WIN – Benefits Planning Basics - Oregon Supported Employment
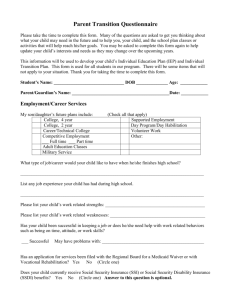
advertisement

OREGON’S WORK INCENTIVES NETWORK (WIN) When you work, you WIN! http://www.win-oregon.com This presentation is sponsored by The Oregon Competitive Employment Project, which is part of the Oregon State Department of Human Services, Office of Vocational Rehabilitation Services funded through a Medicaid Infrastructure Grant from the U.S. Centers for Medicare and Medicaid Services (CFDA #93.768). Updated April 2010 SOME BASIC TERMS YOU MIGHT NOT KNOW SSA: Social Security Administration SSI: Supplemental Security Income SSDI: Social Security Disability Insurance Office of Vocational Rehabilitation Services Other Federal & State Benefits Training Temporary Assistance to Needy Families (TANF) Supplemental Nutrition Assistance Program (SNAP) Housing Assistance (HUD) Unemployment Insurance Medicare Savings Programs (QMB) Low Income Subsidy (LIS) Medicaid (OHP or OHP+) Overview of Title II To be eligible for a T2 benefit based on disability: • Have insured status based on: • Own work record (SSDI) p. 19 • Parent’s work record (SSCDB) • Deceased spouse’s work record (SSDWB) • Meet SSA’s Definition of Disability: • A person must be determined to be medically disabled • Not be working or earning less than SGA THE BASICS: SSDI PAYMENT AND HEALTH CARE SYSTEM SSDI – Cash Benefit: Be disabled by SSA definition: and Be “insured” or draw off “insured” worker who is disabled, retired, deceased. Amount varies based on work history. No asset test. SSDI – Health Care: Medicare (after 24 month waiting period). Office of Vocational Rehabilitation Services Social Security Disability Insurance (SSDI) Reach Insured status based on your own work record: • 20 credits earned of all credits needed, at p. 19 least in the 10 years prior to onset of disability • Those disabled prior to age 31 need less to qualify • Possible to earn up to four credits per year • One credit = $1,120 for 2010 Childhood Disability Benefits To be eligible for Social Security as an adult child with a disability individuals must be: 18 years of age or older p. 20 Disabled by SSA’s definition before age 22; and, Child of an insured worker who are either disabled, retired or deceased. If child marries, benefits end unless marriage is to another Title II beneficiary Disabled Widow(er) Benefits To qualify a widow(er) must be found disabled before the end of a certain period: Month of a spouse’s death p. 20 Last month of entitlement to mother’s benefits 21 Last month of previous entitlement to DWB DWB are not payable prior to age 50 Must meet specific disability criteria Waiting period of five consecutive calendar months Title II Disability Check Amounts Check amount is based, in general, on amount paid in FICA taxes. Varies from person to person Total Family Benefit: Max amount all dependents can draw, split between number of dependents CDB/DWB: check amount is a % of the insured workers benefit. Varies as well. If Insured Worker is drawing a benefit check, their amount is not reduced/changed if CDB is being drawn. THE BASICS: SSI PAYMENT AND HEALTH CARE SYSTEM SSI - Cash Disabled by SSA definition; Little to no assets; under $2,000 for an individual, $3000 for a couple; Little to no income; and Benefit Amount for 2011 is $674, $1,011 for a couple, reduced by other income. SSI – Health Care Medicaid. Office of Vocational Rehabilitation Services The SSI Calculation Step Unearned Income General Income Exclusion (GIE) Countable Unearned Income Gross Earned Income Student Earned Income Exclusion Remainder GIE (if not used above) Remainder Earned Income Exclusion (EIE) Remainder Impairment Related Work Expense (IRWE) Remainder Divide by 2 Blind Work Expenses (BWE) Total Countable Earned Income Office of Vocational Rehabilitation Services Calculations = - Total Countable Unearned Income Total Countable Earned Income PASS Deduction Total Countable Income Base SSI Rate (check for VTR or PMV) Total Countable Income Adjusted SSI Payment + = - - = Total Income Unearned Income Adjusted SSI Wages TOTAL INCOME = Resource Test The SSI program has specific resource limitations set by statute and include real or personal property (including cash). Limits - $2,000 single / $3,000 couple p. 3334 Not subject to regular