colonized oropharyngeal bacteria yet it remains sterile and pneumonia is infrequent because of the antibacterial respiratory defenses • Pulmonary defenses : • Muco-Ciliary, Phagocytes, Antibody Response… • Pneumonia develops if Host defenses are overwhelmed by infectious pathogen Pathogenesis… • • • • • • Poor Immune system >> Poor immune response >> Pneumonia Immune dysfunction ( Severe illness, Sepsis or Steroid / Chemo ) Chronic Illness ( CHF, DM, CRF, COPD, Chronic Liver Disease) Anatomic abnormalities (endobronchial obstruction, bronchiectasis) Or Adequate Immune System : overwhelmed by virulent microorganism. • Virulence factors: some microorganisms develop ways to overcome host defenses • Chlamydia produces cilio-static factor. • Mycoplasma shears off cilia. • Influenza virus reduces tracheal muco-ciliary clearance. • S. pneumoniae produces factors that inhibits phagocytosis • Mycobacterium &Legionella are resistant to the anti microbicidal activity of phagocytes Risk factors Impairs pulmonary defenses >> increased • • • • • • • • • • • • • risk of CAP Chronic lung diseases , Smokers, Asthma ,COPD, Bronchiectasis ,Fibrosis Alcoholics (x9) Homeless , Prisoners Immunosuppressed, Spleenectomy, Cancer , HIV (x 40 ) Chronic liver or chronic kidney diseases , CHF ,CVA Seizures, Dementia Recent Abx Elderly Malnutrition Military recruits Steroids Inhaled steroids, ipratropium and bronchodilators PPI , H2 blockers Antipsychotics Specific risk factors PNEUMONIA Exposure to birds Psittacosis Exposure to bat or bird droppings Histoplasma Exposure to Rabbits Tularemia Cruise ship or hotel previous 2 weeks Legionella Exposure to farm animals Q fever , Coxiella Burnetti IVDU Staph Aureus, Anaerobes , TB MRSA focus, Live in crowded conditions CA-MRSA Bronchiectasis Staph and Pseudomonas Neutropenia Recent Abx Gram Negative Microbiology … OUTPATIENT INPATIENT ICU / SEVERE CASES S. Pneumoniae S. Pneumoniae S. Pneumoniae Mycoplasma Pneumoniae Mycoplasma Pneumoniae Staph Aureus H Influenzae Chlamydia Pneumoniae Legionella Chlamydia Pneumoniae H Influenzae Gram Negative Bacilli Pseudomonas & E. Coli Respiratory Viruses Influenza A & B RSV , Adenoviruses Para Influenza Legionella H Influenzae Aspiration / Anaerobes Microbiology Is Changing Respiratory Viruses Multidrug Resistance • Symptoms: • • • • • • • • • • • Fever, cough, sputum, pleuritic chest pain, shortness of breath chills & shakes Headache, Nausea, Vomiting, Diarrhea, Fatigue, Myalgia, Joint pain Non respiratory symptoms : Confusion & falls ( in the elderly ) … Pleuritic pain more with bacterial pneumonia Rusty sputum to pneumococcal pneumonia Hemoptysis “ more with Klebsiella & TB Constant repetitive harsh dry cough with fever 3days + more with Mycoplasma Pneumonia plus GI symptoms (diarrhea, abdominal pain ) myalgia's, headache confusion and high fever ~ 104 think Legionella Viral pneumonia usually with dry non productive cough , ha, malaise Signs: Chest signs : ( Bronchial breath sounds, dullness , crackles, pleural rub, rhonchi ) Fever , Tachypnea , Tachycardia Elderly ( Hypothermia , confusion, hypotension , falls …. ) Diagnosis • • • • • • – Diagnosis is suggested by symptoms and signs . – Should be confirmed by CXR which almost always show some infiltrate … – CXR is Indicated in All cases of suspected CAP ( T 100+, P 100, RR > 20 ) Rarely false negative CXR …attributed to an infection very early in the course , Neutropenia, Dehydration, and Pneumocystis Pneumonia Pneumocystis Pneumonia : 1/3 of patients have normal CXR early in the disease CXR is essential in an elderly or chronically ill patient who can have pneumonia with only non respiratory findings “ confusion, hypotension , loss of appetite, fall, failure to thrive “ CXR to confirm Dx , can help identify severe , complicated cases (Multi- Lobar Pneumonia , Pleural Effusion, Cavitation ) If S&S of pneumonia with Negative CXR : Diagnosis