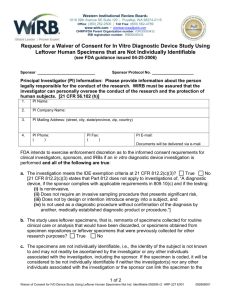
Waiver of Consent for In Vitro Diagnostic Device Worksheet
advertisement

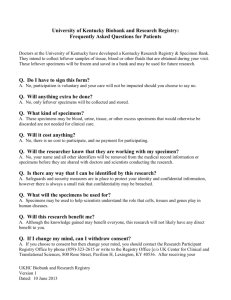
Request for a Waiver of Consent for In Vitro Diagnostic Device Study Using Leftover Human Specimens that are Not Individually Identifiable Worksheet Per the FDA, “In vitro diagnostic products are those reagents, instruments, and systems intended for use in diagnosis of disease or other conditions,” using specimens obtained from the human body. Examples include: assays, genetic tests, and reagents (including antibodies and other biological reagents). In vitro diagnostic products are medical devices per the FDA regulations. Thus, the FDA medical device regulations apply to you if you are using an in-vitro diagnostic device in a research study, and that device is not FDA-approved for the indication described in the research protocol. Specifically: The FDA generally requires that informed consent be obtained for all FDA-regulated human subject research. The FDA also defines human subjects to include human specimens used to test medical devices. However, FDA has stated that they will use “enforcement discretion” for this consent requirement in some cases, when the samples are complete deidentified and other conditions are met. The purpose of this worksheet is to establish and document that your study meets the criteria for “enforcement discretion” for informed consent per the FDA Guidance. Please upload this form in the Informed Consent Process section of the eIRB Smartform, under Question 14. IRB number: PI Name: Study Title: Investigator completing this form: Q1. Is the device an In Vitro Diagnostic device (IVD) that meets all of the following criteria? Indicate if the following criteria apply: ☐ A. The device is properly labeled in accordance with 21 CFR 809.10(c). (Researchers should consult with manufacturer/study supporter for documentation) ☐ B. The testing is noninvasive. (select the nature of the testing) ☐ Blood sampling that involves simple venipuncture ☐ Use of surplus samples of body fluids or tissues that are left over from samples taken for noninvestigational purposes ☐ Does not, by design or intention: a) penetrate or pierce the skin or mucous membranes of the body, the ocular cavity, or the urethra; or b) enter the ear beyond the external auditory canal, the nose beyond the nares, the mouth beyond the pharynx, the anal canal beyond the rectum, or the vagina beyond the cervical os. ☐ C. The testing does not require an invasive sampling procedure that presents significant risk. (i.e. require biopsy of a major organ, use of general anesthesia, or placement of a blood access line into an artery or large vein) ☐ D. The testing does not by design or intention introduce energy into a subject. ☐ E. The testing is not used as a diagnostic procedure without confirmation of the diagnosis by another, medically established diagnostic product or procedure. Specify medically established diagnostic product or procedure to be used: *If Q1 criteria do apply, move on to following questions. Otherwise, informed consent is required for this study. IRB version date 10/27/2015 Q2: Does the study use leftover specimens?1 ☐ No. (If no, informed consent is required) ☐ Yes. Please explain where/how the specimens were collected: Q3: Is the amount of specimen needed for the study more than would be leftover from what is usually collected for routine clinical analysis? ☐ No. ☐ Yes. (If yes, informed consent is required) Q4: Will the investigators, co-investigators, or sponsors have access to identifiable information and/or links or codes which would allow identification of subjects?2 ☐ No. Please explain how specimens will be provided to the investigators, how specimens will deidentifed or coded prior to being supplied to the investigators: ☐ Yes. (If yes, informed consent is required) Q5: Will specimens be accompanied by clinical information? ☐ No. ☐ Yes. Please explain how the study team will ensure that the information will not make the specimens identifiable to the investigator or any other individual associated with the research, including the sponsor, if any (refer to list of 18 HIPAA identifiers here: www.irb.emory.edu/documents/phi_identifiers.pdf): Q6. Will any individuals providing health care for the donors of the specimens share information about the donors/subjects with the research team? ☐ No. ☐ Yes. (If yes, informed consent is required) Q7. If specimens come from an external supplier: Are the specimens provided to the investigator(s) without identifiers and the supplier of the specimens has established policies and procedures to prevent the release of personal information? ☐ No. ☐ Yes. Please provide (if available) the sponsor's documentation of the policies and procedures followed by the specimen provider to ensure that the subject cannot be identified. ☐ N/A. Q8: Will the test results be reported to the subject’s health care provider? ☐ No. ☐ Yes. (If yes, informed consent is required) Thank you! The IRB member(s) will include this information in their review of the research protocol. 1 Leftover specimens are remnants of specimens collected for routine clinical care or analysis that would have been discarded. The study may also use specimens obtained from specimen repositories or leftover specimens that were previously collected for other research purposes. 2 Not individually identifiable means that the identity of the subject is not known to and may not readily be ascertained by the investigator or any other individuals associated with the research, including the sponsor. If the specimen is coded, it will be considered to be not individually identifiable if neither the investigator(s) nor any other individuals associated with the investigation or the sponsor can link the specimen to the subject from whom the specimen was collected, either directly or indirectly through coding systems. specimen to the subject from whom the specimen was collected, either directly or indirectly through coding systems. IRB version date 10/27/2015