COLAs Limit cannot be exceeded at the beginning of each month Resources in excess will render individuals ineligible for SSI cash benefits Ineligibility will continue until resources fall below allowable limits Eligibility will cease if excess continues for 12 consecutive months Countable and Excluded Resources Countable: most assets are counted, such as Bank accounts, stocks/bonds, property you don’t live on Excluded Assets: there are a few assets that don’t count, such as The house you live in, a car you use for medical/work, special needs trust, Property Essential to Self Support (work incentive) Key: does person have access to it to pay for food and shelter SSI is the “2 to 1” Benefit Every $2 earned causes a $1 cash reduction SSDI is about phases and SSI is about a calculation SGA is not a consideration with SSI benefits Work Incentives keep more cash in a beneficiary’s pocket Many ways to stay connected to SSI and Medicaid if working Office of Vocational Rehabilitation Services Living Arrangements Must first determine household or non-household Primary household living arrangements: ◦ Non-institutional care ◦ Home ownership p. 29◦ Rental liability 31 ◦ Public assistance households ◦ Separate consumption ◦ Separate purchase of food for oneself ◦ Sharing ◦ Earmarked sharing Determinations are subject to SSA appeals process Medicare Coverage Five month waiting period from month of onset of disability for cash benefit Additional 24 month qualifying period for Medicare coverage Months needn’t be accumulated consecutively Months accumulated can be applied to subsequent case should entitlement cease due to SGA and entitlement be re-established If 24 months completed prior to losing entitlement and reestablished within 5 years (7 for CDB), 24 add. months not required Four Part Medicare Hospital Insurance / Part A financed through FICA pays for inpatient hospital care and certain follow-up p. 57 Medical Insurance / Part B pays for doctor’s services and variety of other medical services not covered under Part A voluntary and financed through monthly premiums paid by beneficiaries opting for coverage ($96.40) Four Part Medicare Managed Care / Part C Generally administered by HMO type health care agencies. Prescription Drug Coverage / Part D Provides prescription drug coverage for Medicare covered participants. Extended Medicare Coverage Extended coverage (Part A free) - a minimum of 93 months following the conclusion of the TWP Beneficiaries can buy into the Medicare program p. 59 once the extended Medicare coverage is exhausted. Medicaid may help pay Part A premium if under income threshold They must no longer be entitled to benefits because of having earnings above SGA and must have extended period of Medicare eligibility. Keeping Access to Medical Assistance A person with a disability who works in Oregon will very likely have access to medical benefits. Medicaid Continuation (1619b) Employed Persons with Disabilities Medicare Continuation Medicare for Persons with Disabilities Who Work Office of Vocational Rehabilitation Services Oregon’s Work Incentive Network (WIN) WIN is a benefits and work incentives planning service that helps people with disabilities: 1. 2. 3. MAKE INFORMED DECISIONS about work and their benefits; USE WORK INCENTIVES to achieve their employment goals; and NAVIGATE THE BENEFITS SYSTEMS when they begin working. Office of Vocational Rehabilitation Services Other Federal & State Benefits Training TANF SNAP Housing Assistance Unemployment Insurance Veteran’s Benefits Medicare Savings Programs Low Income Subsidy Medicaid Temporary Assistance to Needy Families Program Intent Provide cash assistance to needy families Case management Promote personal responsibility and accountability Reduce families living in poverty by promoting self sufficiency, employment & community resources PRE-TANF Program Intent Provide screenings, case management & cash assistance to needy families Holistic assessment; including the whole family, strengths, needs, goals Focus on family stability, employment and self sufficiency TANF Grant Amounts Typical grant amounts: 2 person = $448, income limit = $499 3 person = $528, income limit = $616 4 person = $647, income limit = $795 5 person = $747, income limit = $932 Examples above are maximum benefits based on 