is “ Bronchitis “ therefore NO Abx is needed if no underlying lung disease… Investigations …Labs … • • • • • • WBC Electrolytes ,Glucose , BUN & Creatinine ABG ( if hypoxia ) PPD ( if suspect TB ) 2 sets of Blood culture : (T < 95 or > 103 , Neutropenia, Severe CAP , Asplenic, Chronic liver disease , alcoholics, homeless ) Pleural Aspiration for pleural fluid > 1 cm on a lateral decubitus CXR • Sputum: ? CT ? Bronchoscopy ? Lung Biopsy ? Gram stain… and sputum culture Diagnosis ……Sputum ? • • • • • Not recommended for OP Low diagnostic yield in CAP Not cost effective positive reports can not separate Colonization from Infection Organism growing from sputum is not definitive proof that it is the etiologic agent. • Only 1/3 of the elderly can produce “ suitable “sample • • Gram stain: Needs Good quality sputum sample ( < 10 SEC /LPF Squamous epithelial cells, plus Neutrophils ) Most labs reject sputum with more than 10 SECs/LPF Difficult to get a good quality sample • • • • Rinsing mouth prior to expectoration No food for 2 hours prior to expectoration Immediate Inoculation into the culture media … Obtained Prior to antibiotic treatment ( Recommendation is < 6 hours ) • When to order “ Sputum “ • Pretreatment sputum is recommended for hospitalized patients … if performed on a good quality sputum with appropriate measures : If Patient … • Failed antibiotic therapy (either outpatients or hospitalized patients) • Cavitary lesions • Severe obstructive or structural lung disease e.g. Bronchiectasis • Pleural Effusion • Immune compromised • Active Alcohol Abuse • ICU patients • Suspected “ Drug Resistance Bacteria or Unusual Pathogens “ • Special stains of sputum for certain organisms when clinically indicated (e.g. Acid fast for mycobacteria, Direct fluorescent antibody for Pneumocystis ) Serology • Routine serological tests are NOT recommended because of the time required and the expense • Serology is necessary if : • Critically ill or non responders … • ‘ Pneumonia Outbreak ‘ with negative blood and sputum culture • Coxiella is suspected ( Q fever) or Pneumocystis • S Pneumoniae : Pneumococcal urine antigen is 80 % sensitive and > 90% specific, positive even after Abx use, and weeks after the illness… • Legionella Urine Antigen , sensitivity is 90% specificity is 99%, can be positive even after proper Abx, and weeks after the onset , use in patients with strongly suspected rapidly progressive legionellosis • Direct fluorescent antibody test for Influenza virus ‘Rapid Influenza Test’ • Sensitivity measures the actual positives (the percentage of people who are identified as having the condition). • Specificity measures the negatives (percentage of healthy people who are identified as NOT having the condition). Diagnosis: Serology • Mycoplasma Pneumoniae : Enzyme Immunoassay (EIA) sensitivity ~ 98 and specificity of 99.7 • Chlamydia Pneumoniae : Direct antigen testing and PCR. • C. Psittica : Complement fixation • Legionella :Urine antigen • Coxiella Burnetti : PCR and culture • Adenovirus : Culture and EIA • Para influenza & Influenza : Rapid diagnostic tests , PCR, EIA Differential Diagnosis • Pulmonary Embolism - most serious missed • • • • • • • Pulmonary Edema Bronchitis Exacerbation of COPD or heart failure Pulmonary Fibrosis Lung cancer Pneumonitis Sarcoidosis Other diagnostic tools • CT Scan : Should NOT be used routinely Indications: 1. Non responders 2. Helps identifies Cavitation 3. Loculated Pleural effusion • Thoracentesis : If a pleural effusion of > 1 cm the fluid should be aspirated • Bronchoscopy / BAL “ broncho-alveolar lavage ” • Lung Biopsy Decision For Hospitalization • Who can be safely treated at home ?? • Decision should be based on medical and social considerations • Q: Able to care for himself , able to take oral meds, Adherence ? • • • • • Preexisting condition, living conditions , cognition, vitals ,labs, CXR and physical