The Evolving Role Of The Radiologist Assistant
advertisement

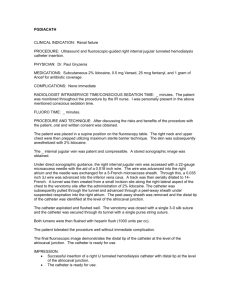
The Evolving Role of the Radiologist Assistant Richard Danieli Outline • • • • • • • • • • • • • • • • • • • • • • • • Introduction Radiology journey R.R.T. to R.A. Education as a Radiologist Assistant student Registered Radiologist Assistant (R.R.A.) Handbook ARRT RA education requirements Procedure List Mandatory procedures Elective procedures Competency requirements CR1 Forms CR2 Forms Summative Evaluations Board license eligibility Exam outline Career outlook Current legislation HR 3032 Medicare Access to Radiology Care Act Society of Radiology Physician Extenders Interesting Case studies Fibrin sheath port injection study Hiatal Hernia on UGI Loopogram obstruction TFC tear wrist arthrogram Questions and Answers Introduction • Clark F. Miller School of Radiologic Technology at Central Maine Medical Center • Central Maine Community College • Florida Hospital College of Health Science • Currently at Quinnipiac University Masters in Health Science Radiologist Assistant – 24 Month Full time: first year classroom, second year clinicals. Clinical placement: • • • • • Yale New Haven Hospital, CT. Fallon Clinic Worcester, MA. Baystate Medical Center Springfield , MA. Cooper Univerisity Hospital Camden, NJ. Uconn Medical Center Farmington, CT R.R.T. to R.A. • • R.R.T. license in every state for clinicals Advance Cardiac Life Support (ACLS) – Moderate/Conscious sedation – Response to a code/anaphylaxis/allergic reaction – Cardiac rhythyms • • Educational structure differences and the importance of good educators The bridge between Radiologist and Technologist – Technician difficulties and interpretation difficulties – logistics (PACS,RIS, proper orders etc…) • Responsibilities- need to recognize pathology – RT’s have Merrills. RA’s have….. Pathology, experience, Radiologist preferences. – IR-Coagulation factors • If you don’t know about it, you don’t look for it – Radiologist-4 years undergrad, 4 years medical school, 1 year surgery/ internal medicine internship, 4 years residency, 1 year fellowship= 14 years education – RA’s- 4 years undergrad, 2 years graduate school= 6 years education Q.U. Education Courses • Clinical Pharmacology I • Human Anatomy • Human Anatomy Lab • Imaging Pathophysiology • Radiation Safety and Health Physics • Image Critique & Pathologic Pattern Recognition I • Image Critique & Pathologic Pattern Recognition II • Interventional Procedures I • Interventional Procedures II • Patient Assessment, Management and Education • • • • • • • • • • Research Methods and Design Clinical Seminar I Clinical Seminar II Clinical Seminar III Radiologist Assistant Clinical I Radiologist Assistant Clinical II Radiologist Assistant Clinical III Radiologist Assistant Clinical IV Thesis I Thesis II • • • • • • • • • • • • • • • • • • GastroIntestinal and Chest Esophageal study must fluoro and image the esophagus, may be with UGI Swallow Function Study (participate in procedure and provide initial observations to radiologist Upper GI Study Small Bowel study- direct the study and spot TI Small bowel study via enteroclysis tube Enema with barium, air, or water soluble contrast Nasogastric/enteric and orogastric/enteric tube placement-may not require image guidance T-tube cholangiogram Defecography Perform chest fluoroscopy for diaphragmatic motion Genitourinary Antegrade urography through existing tube (e.g. pyelostography, nephrostography) Cystography or voiding cystourethrography, with minimum of 10 bladder catheterizations Retrograde urethrography or urethrocystography Loopography through existing tube Hysterosalpinography- imaging only Hysterosalpinography- procedure and image (physian participation required) • • • • • • • • • • • • • • • • • • • • • • • Invasive Nonvascular Arthrogram (radiography, CT, MR joint injection and aspirations) Lumbar Puncture Cervical, thoracic, or lumbar myelographyimaging only Lumbar Puncture with contrast Thoracentesis with or without catheter Placement of catheter for pneumothorax Paracentesis Abscess, fistula, sinus tract study Injection sentinel node localization Breast needle localization Change of percutaneous tube or drainage catheter Thyroid biopsy Liver biopsy Invasive Vascular Peripheral insertions of central venous catheter placement Insertion of non-tunneled central venous catheter Insertion of