Santa Rosa City Schools Medication Training
advertisement

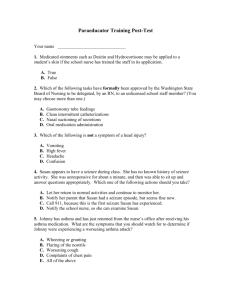
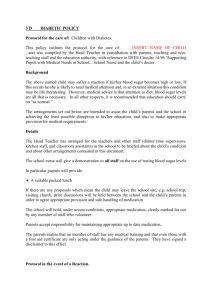
Thank you for all the juggling you do!!! Presented by District Nurses Cheryl Closser, RN, MSN, PHN Beth Munns, RN, BA, BSN Emily Henke, RN, BSN, PHN Jennifer Rodriguez, RN, BSN, PHN October 23rd and 24th 2014 Welcome and Introduction Health Tasks eSchools Confidentiality Medication Administration Nose Bleeds Head Injury Anaphylaxis Asthma Diabetes Vasovagal Syncope Heart Conditions/AED Seizures Immunizations Questions & concerns/evaluation Skills Laboratory CAIR Important Health Tasks Ensuring Confidentiality and Privacy Entering Health Information into eSchools Administering Medications Maintaining the Health Office First Aid Verifying and Reporting Immunization Data Ensuring Confidentiality Awareness of surroundings when speaking about students and any medical conditions. Keep paper work and files confidential; please do not post private information on walls. Do not allow student access. Please review emails before sending. Entering Information in eSchools Enter emergency card information ASAP! Do not drop information. Consistency of entry of health problems. Example: notes addressed to staff. Anaphylaxis vs. Allergies add your initials and date to med alert entry. Ask your nurse about any med alert doc. Questions. Notify staff of any urgent matters i.e. PE restrictions, MD Please Generate health problem list and distribute to appropriate staff. Example: food allergy list for kitchen. Notify nurse of any serious health conditions. Medication Administration Six Critical Rights Right Student Right Medication Right Dose Right Route Right Time Right Documentation Medication Administration Authorization Form Fill Out Completely Name of Student and Birth Date Signatures from parent and doctor with dates. 5 of 6 Rights must be on form Self administration or Self Carry? Important Considerations Changes must be in writing from the physician Notify School Nurse Immediately of Changes and New Medication Orders. Label and Order must match, notify your school nurse if they do not. Doctors orders must be brought into school by parent or faxed All medications this includes over the counter, supplements, herbs and alternative treatments must be in original container and be accompanied by a medication authorization form and/or doctor’s order. All doctors orders must be placed in health file, med book, with medication (disaster preparedness), & nurses mailbox Any problems or questions….contact your school nurse! Problems To protect yourself: if you find an incomplete order, document and date what you are doing to resolve the problem. Time Initials If student takes meds regularly, must mark reason for any missed dose For meds dropped or tossed away. Document on reverse side. Then also document the medication was given. Documentation Complete log in ink, with time, and your initials, when you assist or observe student using medication. Sign and initial bottom of medication log. If student takes meds regularly, document reason for any missed doses. You must have a list of the students who take medication at school All prescription medications must be counted and the number documented on the reverse side of the Medication Administration Record (MAR). Two adults count the number of pills (without touching them) and both adults sign for the medications that have been brought in. Call Nurse for Advice if needed Count pills when medication is dropped off Must be stored in centrally located, locked cabinet ALWAYS lock the med cabinet No student access to med cabinet Refrigerators for med storage must be locked & reserved only for meds! If you do not have a locking refrigerator (for medications only) at your school site, notify your site administrator. Errors and Discontinued Meds Report errors immediately: Site administrator School nurse Parent/ Guardian Document error on MAR Fill out incident report Discontinued/ Outdated Attempt to return When disposing of medication place in sharps container. Medication Error Sheet Please complete error sheet and give a copy to your school nurse and site administrator. If an incident report is required, attach med error sheet to report and give to administrator. Nurses will also complete reports as we check the medication binders and give a copy to the school’s administrators. Emergency Care Plan Forms Please give a copy of the forms i.e. Seizure Disorder, Diabetes, Anaphylaxis to parents and/or students with known diagnosis. Parents and physician must sign all care plan forms. Medication Book Organization A to Z by last name