findings Low risk > Home Moderate risk > Hospital High risk > ICU Most CAP cases are treated as an OP Hospitalization If Multiple risk factors have “ poor outcome ” RR 30 , BP < 90 / < 60 , Multilobar pneumonia , Confusion, BUN > 20 , PO2 <60 , PCO2 > 50 …Acidosis… Require oxygen , ivf , cardiac monitor or iv Abx , ?? severe cases TO assess pneumonia severity …there are Many Prediction Models... • PSI = Pneumonia severity index Pneumonia Outcome Research Team ( PORT ) Study • Prognostic Scoring Index • Mortality prediction rules , helps physicians guide the admission decision • classifies patients into one of 5 classes , points are calculated on factors such as age, sex, comorbidities, signs, labs , CXR • Mortality prediction rules classifies patients into one of 5 classes Points • • • • • Class 0 – 50 = I 51-70 = II 71-90 = III 91-130 = IV 131-395 = V Mortality 0.1 % Class I & II : Treat at Home 0.6% 0.9% Intermediate : (Individualized ) 9.3% 27% Class IV & V : Admit PORT : Pneumonia Outcome Research Team Prognostic Scoring Index Questions : Age , Sex , Nursing home Comorbidities : Cancer , Liver disease , CHF , CVA , CKD … Physical Exam : AMS , Pulse > 125 , RR > 30 , SBP < 90 , T < 95 or > 104 Labs : PH < 7.35 , BUN > 30 , Na < 130 , G > 250 , HCT < 30 , PO2 < 60 , O2 Sat < 90 % … CXR : Pleural effusion For each of variables add points , range is from 10-30 Points …Calculate Age for a man Age (in years) Age for a woman Age (in years) - 10 Nursing home resident +10 Coexisting illnesses Neoplastic disease (active) +30 Chronic liver disease +20 Heart failure +10 Cerebrovascular disease +10 Chronic renal disease +10 Physical examination findings Altered mental status +20 Respiratory rate ≥30/minute +20 Systolic blood pressure <90 mmHg +20 Temperature <35°C or ≥40°C +15 Pulse ≥125 beats/minute +10 Laboratory and radiographic findings Arterial pH <7.35 +30 Blood urea nitrogen ≥30 mg/dL (11 mmol/L) +20 Sodium <130 mmol/L +20 Glucose ≥250 mg/dL (14 mmol/L) +10 Hematocrit <30 percent +10 Partial pressure of arterial oxygen <60 mmHg* +10 Pleural effusion on chest x-ray +10 C U R B - 65 Another way to assess Pneumonia Severity C = Confusion U = Urea > 42 mg R = Respiratory rate ≥30/min B = Blood pressure ≤ 90 / ≤60 mmHg 65 = Age ≥ 65 years Score 0 or 1 can be treated as OP . Score of 2 …Admit . Patients with scores of ≥ 3 ICU. • Simplified C R B - 65 …one point for each For PCP Using clinical judgment without blood test if patient is 65 + and has one of these variable , then admission to hospital is reasonable Confusion , RR > 30 ,BP < 90 / < 60 These are Guidelines …Not Rules Use Clinical Judgment … No rule is absolute Treatment Supportive : Hydration, Oxygen, Analgesics, Antipyretics , IVF Empiric Therapy : (< 6 hours ) proven to reduce mortality . Empiric Therapy > 90 % respond very well Do NOT wait for diagnostics Guidelines for Empiric treatment are based on: Likely Pathogens , Severity , Comorbidities , Local susceptibility Location ( OP / Inpatient / ICU ) Modifying factors ( Cardio pulmonary disease or other factors ) Clinical Trials, Efficacy of agents , Safety Profile of Abx, Cost Risk factors for antimicrobial resistance : ( Age > 65 year , Abx past 3 months, Alcoholism, Immunosuppressed , exposure to child in a day-care center) What is proven to lower mortality ? 1. Antibiotic within 6 hours 2. Two Abx agents in Pneumococcal Pneumonia with bacteremia Beta Lactams : Penicillin's , Cephalosporin Gram Positive organisms. Monobactams (Aztreonam ) , Carbapenem ( Meropenom , Ertapenem ) Macrolides: ( Azithromycin , Clarithromycin , Erythromycin ) S Pneumoniae, H Influenzae, Mycoplasma, Legionella and Chlamydia …also covers Streptococci, staph, enterococci Quinolones : Moxifloxacin , Levaquin & Ciprofloxacin…. Once daily , Oral antibiotics ( or iv ) Covers Pneumococci, including drug resistance ( DRSP) , Gram negative and the atypical pathogens They