Seronegative_Spondyloarthopathies
advertisement

Seronegative
Spondyloarthropathies
Goals of the Lecture
• Introduce the spondyloarthropathies
• Recognize AS as the prototypic disease
• Recognize common clinical and
radiologic features and specific features
including:
• Epidemiology
• Diagnosis
• Treatment
Seronegative
Spondyloarthropathies
Seronegative spondyloarthropathies
(SNSA):
A family of diseases
• Ankylosing Spondylitis
• Reiter’s syndrome/
Reactive arthritis
• IBD arthropathy
• Psoriatic arthropathy
(SNSA variant)
• Undifferentiated
spondyloarthropathy
• Juvenile onset SNSA
SNSA: Group characteristics
• Propensity to affect spine, peripheral
joints, and periarticular structures
• Characteristic extraarticular features
• Absence of RF and ANA
• Association with HLA B27
SNSA: Group pathology
• Sacroiliitis
– Osteopenia
– Erosions
• Peripheral arthritis
– Synovial hyperplasia
– Pannus
– Lymphoid infiltration
• Enthesitis
– Inflammation at tendinous
insertions
Causes of sacroiliitis
• Seronegatives
–
–
–
–
–
–
–
AS
Reiter’s
Psoriatic arthritis
IBD
SAPHO
Acne-associated
Intestinal bypass
• Infections
–
–
–
–
Pyogenic infections
Tuberculosis
Brucellosis
Whipple’s
• Others
– Paraplegia
– Sarcoidosis
– Hyperparathyroidism
Ankylosing spondylitis:
Prototype SNSA
• Systemic inflammatory
– Sacroiliitis is hallmark
• X-ray evidence needed for original and modified
NY criteria
– Clinical spectrum wider than symptomatic
sacroiliitis
– Atypical
AS: Diagnosis
• Diagnostic Criteria
– Highly sensitive at early stage of disease
• Classification Criteria
– Deals with groups of patients
– NOT individual patients
– Primarily for epidemiologic purposes
Grading sacroiliitis
• Grading of radiographs
Normal
0
Suspicious
1
Minimal sacroiliitis
2
Moderate sacroiliitis 3
Ankylosis
4
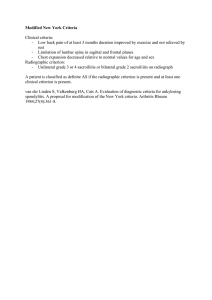
Ankylosing spondylitis
(Modified New York classification criteria)
1. LBP at rest for >3 months
• improved with exercise
• not relieved by rest
2.
3.
4.
5.
Limitation of lumbar spine
Decreased chest expansion
Bilateral sacroiliitis grade 2-4
Unilateral sacroiliitis grade 3-4
Definite AS if criterion 4 and any other criteria is fulfilled
Ankylosing spondylitis:
Clinical features
• Onset in late adolescence/ early
adulthood
• After age 45 is uncommon
• Much more common in men
• M:F 3:1
• Clinical/xray features evolve more slowly in
women
• Skeletal vs. extraskeletal features
AS :Skeletal features
• Axial (back pain)
– sacroiliitis
– spondylitis
•
•
•
•
Hips/shoulders
Enthesitis
Osteoporosis
Spinal fractures
Ankylosing spondylitis
vs. mechanical LBP
• Inflammatory/
spondylitic back pain
1. Onset prior to age 40
2. Insidious onset
3. Persistence at least 3
months
4. Morning stiffness
5. Improvement with
exercise
Need 4/5 criteria
Inflammatory questions
– Sensitivity 95-100%
– False + 10-15%
• mechanical back pain
and healthy athletes
• low prevalence of AS in
population (1-2%)
– Positive predictive value
is low
• 10% false positive
AS: Peripheral
skeletal features
• Hip and shoulder
involvement
– May be first symptom
– Up to 1/3 patients
– More common in
juvenile (<16) onset
– Flexion contractures at
hips
AS: Peripheral skeletal features
• Other peripheral
joints
– Infrequent
– Often asymmetric
– Transient
– Rarely erosive
– Resolves without
residual deformity
AS: Enthesitis
• Enthesitis
– Extra-articular or juxta-articular
bony pain
•
•
•
•
•
•
•
•
•
•
Costosternal junctions
Spinous processes
Iliac crests
Greater trochanters
Ischial tuberosities
Tibial tubercles
Achilles tendon insertions
Plantar fascia insertion
Pes anserinus
Epicondylus humeri lateralis
Extraskeletal manifestations
• A ortic insufficiency and other cardiac pathology
• N eurologic (atlantoaxial subluxation, Cauda equina)
• K idney (secondary amyloidosis, chronic prostatitis)
•
•
•
•
•
S pine (cervical fracture, spinal stenosis)
P ulmonary (apical lobe fibrosis, restrictive disease)
O cular (anterior uveitis)
N ephropathy (IgA)
D iscitis
AS: Extraskeletal manifestations
• Eye- acute anterior uveitis (25-30%)
• Heart- ascending aortitis, AR (3-10%),
conduction abnormalities (3%)
• Pulmonary- apical fibrosis (rare)
• Neurologic- fracture/dislocation.