and include E Care Plans. Please use alphabetical file tabs. If you have a separate emergency plan binder a copy of the plan must also be placed in the medication binder. If you have a separate binder for diabetic students, have a reference in main binder. Make a list of students taking daily medication and place in front of binder. Staff Awareness Elementary schools may have a red binder in the staff room with care plans and physician notes; staff should look at. FYI: Teachers/staff should also have a red binder in their classroom for substitute teachers with emergency plans. This should also include a list of students with med alerts from eSchools. Teachers may ask you for this information. Field Trips Ask teachers to notify you 2 weeks in advance for field trips. Give them a copy of the medication administration form and the medication before the trip. Instruct teacher to document on back of form during the trip and assist with official documentation in med book on return. Maintaining the Health Office All equipment is functioning correctly Supplies are stocked, organized and accessible. Health office is clean, there should not be any food in the office. Example: Clean bed after every use. Ensure Emergency First Aid bag is ready to go, along with student medications, logs and ecards for disasters. First Aid Considerations Provide as much privacy as possible. Follow universal precautions. Document all visits to the Health Office (in pen) may use paper or computer log. Ensure 911 is called if situation warrants, and notify administration, parents and school nurse. Wash hands before and after first aid treatment Wear gloves when in contact with blood and other body fluids Call janitorial staff for clean up of excess bodily fluids Wipe down beds after each use, if blankets are used wash between uses. Keep health office area clear of food and beverages. FIRST AID - Sit upright, lean slightly forward. - Pinch soft part of nose above nostrils, 5-10 minutes, repeat if needed. - May use ice on bridge of nose if needed. - To prevent re-bleeding, advise students not to blow/pick nose or bend down for several hours. - If nosebleed lasts more than 20 minutes or follows an accident, fall or head injury don’t hesitate to call 911. What is a Concussion? A concussion is caused by a fall, bump, or blow to the head & can change the way your brain normally works. Head injuries must be taken seriously. May be difficult to determine whether mild or severe. Call parents and give head injury form with signs & symptoms and when to seek care. Severe symptoms usually develop within 24 hours but can occur several weeks later. Doctor’s note required for students to return after a concussion. Ice for head or neck Keep still in a darkened room, not alone Ask simple questions (what is your name, what day is today, where are you?) Observe body language, personality, balance Monitor student for worsening of symptoms, report to nurse and parent Re-evaluate student at 15 and 30 minutes Concussion Checklist http://www.cdc.gov/concussion/pdf/TBI_schools_che cklist_508-a.pdf Concussion: Heads Up For Schools (More information & free resources). Appears dazed, stunned, and/or confused Loses consciousness (even briefly) Memory, behavior or personality changes Balance problems or dizziness Double or blurry vision Headache and/or sensitivity to light or noise Feels tired, sluggish, hazy, foggy or groggy Nausea and/or vomiting Just not feeling right or feeling down Requires a hospital visit! Need doctor’s note to return to school. When is Head Injury a Medical Emergency? Call 911 if… Difficulty breathing Blood or clear fluid in the ears or nose One pupil larger than the other Loss of consciousness Mood changes Increasing confusion Loss of balance Worsening headache Drowsiness or cannot be awakened Weakness, numbness, and/or decreased coordination Speech problems Persistent vomiting or nausea Severe head/facial bleeding Unusual behavior Seizures If found unconscious assume the neck is injured and stabilize. DO NOT MOVE! Call 911. Stop any bleeding with pressure unless you suspect a skull fracture, no direct pressure. Open airway, watch for breathing. CPR if needed. Extremely serious form of an allergic reaction Can occur within seconds or be delayed. “Any respiratory system involvement, difficulty breathing, audible wheezing or difficulty swallowing”. -EMSA Definition Act immediately, You can save a student’s life! Anaphylaxis Emergency Care Plan See Handouts in English and Spanish: http://www.foodallergy.org/document.doc?id=234 http://www.foodallergy.org/document.doc?id=126 Please distribute copies of this plan to