penetrate very well into respiratory secretions . Highly bioavailable ~ 100 % the same serum level achieved with oral or iv therapy Recommended to give IV , to Ensure Absorption, once the patient shows response , change to oral therapy Anti Pneumococcal Quinolones : ( Respiratory ) Moxifloxacin and Levaquin Anti Pseudomonal Quinolone : ( Ciprofloxacin and Levaquin ) Although all anti pneumococcal quinolone are effective against pneumococci, they differ in their intrinsic activity against Pneumococci …on the basis of MIC they can be ranked …the most effective being Moxifloxacin , then Levaquin Empiric Abx for Outpatients Outpatient treatment in otherwise healthy , no recent Abx … • Azithromycin 500 mg / day or Doxycycline 100 mg bid Outpatient Tx for patients with comorbidities or who was on Abx last 3 m • Respiratory Fluoroquinolone (Moxifloxacin , Levaquin) Or Amoxicillin or Augmentin plus Macrolide ( Zithro ) ( Can substitute Doxycycline for Zithro ) Why ? Those Patients with Comorbidities failed Macrolides alone Tx because of (DRSP ) Outcome of Empiric Out Patient Treatment 90% will improve in 2 days ( Less Cough, Dyspnea, WBC ,Pain, and Fever ) 5% will slowly improve after 48 hours 5% will not improve in 2 days or feel worse , need to be reassessed … Therefore : patient need to be informed if after 72 hours , if they don’t improve , or develop fever 101, or are short of breath, hemoptysis , confusion or pleuritic chest pain …to come back to be checked ~ Half Of The 5 % experience progression and require hospital admission. The overall mortality rate for the outpatient group is < 1%. Excellent prognosis for the young, or otherwise healthy individuals Young healthy adults feel well enough to return to work in 4 or 5 days; almost all recover in 2 weeks Older patient & those with comorbidities can take few weeks to fully recover Pneumonia due to S . Pneumoniae and Influenza virus in the elderly with comorbidities can be fatal Empiric Inpatient Treatment (Not ICU) Treat for Drug resistance pneumococcal and Atypicals …Always with iv Abx • Monotherapy with a Respiratory Quinolone (Moxifloxacin , Levofloxacin ) or • Combination of β-lactam ( Rocephin, Augmentin ) plus ( Macrolide or Doxycycline ) . For patients with specific risk factor For Anaerobic infection (Aspiration pneumonia) Use Quinolone or Rocephin Plus Anaerobic coverage “ Clindamycin or Metronidazole or Zosyn or Timentin “ If Pseudomonas is a consideration Two Anti pseudomonal Agent ( Zosyn, Timentin, Meropenom , Cefepime) plus Anti pseudomonas Quinolone ( Ciprofloxacin or Levofloxacin ) Suspected concomitant Meningitis (? Pneumococcal) Vancomycin & Rocephin For Cavitary infiltrate or Empyema : Treat as MRSA (Vancomycin, Zyvox ) Bronchiectasis or ( COPD with Recent Abx & Steroids ): ( Treat For Pseudomonas, S Pneumonia & Legionella ) Allergy to penicillin : Maxipime =Ceftazidine 3rd gen ,or Fortaz =Cefepime 4th gen Legionella : Levaquin or Zithro Principles Of Antibiotic Therapy RECOMENDATION Based on / Evidence First Dose of Abx Within 6 Hours Observational Studies Treat all for possible Pneumococci and Atypical Observational Studies pt. age 65+ Macrolide Monotherapy for OP or IP with NO risk for DRSP or Gram Negative or Aspiration Randomized controlled trials For OP & IP with risk for DRSP or Gram Negative use 1. Macrolide & Oral Beta lactam or 2. Quinolone Monotherapy Randomized controlled trials & Observational Studies For OP at risk for DRSP the Oral Beta lactam should be (Cefuroxime, or high dose Ampicillin or Augmentin) In vitro susceptibility and expert opinion IP with risk for DRSP IV Beta lactam should be ( Rocephin, iv High dose Ampicillin or Augmentin ) In vitro susceptibility and expert recommendation Limit Anti pseudomonas to patient with Expert Opinion pseudomonas Risk factor ( to prevent resistance ) Limit Vancomycin use to empiric therapy of very severe illness ( meningitis ) to avoid overuse Expert Opinion Choose most active agent to minimize future resistance and best clinical benefit Expert Opinion Monitoring hospitalized patients Most Patients show clinical response in 1-3 days and stabilize in 3–7 . Vital signs, Temp , WBC , Symptoms & Clinical signs. Check sputum and blood culture results If done … adjust therapy Evaluation of Response to Therapy : Clinical improvement, relief of cough, sputum, dyspnea, improved appetite ,ability to take oral medications Normal Temp for 36 hours … WBC decline Normal functioning GI system …switch to highly bioavailable oral Abx Prepare to discharge if medically and socially stable Duration of Abx : 5 – 7 days for mild – moderate CAP If more serious ( MRSA , Pseudomonas or bacteremia) can take as long as ~ 3 weeks Radiological improvement lags behind clinical improvement Highest Mortality “ Pseudomonas followed by Klebsiella ,E coli, Staph Aureus “ Non Responders Patients Who Do Not Respond Within 72 Hours Of Appropriate Abx • Worsening or progressive clinical deterioration …needing ventilator Non responding , delay in clinical repose By day three if pneumonia patient does not improve , despite proper antibiotics, Reconsider the diagnosis … Does the patient has pulmonary embolism, or pulmonary edema or other … If this is an infection , is this an Unusual or virulent organism , Abx resistance,, coinfection, obstructive process, immune suppressed, TB or fungal infection or Cancer ? Workup for Non responders : Start all over … Retake the history, Recheck labs, reports of sputum, blood cultures, CXR , urine …Repeat CXR request CT if not done , Request Pulmonology consult ? Bronchoscopy and BAL to obtain microbiology and cytology , if pleural effusion Diagnostic Tapping …transfer to a higher level of care Risk factors for ( Non responding or treatment failure ) : Multilobar pneumonia ,Cavitation, pleural effusion, leucopenia, high PSI ,liver disease Protective factors : Prior pneumonia vaccine & Influenza vaccine, : using Quinolone Radiological Follow up • o o o • Every patients with pneumonia especially smokers > 40 should have a follow-up CXR after ~ 6 weeks to document resolution which may lag several weeks…behind clinical improvement Resolution Bacterial in 2-4 weeks Viral : 4 weeks + Mycoplasma : 6 weeks + Persistence of infiltrate after 6 weeks raises suspicious for Cancer or TB Up to 2% of hospitalized patients with CAP have Lung Cancer (with pneumonia distal to an obstructed bronchus) • 50% of these cancers are evident on the initial chest film. • The other 50% manifest as failure of pneumonia to resolve radiologicaly and are diagnosed at bronchoscopy … Complications Respiratory failure , Pleural effusion , Abscess, Empyema, Shock, Sepsis, CHF, MI, GI Bleed, Renal failure, Multi organ failure, Bleeding , Bacteremia which can lead to metastatic infection ( septic arthritis or meningitis ) in addition to worsening of already existing comorbidities • More than 60,000 people died in 2005 from CAP ‘ Poor prognostic factors include Elderly > 60 Multi-Lobar WBC < 5000 Comorbidities ( Alcoholics, CHF, Chronic Liver or Renal Disease , Immune Suppressed, Positive Blood Cultures) Pleural Effusion • Seen in ~ 40% of patients hospitalized for CAP mostly “ simple - Para pneumonic “ must differentiate it from empyema by sampling the fluid • Pneumococcal pneumonia is the infection most commonly complicated by pleural effusion , other pathogens ( H. Influenzae , Mycoplasma, Legionella and TB) • All patients with a pleural effusion should have a lateral decubitus CXR . If the effusion is > 1 cm in height, the fluid should be aspirated. If frank pus Chest tube … Thoracotomy and Decortication may be necessary. Lung abscess – Uncommon – Risk factors : Conditions associated with impaired cough reflex and/or aspiration, such as alcoholism, anesthesia, drug abuse, epilepsy, and CVA – Dental caries , Bronchiectasis ,Bronchial carcinoma and Pulmonary infarction • Etiology – Combination of Aerobic and Anaerobic Bacteria – Anaerobic bacteria ( Bacteroides ) – Aerobic ( Streptococcus milleri , Staph aureus , S. pneumoniae H. influenzae ,Pseudomonas aeruginosa ,E. coli , Klebsiella pneumoniae ) Recurrent pneumonia • Of patients hospitalized for CAP ~ 10–15 % have another episode within two years. • If the recurrence affects the same anatomic location as the previous episode, the most likely cause is an obstructed bronchus due to either a tumor or a foreign body. • CT of the Chest often detects pulmonary anatomic defects (e.g. Bronchiectasis ) that might be the cause of the recurrence. • COPD and repeated macro Aspiration are the most common causes of recurrent pneumonia. Prevention Influenza and Pneumococcal Vaccines … Protective ( when patient is afebrile , before discharge ) Yearly Influenza Vaccine : > 6 m and up Pneumococcal vaccine Q 5 years : Adults …65 + …Age 2-64 “ high risk “ with Chronic health problems ( Heart disease , lung disease , Sickle cell disease, Alcoholics, DM, Cirrhosis, Immune suppressed , HIV , Asplenics , Asthmatics , Hodgkin's, Lymphoma, organ transplant, Nephrotic ) ~ 50 % of adults Smoking Cessation Counseling • Avoid Abx for simple uncomplicated infection ( Sinusitis, URI, Bronchitis , Asymptomatic UTI ) • Avoid “ double “ antibiotic coverage • De- escalate Broad spectrum Abx • Short courses of Abx • • • No antibiotics for Single Positive Blood culture for Coagulase Negative Staph ( Common colonizer of skin ) The most serious pathogens (MRSA , Pseudomonas, Klebsiella, C diff and Multi Drug Resistance Bacteria ) are the product of our Antibiotic abuse 20 % of hospitalized patients in the US acquire Clostridium Difficile and about 30% of those develop C diff associated diarrhea ( mild self limiting to severe life threatening pseudomembranous colitis ) Health care Associated Pneumonia ( HCAP ) o Residence in a Nursing Home or other long-term care facility o Attend Hospital or Hemodialysis clinic within 30 days o Hospital Admission for two or more days within 90 days o IV Therapy, or IV Chemo , wound care, within 30 days Increased risk for 1. Multidrug-Resistant (MDR) pathogens 2. Poly Microbial • • Microbiology —Common pathogens include Aerobic Gram-negative Bacilli (e.g. E. Coli, Klebsiella , Enterobacter, Pseudomonas, Acinetobacter) and Grampositive Cocci ( Staph Aureus, including MRSA, Streptococcus ) Same increased risks with “ HAP / VAP “ Hospital acquired Pneumonia ( HAP) • Pneumonia that occurs 48 hours or more after admission • Highest risk is in patients on mechanical ventilation Sputum Gram stain and culture are indicated for all patients • Complicates up to 1% of hospitalizations • Mortality: 30-50% • Etiology of HAP differs … • CVA : Aspiration With Pneumoniae & Anaerobes • Ventilator : Pseudomonas , Gram negative Coliforms, Staph including MRSA • Organ Failure : Gram negative Coliforms • Airway Obstruction : Anaerobic • HIV and Chronic Steroid users : Fungi, Pneumocystis • Neutropenia < 500 : Candida and Aspergillus • Management: Antibiotics • Combination ( 2 – 3 antibiotics ) • Primaxin, Aminoglycoside, Meropenom , Clindamycin , add Vancomycin for MRSA or Zithro for Legionella • Antifungal • Resistance to Macrolides becoming more common • Decision for hospitalization should be based on medical and social considerations • If pneumonia does not respond think Pulmonary Embolism - most serious missed • Respiratory or Pulmonary Quinolones are (Levaquin & Moxifloxacin) • Cipro is a Gram Negative Abx • Antibiotics within 6 hours proven to lower mortality • Avoid Abx for simple uncomplicated infection ( Sinusitis, URI, Bronchitis …) Healthy Outpatients : Treat with Azithromycin or Doxycycline Outpatient with comorbidities or who was on Abx last 3 m Treat with Quinolone or ( Zithro ) plus (Amoxicillin or Augmentin )