0 income. TANF and Employment Example: Family of 3, TANF countable income $616. They were receiving a full TANF grant of $528 based on 0 income. New job with earnings of $600 per month. Family is still below countable income of $616. When looking at income computer will calculate: Earned income at 50% reduction Grant of $528 - $300 = $228 new grant amount Supplemental Nutrition Assistance Program Basic Eligibility and Program Requirements SNAP The intent of the SNAP Program is to improve the health and well-being of eligible individuals by providing a means to meet the nutritional needs. Basic requirements Must have a valid Social Security Number Must be a US citizen or meet certain alien status requirements Must participate in the OFSET program Students must meet certain criteria Financial Eligibility Categorical eligibility 185% of the Federal Poverty Level Deductions Clients are responsible for: Reapplying for benefits and responding to Interim Change Reports Responding to requests for additional information from their worker Knowing their reporting requirements and reporting when required Housing Choice Vouchers (HCV): Provides tenant-based rental assistance in privately-owned units Tenants pay rent based on income Rental subsidy is paid by Housing Authority (HA) to landlord 32 Public Housing: Project-based rental assistance in housing units owned and managed by HA Tenants pay income-based or flat rent Housing authority performs repairs, annual inspections, collects rent, etc. 33 Public Housing vs. Vouchers Public Housing is owned and managed by the local public housing authority (PHA or HA). Housing Authority serves as the landlord. Subsidized housing or Housing Choice Vouchers (a.k.a. Section 8) is owned and operated by private owners, individuals, or landlords. Housing Authority is not the landlord HA provides rental subsidies to private owners/landlords Subsidy follows the tenant, not the property 34 Rental Developments Multifamily Housing (HUD) is where the subsidy is given to the owner, who provides affordable housing to low-income families. The housing subsidy stays with the property. Rural Development (USDA), similar to Multifamily Housing, subsidized rental assistance to low-income individuals and families in non-metropolitan settings 35 Participant Eligibility Must be a U.S citizen, national or non-citizen with eligible immigration status. Must meet the low-income guidelines as published by HUD. 36 Income Limits Income Limits: http://www.huduser.org/DATASETS/il.html 30% of the Median Very Low Income Low-Income 30% of the Median: 40% of all public housing admissions 75% of all housing choice voucher admissions 37 The Application Process Pre-application completed – income is calculated and eligibility determined Applicant is placed on waiting list Some HAs have wait list preferences, i.e., Homeless Current county/city resident Terminally ill Young and disabled (for Mainstream only) 38 The Application Process Initial Screening and background check—must deny applicants for certain crimes HAs may deny for other reasons Owing a HA money Committed fraud Income, assets, and deductions are verified by third party source 39 The Application Process Applicant reaches top of waiting list Applicant attends briefing/orientation Applicant receives a ‘voucher’, and housing search begins Applicant finds unit, landlord completes Request for Tenancy Approval form. 40 Unemployment Insurance Program Program Intent “Pay benefits promptly to claimants who are out of work through no fault of their own.” Office of Vocational Rehabilitation Services Eligibility for Unemployment Insurance There are three tests an individual must meet to qualify for unemployment insurance: Be unemployed as defined in state law, Qualify as a worker based on prior employment, and Be out of work through no fault of his/her own. Office of Vocational Rehabilitation Services Ways to Qualify for Unemployment Insurance There are two ways to qualify: Be paid at least $1,000 in wages from employment subject to UI law AND have total base year wages equal to or exceeding one and a half times the wages paid in the highest quarter of the base year, or Have some wages paid in the base year and perform at least 500 hours of work during the base year at employment subject to UI law. Office of