students/families whom have serious allergies. Nuts Shellfish Latex Bees Variety of Foods Some Chemical Exposures such as Sulfa Plants Other Unknowns What Kids Could Say: Look I have small red bumps My throat hurts I can’t swallow I can’t breathe I’m scared I’m dizzy I’m really itchy all over I feel like throwing up My stomach hurts My heart is beating really fast What You May See: Change of Voice Coughing Wheezing Change of Color Swelling of any body part Fainting or Loss of Consciousness What to do if Suspected Anaphylactic Reaction Determine if anaphylaxis is suspected. More of a danger not to give it than to give it. If symptoms have occurred CALL 911 immediately, stay with student. Have student sit and stay calm. Prepare to administer EpiPen. EpiPen acts immediately but effects last only 10-15 minutes. Make sure 911 is called. Two strengths: Above 66 lbs. = 0.3 mg (yellow) Below 66 lbs. = 0.15 mg (green) How to Administer Epi-Pen: Form a fist around the Epi-pen. Pull off the Safety Cap. Never put thumb, fingers, or hand over the black/orange tip. Swing and jab the tip firmly into the OUTER THIGH at a 90 degree angle. (Can be injected through clothing.) You will hear a click. Hold the EpiPen in place for 10 seconds. Remove & massage the injection area for several seconds. (After the injection, they may feel their heart pounding. This is a normal.) Check the black/orange tip: If the needle is exposed the dose was delivered, if not repeat above steps. Always Call 911: Give epi-pen first if alone, then call 911. Know time you gave Epi-pen, may only last 10-15 minutes. Do not give Benadryl first, takes 30-60 min. If symptoms return give 2nd Epi-pen 10-15 minutes after initial dose. If insect sting, remove stinger/apply ice to sting area. Scrape stinger out, do not pull out. Give used Epi-pen to paramedics Observe for signs of shock cover with blanket if cold. Watch breathing. If stops breathing begin CPR. Document the incident Send a copy to your school nurse School Personnel are required to have current CPR certification to administer an Epi-pen. Store at room temperature Keep record of expiration datesolution must be colorless, replace if brown Auvi Q Demonstration SEIZURE TRAINING FOR SCHOOL PERSONNEL Information from Epilepsy Foundation Discuss what a Seizure is. Review types/signs of Seizures. Seizure Triggers or Precipitants What to do during a Seizure. Recognize when a Seizure is a Medical Emergency. What is a Seizure? A brief, excessive discharge of electrical activity in the brain that alters one or more of the following: Movement Sensation Behavior Awareness Most Seizures are NOT medical Emergencies! Types and Signs of Seizures Generalized Seizures: (seizures involving the entire brain) *Tonic-Clonic (generally last 1 to 3 minutes, sudden, loss of consciousness, convulsions, stiffening and/or jerking of extremities) *Absence Seizures(generally last 1 to 10 seconds, lapse of awareness, blank stare, pause in activity) Partial Seizures: (seizures involving only part of the brain) *Simple/Complex Partial (awareness maintained and/or impaired, psychic/sensory symptoms, inability to respond) Seizure Triggers and Precipitants Flashing lights and hyperventilation can trigger seizures in some students with epilepsy Factors that might increase the likelihood of a seizure in students with epilepsy include: Missed or late medication (#1 reason) Stress/anxiety Lack of sleep/fatigue Hormonal changes Illness Alcohol or drug use Drug interactions (from prescribed or over the counter medicines) Overheating/overexertion Poor diet/missed meals What to do during a Seizure? Remain calm Time seizure Ensure safety Clear the area Cushion head, remove glasses Turn on side, loosen any tight clothing Nothing in mouth; don’t hold down Protect privacy After: reassure and stay with them When is a Seizure an Emergency? Call 911 When: Convulsive (tonic-clonic) seizure > 5 minutes Please refer to individual student health plan & consult with your nurse. Repeated seizures without regaining consciousness Injured or other medical condition First-time seizure Breathing difficulties Possible pregnancy Contact Information Epilepsy Foundation Information and Referral. (800) 332-1000 www.epilepsyfoundation.org What is Asthma? Asthma Triggers Allergens (mold, dust, pollen, animals etc.) Chemicals (sulfites, aspirin, etc.) Emotions (stress, crying, excitement) Exercise Irritants (perfume, cleaning fluids, smoke) Respiratory Infections (cold, flu, sinus) Seasonal/Time (day vs. night) Smoking Image Retrieved from:http://www.momscleanairforce.org/2013/05/20/asthma-cartoon Wheezing Frequent Cough Chest Tightness Shortness of Breath Difficulty Walking or Talking Check their Peak Flow Meter if they have one. Three Types: Please call nurse if unsure of the type of inhaler provided. 