tunneled central venous catheter Port injection Extremity Venography Post processing Perform CT post processing Perform MR post processing Clinical Portfolio • The Clinical Portfolio consists of the following components: – (1) Clinical Experience Documentation and Clinical Competence Assessments – (2) Professional Activities and Accomplishments Record – (3) Case Studies – (4) Summative Evaluation Rating Scales. Form CR-1: Summary of Clinical Experience and Competence Assessments • 1. This form is completed by the student as he or she: (a) completes the requisite number of cases for the mandatory and elective procedures; and (b) is evaluated by a radiologist on the mandatory and elective procedures. • 2. The student records the number of cases completed for each mandatory and elective procedure he or she performs. • 3. The student records only the date that the competency assessment was completed. Note that the actual competence assessments are completed by a radiologist using Form CR-2 • 4. The preceptor and program director must verify and sign the bottom of Form CR-1. This form is submitted to ARRT at the time of application. Form CR-2: Clinical Competence Assessments (Forms CR-2A through CR-2E) • 1. These forms are completed by the radiologist at the time he or she evaluates the student. There are separate evaluation forms for each class of radiologic procedures: – Form CR-2A: GI/Chest Form CR-2C: invasive nonvascular – Form CR-2B: GU Form CR-2D: invasive vascular – Form CR-2E: post-processing activities • 2. The radiologist and student are required to sign the bottom of Form CR-2 for each assessment, which is subsequently reviewed and signed by the program director. • 3. The student must submit a minimum total of 15 assessment forms to ARRT (12 mandatory and 3 elective procedures). Summative Evaluation • The Summative Evaluation Rating Scales address five skill areas: – (1) evaluation of medical information – (2) patient communication – (3) radiation safety – (4) professionalism – (5) specific procedural skills R.R.A. Exam Board Eligibility • 1. ARRT Certified and Registered in Radiography • 2. One year of Acceptable Clinical Experience • 3. Educational Program Completion • 4. Didactic Competence Requirement R.R.A. Licensing Exam Board Eligibility • 5. Clinical Education Requirements – 5A. Component 1: Clinical Experience Documentation and Competence Assessments – 5B. Component 2: Professional Activities and Accomplishments Record – 5C. Component 3: Case Studies – 5D. Component 4: Summative Evaluation Rating Scales R.R.A. Licensing Exam Board Eligibility • 6. Baccalaureate Degree • 7. ARRT Ethics Requirements • 8. Application for Certification Registered Radiologist Assistant Examination Content Categories • Multiple Choice: – – – – – A.Patient Communication, Assessment, and Management- 45 points B. Drugs and Contrast Materials -30 points C. Anatomy, Physiology, and Pathophysiology- 55 points D. Radiologic Procedures- 40 points E. Radiation Safety, Radiation Biology, and Fluoroscopic Operation- 15 points – F. Medical-Legal, Professional, and Governmental Standards -15 points – Total Number- 200 points – Testing Time Allowed 3.5 hours • 2 Case Studies – Each case is followed by four to six essay questions worth 3 or 6 points each. – Testing Time Allowed 2.5 hours Career Outlook • Momentarily Difficult – New Profession, Myths, and Fears (lack of support) – Reimbursement issues (CMS Guidelines and supervision requirements) • R.R.A. roles beyond ARRT – Image interpretation ( think radiology residence) – Radiology Procedures not listed (bone marrow biopsy, IVC filter placement, drainage tube insertion, port removal, radiologist comfort etc…) – Liability • United kingdom – Advanced radiographer Practitioner • Quality of service provided – Clinical training of RA vs resident, PA, NP HR 1148 Medicare Access to Radiology Care Act of 2013 • To amend title XVIII of the Social Security Act to provide for payment for services of qualified radiologist assistants under the Medicare program. • More senator Co-sponsorship needed. Society of Radiology Physician Extenders • “The Society of Radiology Physician Extenders (SRPE) is a non-profit organization for the RPA and RRA sharing a common bond within the global mid-level radiology profession and medical community in general. The society holds an annual conference conducting seminars and