Vocational Rehabilitation Services How Benefit Amounts are Determined The weekly benefit amount (WBA) is 1.25 percent of the wages paid during the base year from subject employment, within minimum and maximum amounts set by law. The minimum weekly benefit is $115 and the maximum weekly benefit is $492 for new claims filed effective June 28, 2009. Beginning with claims filed effective July 4, 2010 the minimum WBA will be $116 and the maximum $496. Benefit amounts for claims effective before July 4, 2010 will not change. Office of Vocational Rehabilitation Services Maximum Benefit Amount for UI The maximum benefit amount (MBA) is the total regular benefits a person can draw during the lifetime of the claim. For most people, the MBA is 26 times the weekly benefit amount. However, people who have very low base year wages qualify for the lesser of 26 times the weekly benefit amount or 1/3 of the total base year wages. Office of Vocational Rehabilitation Services Qualified Medicare Beneficiaries QMB provides additional medical coverage for Medicare recipients. When used alone, QMB refers to all QMB programs. Sometimes these programs are referred to as “Medicare Savings Programs”, or MSPs. The QMB programs are: QMB-BAS: Qualified Medicare Beneficiaries - Basic. The basic QMB program. QMB-SMB: Qualified Medicare Beneficiaries Special Medicare Beneficiary. QMB-SMF: SMB, Full federal reimbursement. SBI: State Buy-In. For Medicare Part A beneficiaries with countable incomes above 135% of the Federal Poverty Level. SBI is a case descriptor, not a program. More on this later. QMB benefits QMB-BAS: payment of Medicare Part A and Medicare Part B premiums, co-pays and deductibles. QMB-BAS is considered a medical benefit and recipients receive a medical card. QMB-SMB/SMF and SBI: payment of Medicare Part B premiums only. SMB, SMF, and SBI are not medical benefits. QMB Non-financial Eligibility Requirements To receive QMB or any of its subprograms, an individual must be receiving Medicare Part A. (OAR 461-135-0730) A person does not have to receive Medicare Part B benefits to be eligible for QMB benefits. Medicare Part D Prescription Drug Program and Low Income Subsidy (Extra Help) Prescription Drug Plan Beneficiaries enroll themselves through participating drug plan (PDP)… SSA does not process Part D enrollments Beneficiaries enroll during an enrollment period Participants must meet deductible, premium and copayment responsibilitioes Premium amount will vary from plan to plan Part D Participation voluntary CMS can assist a beneficiary in enrolling in a plan through its website http://www.medicare.gov Refer all questions regarding Part D coverage to 1-800-Medicare Beneficiaries can also get assistance selecting a plan through their State Health Insurance Counseling and Assistance Program (SHIP) Medicaid (OHP+) Eligibility for People with Disabilities Doors on the House of Medicaid Specifically for People with Disabilities 1. 2. 3. 4. 5. 6. 7. 8. SSI Former SSI Recipients:1619(b) Former SSI Recipients: DAC/CDBs Former SSI Recipients: Pickle Former SSI Recipients: DWB 300% Mental Health Non-Waivered Employed Persons with Disabilities Order of Use If eligible for SSI, 1619b, or any of the Former SSI Protected groups, those should be used first. There is no monthly premium/fee/liability If not eligible for those doors, determine most cost effective door to use 300% or EPD MH Non-Waivered or EPD Your Role 1. 2. Is NOT to determined eligibility Is to verify eligibility During comp intake ask a few questions about the person’s situation to be sure it matches the Medicaid group they are going under When verification comes back, check to make sure everything matches. If you find someone could be better off under a different group; contact case worker, pull in Medicaid Policy Analyst IT TAKES A TEAM TO REMOVE THIS BARRIER You can’t do your job AND be a Work Incentive Expert..….. BUT YOU CAN: 1. Let people know there are WORK INCENTIVES that support their employment efforts; 2. Recognize MYTHS and communicate FACTS; and 3. Encourage people to connect to WIN for more individualized analysis. Office of Vocational Rehabilitation Services QUESTIONS? CALL THE WIN STAFF IN YOUR AREA! Or for more information about WIN: http://www.win-oregon.com Office of Vocational Rehabilitation Services