1. 2. 3. Rescue Maintenance Steroid Reversing Medication Rescue Inhaler Rescue Inhaler/Symptom Relieving: FOR SCHOOL Example: Albuterol/Ventolin/Pro Air HFA Maintenance Inhaler Maintenance/Preventative: Home Use Example: Advair, Q Var, Dulera No inflammation=no muscle irritation=no tightening of the breathing tubes. Steroid Flare Up Reversing Medication Example: Prednisone Symptom Relieving: Rapid Heart Rate Tremors Nervousness Headache 1. Help to sit upright; stay calm and reassure 2. Follow Emergency Action Plan &/or Doctors order for use of rescue inhaler 3. Get help from school nurse or notify parent if student has any of the following: • Inhaler not helping • Breathing hard and fast • Can’t walk or talk well 4. Call 911 if not breathing, unconscious, lips blue, struggling to breathe (hunched over or ribs show), or other signs of distress Notify Parent or Guardian Remove the cap and hold the inhaler upright. Shake the inhaler Tilt your head back slightly and breathe out. Press down on the inhaler to release the medicine as you start to breathe in slowly. Breathe in slowly for 3 to 5 seconds. Hold your breath for 10 seconds to allow medicine to go deeply into your lungs. Repeat puffs as directed. Wait 1 minute between puffs to allow the second puff to get into the lungs. Asthma Action Plan Please have parents and/or doctor complete the plan for students that have significant difficulty with their asthma. Vasovagal Syncope Student faints in response to trigger (sight of blood, heat, lack of food or water, fear of injury, standing for a long time, etc.) If a student loses consciousness call 911 Student should be checked by MD. especially if it is a first occurrence. If known history and student uninjured he/she should rest for 15 to 30 minutes. Heart Conditions and AEDs AED can save a child’s life that has a heart condition. AED awareness training annually at your school sites. AT least one person on site at all times that is CPR certified. Register at Coastal Valley EMS Place device in visible location for anyone to use. Monthly AED Readiness Check Date Functional(green light) Adult Padpak Exp date Ped Padpak Exp date Signature What is Diabetes? Body does not make or properly use insulin. Insulin is needed to: • Move glucose from blood into cells for energy If insulin isn’t working, high blood glucose results: • • • Energy levels are low Dehydration Complications Retrieved from: www.diabetes.org Type 1 Insulin dependent diabetes Insulin producing cells (pancreas) destroyed by body Must take insulin daily by injection or insulin pump. Type 2 Most common in adults. Pancreas can still make insulin. Diet, weight, lifestyle, and genetics causes. Early diagnosis controlled with medications at home. Signs and Symptoms of Diabetes Increased urination Increased thirst Increased tiredness Acanthosis Nigricans=dark pigmentation of skin around neck http://www.bing.com/images/search?q=nigricans+albicans&qpvt=nigricans+albicans&FORM=IGRE Medication/insulin Blood sugar monitoring Carbohydrate Counting Exercise 24/7 Job http://www.bing.com/images/search?q=juggling+type+1+diabetes&qs=n&form=QBIRMH&pq=juggling+type+1+diabetes&sc=0-12&sp=-1&sk= Diabetes Medical Management Plan Basis for all school-based diabetes care plans. Developed by student’s personal health care team and guardian. Signed by a member of student’s personal health care team. Individualized Basal dose is the background insulin that works for 24 hours Bolus dose is extra insulin given for carbohydrates Correction dose is used to decrease high blood sugar Ketones are acids produced by the body when it burns fat for fuel. Bad for diabetics. I:C is the insulin to carbohydrate ratio Insulin and Activity make blood sugar go down Food makes blood sugar go up Stress, illness, and injury affect blood sugar and it can go up or down. Many older students are independent! Some students will need school staff to observe or assist with care. All students with diabetes will need help in the event of an emergency situation. Always check the health plan Never leave student alone In Range (set by doctor) Administer insulin per plan Document Back to class Too high= Hyperglycemia Too low= Hypoglycemia Goal is to lower blood sugar within range Check blood glucose Allow use of the bathroom Allow access to water Insulin dose if stated in plan Check ketones if in plan Call home May NOT PLAY or DO PE if ketones present Ketones can lead to diabetic keto-acidosis emergency Develop over time, usually