presentations. The SRPE is an active participant with other health care professionals and organizations to educate and promote the role of the mid-level radiology extender. Our organization is committed to fostering the highest values and promoting superior lifelong success both personally and professionally.” – Conferences with Continuing Education Credits – Legislative involvement • http://www.srpeweb.org/DesktopDefault.aspx References • A.R.R.T (2013). Registered Radiologist Assistant (R.R.A.) | ARRT - The American Registry of Radiologic Technologists. Retrieved January 12, 2013, from https://www.arrt.org/Certification/RegisteredRadiologist-Assistant • S.R.P.E. (2013). Society of Radiology Physician Extenders Inc. Society of Radiology Physician Extenders Inc. Retrieved January 12, 2013, from http://www.srpeweb.org/DesktopDefault.aspx Richard Danieli 55 year old female Right breast grade 3 infiltrating ductal carcinoma Mammogram of Right Breast Breast Cancer Ultrasound of Right Breast Breast Cancer Left sided portacatheter placed 5/23/12 in good location and functional Portacatheter needed for chemothereapy treatment for cancer of the right breast Initial post port chest x-ray on 5/23/12 No blood return from port when accessed two days ago Left sided portacatheter placed to keep right side open for surgical and radiation options • • • • • • Portacatheter was accessed using sterile technique Patient was positioned supine on fluoroscopy table Scout spot x-ray obtained Patient was positioned in right anterior oblique 10 cc non ionic iodinated contrast was injected in the port Live fluoroscopy and rapid sequence imaging was obtained Scout fluoroscopy image 1 month post port placement Note: Loop in catheter Note: Distal location of catheter Malposition of the distal end of the portacatheter Loop in middle portion of portacatheter Fibrin sheath formation of distal portacatheter lumen Port Injection Image Note: contrast jetting superiorly and laterally from catheter. Extravasation of contrast through fracture or hole of catheter Migration of the catheter tip superiorly with a mid-portion loop is known complication especially with left sided ports due to the vessel pathway Fibrin sheath formation of the distal catheter lumen another known complication of portacatheters allowed a limited forward flush, but no blood aspiration Removal of current portacatheter Replace with a new portacatheter John: 1. What are the indications for a central venous port? 2. What are the indications for a left chest port placement? Stacy: 1. If a large symptomatic venous air embolism is caused, in what position do you place your patient? 2. What is the treatment for a large symptomatic venous air embolism? Tina: 1. What are the post op port placement instructions for patients? 2. Describe the details involved with using tissue plasminogen activator to treat fibrin sheaths or clots at the catheter tip. Kandarpa, K., & Machan, L. (2011). Handbook of interventional radiologic procedures (4th ed.). Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health. Kessel, D., Robertson, I., & Sabharwal, T. (2011). Interventional radiology: A survival guide (3rd ed.). Edinburgh: Churchill Libingstone/Elsevier. Kim, F. M., Burrows, P. E., Hoffer, F. A., & Chung, T. (1996). Interpreting the results of pediatric central venous catheter studies. Radiographics, 16, 747-754. Retrieved from http://radiographics.rsna.org/content/16/4/747.full.pdf+html. Mauro, M. (1998). Delayed complications of venous access. Techniques in Vascular and Interventional Radiology, 1(3), 158-167. doi:10.1016/S1089-2516(98)80145-5 . Slaby, J., & Navuluri, R. (2011). Chest Port Fracture Caused by Power Injection. Seminars in Interventional Radiology, 28(3), 357358. doi:10.1055/s-0031-1284463. Richard Danieli 77 year old female No known surgery to gastrointestinal tract No weight loss Dysphagia Pharyngeal perforation, aspiration, and fistula were not clinically indicated therefore thick and thin barium contrast was used and not water soluble contrast. The patient stated “food gets stuck in my throat” Other clinical reasons for performing an esophagram include: Dysphagia (difficulty swallowing) Odynophagia (painful swallowing) Globus (sensation of a lump in the throat) Suspected aspiration Postoperative assessment of laryngectomy Penetrating Trauma Endoscopy showed antral deformity follow up with GI study recommended