subluxations, cauda equina syndrome
AS: Iritis
• Acute anterior uveitis/iritis/
iridocyclitis
• Most common ES
• 25-30%
• Unilateral
• Recurrent
• Symptoms
•
•
•
•
Pain
Lacrimation
Photophobia
Blurry vision
AS: Physical examination
• Limited range of motion (especially
hyperextension, lateral flexion, or
rotation)
• Spasm/soreness of paraspinal muscles
• Positive Schober’s test
• Loss of lumbar lordosis
• Sacroiliac discomfort
Patrick’s and Gaenslen’s tests
Office measurement
Wiki
• The Dimples of Venus (also known as booty dimples, back
dimples, or butt dimples) are sagittally symmetrical indentations
sometimes visible on the human lower back, just superior to the
gluteal cleft. They are directly superficial to the two sacroiliac
joints, the sites where the sacrum attaches to the ilium of the
pelvis.
• The term "Dimples of Venus", while informal, is an historically
accepted name within the medical profession for the superficial
topography of the sacroiliac joints. The Latin name is fossae
lumbales laterales ('lateral lumbar indentations'). These
indentations are created by a short ligament stretching between the
posterior superior iliac spine and the skin.
• Booty dimples are rapidly gaining cultural momentum as a feature
men find attractive in women and other men.
Wiki
•
•
•
•
The dimples of Venus (also known as back dimples) are sagittally symmetrical
indentations sometimes visible on the human lower back, just superior to the gluteal
cleft. They are directly superficial to the two sacroiliac joints, the sites where the sacrum
attaches to the ilium of the pelvis.
The term "dimples of Venus", while informal, is a historically accepted name within the
medical profession for the superficial topography of the sacroiliac joints. The Latin
name is fossae lumbales laterales ("lateral lumbar indentations"). These indentations are
created by a short ligament stretching between the posterior superior iliac spine and the
skin. They are thought to be genetic.
There are other deep-to-superficial skin ligaments, such as "Cooper's ligaments", which
are present in the breast and are found between the pectoralis major fascia and the skin.
There is another use for the term "Dimple of Venus" in surgical anatomy. These are two
symmetrical indentations on the posterior aspect of sacrum which contain a venous
channel too. They are used as a landmark for finding the superior articular facets of the
sacrum as a guide to place sacral pedicle screws in spine surgery[1].
1="Vertebra prominens"
Spinous process of C7
2= 2nd Lumbar vertebra
3= L4-5 inter vertebral
space
4= Iliac crests
5= Dimples of Venus /
Sacroiliac joints / Booty
Dimples
Office measurement
Don’t Be Fooled!
AS: Laboratory findings
•
•
•
•
•
•
Elevated ESR (75%)
Elevated CRP
ANA and RF negative
NC/NC anemia (15%)
HLA B27
No diagnostic or pathognomic tests!
HLA-B27: Disease Associations
Disease
Association
Ankylosing spondylitis
Reiter’s syndrome
Reactive arthritis
Inflammatory bowel disease
Psoriatic arthritis- spondylitis
- peripheral arthritis
Whipple’s disease
>90%
80%
85%
50%
50%
15%
30%
HLA B27 and AS in Caucasian
populations
•
•
•
•
•
HLA B27 in Americans
HLA B27 in African Americans
HLA B27 in AS patients
Prevalence of AS in population
Prevalence of AS in HLA B27+
individuals
• Prevalence of AS in B27+ relatives
• Prevalence of AS in B27- relatives
8-14%
3%
>90%
1%
2%
20%
0%
AS: Radiologic features
• Sacroiliac
– Bilateral, symmetric involvement (i.e.
erosions, sclerosis, pseudowidening,
ossification)
• Spine
– “Shiny corners”, squaring of the vertebra,
ossification of the annulus fibrosus,
ankylosis
• Hip
– Symmetric concentric joint narrowing
AS: Radiographic findings
• SI joint- symmetric
– Pronounced on iliac
side
• Erosions/sclerosis
– ‘Postage stamp’
serrations
– Pseudowidening
www.mdconsult.com/das/book/0/view/1807/I4-u1....