one high blood sugar is not a cause for an alarm. Pumpers can develop faster Time to check can vary based on health care plan. Always check if have Nausea Vomiting Abdominal Pain Flu like symptoms Two ways to check ketones; blood or urine Pee on a keto stick Any color on the stick is a call home Darker the color the more serious Dark and vomiting call 911 if unable to reach parent this can become very dangerous and serious Blood sugar too low – usually less than 80 Quick onset Requires immediate treatment May lead to unconsciousness if not Most students will be able to recognize the signs and symptoms of hypoglycemia but not always… Hypoglycemia Signs and Symptoms Mild Extreme Hunger Tremors Lethargic Increased heart rate Pale skin Sweating Change in Personality Shakiness Dizziness Headache Lethargic Dilated Pupils Clammy Skin Anxiety Moderate to Severe Yawning Irritability/frustration Behavior/personality changes Extreme tiredness/fatigue Sudden crying Restlessness Confusion Inability to swallow Dazed Appearance Seizures, convulsions Unconsciousness/coma jerking movements Blood sugar (BS) check If no meter, treat for a low with… Rule of 15 Student eats / drinks 15 grams of a fast acting carbohydrate • 4 oz. of juice • 3-4 glucose tablets • 1-2 TBSP honey • 6 oz. regular soda --NOT DIET SODA • 3 tsp. sugar in water Re-check BS in 10-15 min Repeat with 15 more grams if still low Recheck in 10-15 min If symptoms continue, call home Do Not Over Treat or allow student to over treat Student unable to swallow or unconscious Inject glucagon ASAP! Call 911 Position student on side will vomit Call parent or guardian and nurse Stay with the student Student should respond to the glucagon in 1020 minutes When student is awake and able to swallow give juice while waiting for EMS If student found unconscious assume low BS Naturally occurring pancreatic hormone It raises blood glucose level by releasing liver glycogen. Treatment for severe hypoglycemia. Can save a life! Cannot harm a student – cannot overdose. There are different doses, check the doctor’s order. 88 Place: As designated in DMMP accessible to school personnel. Store at room temperature Expiration date: Monitor After mixing, dispose of any unused portion within one hour. 89 1. Flip cap off glass vial containing dry powder 2. Remove cap from syringe 3. Put on gloves if available 90 4. Inject entire fluid in syringe into the bottle containing powder 5. Shake gently or roll to mix until all powder is dissolved and solution is clear. 91 6. Inspect. Solution should be clear and colorless. 7. Draw prescribed amount of glucagon back into syringe. 92 8. Clean site if possible. 9. Inject at 90° into the tissue under cleansed area (may administer through clothing as necessary buttocks thigh arm 93 10. 11. 12. 13. 14. 15. May take 10-20 minutes for student to regain consciousness Check blood glucose Give sips of fruit juice or regular soda, once student is awake and able to drink Advance diet as tolerated Document as per DMMP Do not recap syringe. Discard sharp in appropriate container 94 The time to complete recovery from a severe hypoglycemic episode varies according to how low the blood glucose level was and for how long prior to treatment Some signs and symptoms, such as headache, may persist for several hours, although the blood glucose level is satisfactory Continued monitoring is important Student may need to be transported via EMS or go home with parent/guardian 95 Student does not remember being unconscious, incoherent or has a headache Blood 200) glucose becomes very high (over Nausea or vomiting may occur 96 Glucagon Training Documentation Send copy to HR Keep a copy for your own records Diabetes Monitoring Log For the supervision of diabetic students at school. Let your nurse know if you have a student that requires supervision. Legal Considerations In the State of California unlicensed assistive personnel may administer insulin. Maintaining and Reporting Immunization Information Review immunization records and ensure requirements are met Shots for School Complete state reports for K and 7th grade Annually send report to Public Health Dept. for K and notify your nurse when complete. Send proof to Special Services. Notify nurse of any questions or concerns Immunization Guidelines Conditional vs Unconditional Admission 30 day grace period while waiting for records Waiver Forms Homeless may attend without immunizations. http://eziz.org/assets/docs/IMM-1080.pdf CAIR Please review form; add email and school Promise of CONFIDENTIALITY Password and User Name District Nurses to follow up CAIR web information Jrodriguez@srcs.k12.ca.us