Esophagram performed Thick and thin barium used in vertical and horizontal positions Patient positioned upright in right lateral, AP, and LPO Patient positioned supine in RAO, AP and RPO Images obtained of esophagus collapsed and dilated with barium Modifications of routine exam to image visualized pathology The chest x-ray shows the Hiatal Hernia. Notice the circumscribed lucency behind the heart. Notice the small Zenker’s diverticulm. Notice the distal esophageal diverticulum with barium distending distal esophagus Image obtained in upright position Notice distal esophageal diverticulum has barium pooling. In comparison to previous image there are tertiary contractions of the distal tortuous esophagus Image obtained in upright position stomach Notice the location of the diaphragm, clearly showing a Type IV complex paraesophageal hiatal hernia. Image obtained supine notice difference in appearance from prior images done upright showing or movement of the hernia Results:Multiple tertiary contractions of the esophagus are seen associated with prominence of the cricopharyngeus sphincter. 5mm in diameter Zenkers diverticulum is noted. No aspiration or penetration is seen. Large Hiatal hernia is seen with the majority of the stomach herniated into the chest cavity. There is considerable gastroesophageal reflux. A 2cm diameter outpouching is noted of the distal aspect of the esophagus compatible with distal esophageal diverticulum. Impression: Prominence of the cricopharyngeal sphincter associated with small Zenkers diverticulum. Significant motility dysfunction of the esophagus. Diverticulum of the distal esophagus as described. Large hiatal hernia. See above The differentials for the hiatal hernia on the frontal chest x-ray are: retrocardiac lung abscess retrocardiac empyema epiphrenic esophageal diverticulum There are no differentials for the esophagram images. They could potentially be wrongly diagnosed. The stomach could be wrongly diagnosed as a volvulus or malrotation if the interpreter did not notice the level of the diaphragm, but these diagnosis should be done on an UGI where the duodenum is visualized The zenckers diverticulum could be wrongly diagnosed as an ulcer The distal esophageal diverticulum could be wrongly diagnosed as a large ulcer Zenker’s diverticulum correlates with the sensation of food getting stuck in the upper esophagus Motility dysfunction which contributes to the patient’s dysphagia. Considerable gastroesophageal reflux (suspected treatment or forgot to mention symptoms) Asymptomatic distal esophageal diverticulum Asymptomatic type IV complex paraesophageal hiatal hernia Treatment for the reflux would be recommended such as Prilosec (an antacid). Surgery of hiatal hernia only necessary if hernia causes strangulation which cuts off the blood supply or causes an obstruction No treatment for asymptomatic type IV complex paraesophageal hiatal hernia No treatment for 77 year old asymptomatic distal esophageal diverticulum No treatment for the Zencker’s diverticulum No treatment for dysmotility Upper gastrointestinal barium study to visualize the stomach and duodenum could be done for further evaluation Small bowel follow through with barium could also be done to further evaluate potential areas of obstruction. CT with oral contrast of the abdomen and pelvis could be performed to further evaluate the anatomy John: Stacy: What are the four types of Hiatal Hernias? What are two properly named diapragmatic hernias? Discuss the indications and contraindications of using a barium tablet during an esophagram Discuss the indications and contraindication of administering effervescent granules Tina: Define a Zenker’s diverticulum Discuss another type of esophageal diverticulum Herring M.D., W. (2007). Recognizing Tumors, Tics, and Ulcers: Radiology of the Gastrointestinal Tract. In Learning Radiology Recognizing the Basics. (1st ed.). (pp. 181-196). Philadelphia, Pennsylvania: Mosby Elsevier. Houston M.D., J. D., & Davis M.D., M. D. (2001). Pharyngeal and Esophageal Examinations. In Fundamentals of Fluoroscopy. (1st ed.). (pp. 15-47). Philadelphia, Pennsylvania: W.B. Saunders Company. Mettler,JR., M.D., F. A. (2005). Gastrointestinal System. In Essentials of Radiology. (2nd ed.). (pp. 170-188). Philadelphia, Pennsylvania: Elsevier Saunders. Pretorius,M.D., E. S., Solomon,M.D., J. A., & Rubesin,M.D., S. E. (2011). Upper