More sensitive than XRAY
• MRI
• CT
Late sacroiliac changes
• Calcification,
interosseous
bridging, and
ossification
• Bony ankylosis
• Osteoporosis
AS
Radiographic findings
• Vertebral
Column
– Squaring of
vertebrae
Skeletal manifestations
• Syndesmophytes
– Ossification of the
outer layers of
the annulus
fibrosis
– Sharpey’s fibers
– Vertical
Osteophyte Vs. Syndesmophyte
Late axial disease
B
A
M
B
O
O
AS: Radiographic findings
• Enthesitis
– Bony erosions
– Osteitis (whiskering) of
insertions
• Ischial tuberosities
• Iliac crest
• Calcani
• Femoral trochanters
• Spinous processes
AS: Treatment
• Main objectives
– Patient education
– Early diagnosis
– Control pain and suppress inflammation
– Daily exercises
– Surgical measures (i.e. hip arthroplasty)
– Vocational support
AS:Treatment
• NSAIDs- pain and stiffness
• Sulfasalazine/MTX- peripheral
arthritis
• Anti-TNF agents- axial and peripheral
disease
• Oral corticosteroids- little role
• Local corticosteroids- recalcitrant
enthesopathy
Etanercept in AS
(% ASAS Response Week 12)
Davis J, et al, Arthritis Rheumatism 2003
100
90
80
70
60
Placebo (n=138)
Etanercept (n=139)
50
40
30
20
10
0
ASAS 20
ASAS 50
ASAS 70
Infliximab in AS
(% ASAS Response at 24 weeks)
van der Heijde D, et al, Arthritis Rheumatism 2005
100
90
80
70
60
50
40
30
20
10
0
placebo (n=78)
Infliximab (n=201)
ASAS 20
ASAS 40
AS: Summary
Age at onset
Sex ratio
Axial disease
Sacroiliitis
Peripheral joint
Eye involvement
Infectious triggers
Young adults
3:1 (males to females)
Virtually 100%
Symmetric
25%
25%
Unknown
Case scenario 1
• 35 year old male
• 6 months of low back
stiffness and pain
– Improves with exercise
• Painful swelling at
Achilles insertion
• Urethral discharge prior
to symptoms
Physical Exam
Reactive arthritis: Clinical triad
1. Conjunctivitis
2. Urethritis/cervicitis
3. Arthritis
Reactive arthritis: Epidemiology
• Incidence
– Postdysenteric: 9/602 sailors
– Olmsted county, MN: 3.5 cases/100,000
• Age of onset
– 20-30s (5-80)
• Gender
– 5:1 male to female
– Postvenereal (males >> females)
– Postdysenteric (males=females)
Reactive arthritis: Joint disease
• Onset 1-4 weeks after exposure
• Asymmetric, additive, and ascending
oligoarthritis
• Lower extremity typical
• Dactylitis (“sausage digits”)
• Axial symptoms at onset (50%)
Reactive arthritis: Clinical
features
• Ocular
– Uveitis, conjunctivitis,
keratitis
• Mucocutaneous
– Oral ulcerations, circinate
balanitis, keratoderma
• Others
– Fevers, cardiac (AR,
conduction
abnormalities)
Reactive arthritis: Triggers
• Enteric pathogens
– Shigella flexneri
– Salmonella
typhimurium
– Yersinia
enterocolitica
– Campylobacter jejuni
• Urogenital
pathogens
– Chlamydia
trachomatis
– Ureaplasma
urealyticum
Reactive arthritis: Labs
• Elevated ESR and CRP
• Thrombocytosis, NC/NC anemia
• Remember HIV
• ALL ARE NON-SPECIFIC
Reactive arthritis: Therapy
•
•
•
•
•
•
NSAIDs
Long acting indomethacin
Systemic glucocorticoids
DMARDs
TNF blockers
Prolonged antibiotics ??
Reactive arthritis: Summary
Age at onset
Sex ratio
Axial disease
Symmetry
Peripheral joints
Eye involvement
Skin/nail findings
Young adults
Mostly male
50%
Asymmetric
>90%
Common
Common
Case scenario 2
• 45 year old male
• 6 months of low back
stiffness and pain
– Improves with exercise
• New rash on elbows and
knees
• Tender, swollen fingers
and toes
Psoriatic arthritis (PSA)
Five types
1. Oligoarticular (>50%)
2.
3.
4.
5.
RA variant (25%)
DIP only (5-10%)
Arthritis mutilans (5%)
Back disease (20-40%)
Psoriatic arthritis (PSA):
Radiology
• Fusiform
• Normal
mineralization
• Joint space loss
• Pencil in cup
• Bone proliferation
Psoriatic arthritis: Summary
Age at onset
Sex ratio
Axial disease
Symmetry
Peripheral joint
Eye involvement
Skin/nail disease
Young adults
Equal
20%
Asymmetric
95%
Occasional
Virtually 100%
Case scenario 3
• 35 year old male
• 6 months of low back
stiffness and pain
– Improves with exercise
• New onset diarrhea
• Painful sores on shins
Inflammatory bowel disease:
Relationship to bowel symptoms
• Bowel symptoms precede or coincide
with joint symptoms in vast majority
• BUT, in 5-10% joints symptoms
preceded bowel disease
• In UC, removal of colon usually
eliminates peripheral disease
Inflammatory bowel disease:
Axial disease
• Prevalence
– Sacroiliitis 10-20%
– Spondylitis 7-12%
• Female to male ratio: 1:1
• Onset of axial involvement does not
correlate with IBD
• Removal of bowel does not affect axial
disease
Inflammatory bowel disease:
Peripheral arthritis
• Prevalence: 17-20% (higher in
Crohn’s)
• Pattern: Pauciarticular, asymmetric,
frequently transient
• Joints involved: Large lower extremity
joints (usually not destructive)
• Soft tissue: enthesopathy, clubbing,
sausage digits
IBD: Summary
Age of onset
Sex ratio
Axial disease
Symmetry
Peripheral joints
Eye involvement
Skin/nail findings
Young adults
Equal
<20%
Symmetric
Frequent
Occasional
Uncommon