Gastrointestinal Tract. In Radiology Secrets Plus. (3rd ed.). (pp. 101-118). Philadelphia, Pennsylvania: Mosby Elsevier. Sandstrom,M.D., C. K., & Stern, M.D., E. J. (2011). Diaphragmatic Hernias: A Spectrum of Radiographic Appearances. Current Problems in Diagnostic Radiology, 40(3), 95-115. doi:http://dx.doi.org/10.1067/j.cpradiol.2009.11.001, Richard Danieli A 68 year old male with history of muscle invading bladder cancer. Post operative robotic assisted radical cystoprostatectomy Post operative ileal conduit urinary diversion performed History of bladder cancer Prior CT Filling defects in the dilated left renal pelvis Absence of contrast opacification of the left ureter, Recommend direct inspection of the left collecting system with cystoscopy and ureteroscopy. Interval worsening of the left hydroureteronephrosis. Anastomotic stricture at the junction between the ureter and ileal conduit cannot be excluded Recommendation from prior CT Evaluate Ileal Conduit Evaluate left ureter by retrograde contrast administration History of bladder cancer Obstructed proximal left ureter seen on prior CT 24-gauge Foley catheter inserted into stoma with 30 cc balloon inflated Conray-60 introduced into ileal conduit by gravity infusion Reflux into right ureter No contrast entered the left ureter despite various positional changes and delayed imaging. Patient vomited possibly due to relative over distention of the ileal bladder in attempts to induce left ureteral reflux Normal right upper urinary tract Normal ileal conduit contour No reflux into left ureter due to obstruction at the ureteroileal junction Note: No contrast in left ureter Catheter Right ureter Catheter balloon Ileal conduit Catheter Note: No contrast in left ureter Catheter balloon Right ureter Ileal conduit Right ureter Note: No contrast in left ureter Catheter balloon Catheter Ileal conduit IV contrast in right ureter IV contrast remained in left renal pelvis IV contrast in right ureter IV contrast remained in left renal pelvis No contrast extravasated therefore obstructed Ureteral obstruction post ileal conduit Improperly fashioned anastomosis Ischemia of the ureter with subsequent fibrosis and stricture Recurrent tumor in the ureter (rare) Infection or abscess formation with reaction Edema Calculus Sloughed papilla Adhesions or scarring. Torsion or compression at the sigmoid No extravasation of contrast outside of the ileal conduit or the right ureter Normal contour of ileal conduit and right ureter No contrast filling into the left ureter during the loopogram. Left ureter not evaluated from retrograde contrast administration via loopogram or antegrade contrast administration via CT Renal ultrasound Renal radionuclide studies, Percutaneous nephrogram/ureterogram Intravenous pyelogram (IVP) Abdomen/pelvis CT (with oral contrast, with and without IV contrast) John: 1. Where are post operative ileal conduit obstructions most common? 2. Besides obstruction, what is the other most common abnormality post operative ileal conduit surgery. Stacy: 1. Describe pseudoobstruction (conduit malfunction) and the cause. 2. What is a mucus plug in reference to a loopogram? Tina: 1. Describe two renal complications of an ileal conduit. 2. What risks are associated with an excessive length of an ileal conduit? Appleby, S., & Atala, A. (2010, September 2). Urostomy and Continent Urinary Diversion. National Kidney and Urologic Diseases Information Clearinghouse. Retrieved July 7, 2012, from http://kidney.niddk.nih.gov/kudiseases/pubs/urostomy/index.aspx Banner, M. P., Pollack, H. M., Bonavita, J. A., & Ellis, P. S. (1984). The radiology of urinary diversions. Radiographics, 4, 885-913. Retrieved from http://radiographics.rsna.org/content/4/6/885.full.pdf+html?sid=b58c27e0-59a3-40e3-bba639316da2f87d Fernbach, S., & Holland, E. (1988). Undiversion of the urinary tract: The pre-and postoperatie evaluation. Radiographics, 8, 213-233. Retrieved from http://radiographics.rsna.org/content/8/2/213.full.pdf+html?sid=b58c27e0-59a3-40e3-bba639316da2f87d Noble, J., Amin, Z., Kessel, D., & Rickards, D. (1994). Recurrent upper tract urothelial tumours: the use of loopography following cystectomy for bladder cancer. British Journal of Radiology, 67(803), 1057-1061. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/7820396 Thiruchelvam, N., Harrison, M., & Page, A. C. (2007). The double wire technique: an improved method for treating challending ureteroileal anastomotic strictures and occlusions. British Journal of Radiology, 80, 103-106. Retrieved from http://bjr.birjournals.org/content/80/950/103.long Rich Danieli 19 year old female continued right wrist discomfort for four months status post surgery for fracture of 5th metacarpal due to traumatic fall Patient continues to have pain with movement and therefore range of motion is slightly limited. An evaluation of patient and patients chart shows no contraindication for arthrogram or MRI (not pregnant, not claustrophobic, non-ferrous orthopedic hardware, no other metallic hardware, normal coagulations, no infection, and no known allergies. Bleeding Infection Contrast Reaction Joint Capsule Rupture. It assists and increases the ability to diagnose pathology within the wrist on the MRI. Do nothing MRI without gadolinium Arthogram without gadolinium and MRI Wrist arthroscopy. 20ml syringe Gadolinium mixture Injection site of the wrist 15ml saline 5ml isovue iodinated contrast 0.2ml of gadolinium. radioscaphoid joint Small patient and small joint only 2.5ml of Gad mixture was injected. Exercise wrist Final images obtained and recorded Send patient to MRI Artifact Gadolinium injected in the wrong area Delayed gadolinium injection time from MRI scan time homogenous structure composed of articular disc, the dorsal and volar radioulnar ligaments, the meniscus homologue, the ulnar collateral ligament, and the sheath of the extensor carpi ulnaris Arthrogram right wrist with contrast and gadolinium injection Partial sprain triangular fibrocartilage complex ligament at its attachment to the ulnar styloid Internal sprain triangular fibro cartilage. MRI right wrist with gadolinium Partial sprain TFC ligament at its attachment to the ulnar styloid Internal sprain triangular fibro cartilage. MRI right wrist with gadolinium Partial sprain TFC ligament at its attachment to the ulnar styloid Internal sprain Triangular fibro cartilage. No prior MRI available for comparison, intra-articular injection performed prior to patient’s arrival to the MRI center.. There is normal marrow signal in the distal radius and ulna, carpal bones and the base of the metacarpal bones. There is no eveidence of fracture or bone contusion. There is a partial tear of the triangular fibrocartilage ligament at it attachment to the ulnar styloid. There is a sprain of the scapholunate ligament. There is no evidence of vascular necrosis of the scaphoid. Surrounding soft tissue structures are unremarkable. There is no joint effusion. The median nerve has a proper signal characteristic in the caudal tunnel. There is no abnormal fluid collection. There is metal artifacts along the diaphysis of the fifth metacarpal. Posterior rotation of the distal ulna and a shallow ulnar notch of the distal radius suggesting distal radial ulnar instability. John What is the specific components of the patient’s orthopeadic hardware made of that make it compatible with MRI? What are the typical sequences used for an MRI of the wrist with Gadolinium? Tina What are the pros and cons of patient positioning when performing an MRI of the wrist between having the wrist above the head (superman position) or having the wrist by the patient’s side? If the patient was pregnant, what would have been the best diagnostic test to perform? Stacy What is a patient assessment test to check for triangular fibrocartilage complex injury and how is it performed? Was an MRI with Gadolinium necessary for this patient to determine her diagnosis? David W. Stoller, The wrist, Seminars in Roentgenology, Volume 30, Issue 3, July 1995, Pages 265-276, ISSN 0037-198X, 10.1016/S0037-198X(05)80015-X. Houston,MD, J., & Davis, MD, M. (2001). Musculoskeletal Examinations. In Fundamentals of Flouroscopy. (1st ed.). (pp. 135138). Philadelphia, PA: W.B. Saunders Company. Luis Cerezal, Faustino Abascal, Roberto García-Valtuille, Francisco del Piñal, Wrist MR Arthrography: How, Why, When, Radiologic Clinics of North America, Volume 43, Issue 4, July 2005, Pages 709-731, ISSN 0033-8389, 10.1016/j.rcl.2005.02.004. Robinson, P. (2005). MR imaging of the wrist. Current Orthopaedics, 19(3), 196-208. Usha Chundru, Geoffrey M. Riley, Lynne S. Steinbach, Magnetic Resonance Arthrography, Radiologic Clinics of North America, Volume 47, Issue 3, May 2009, Pages 471-494, ISSN 0033-8389, 10.1016/j.rcl.2009.02.001.